And while using OCTs, lasers, and light-emitting devices does not require knowledge of the underlying mechanics, like driving a car, appreciating the technology behind these devices offers deeper insight into ocular disease and adds credibility when discussing findings with colleagues and patients.
This article provides the essential knowledge about the electromagnetic energy of the universe and its relevance to the ocular applications and procedures that optometrists employ every day.
Electromagnetic radiation
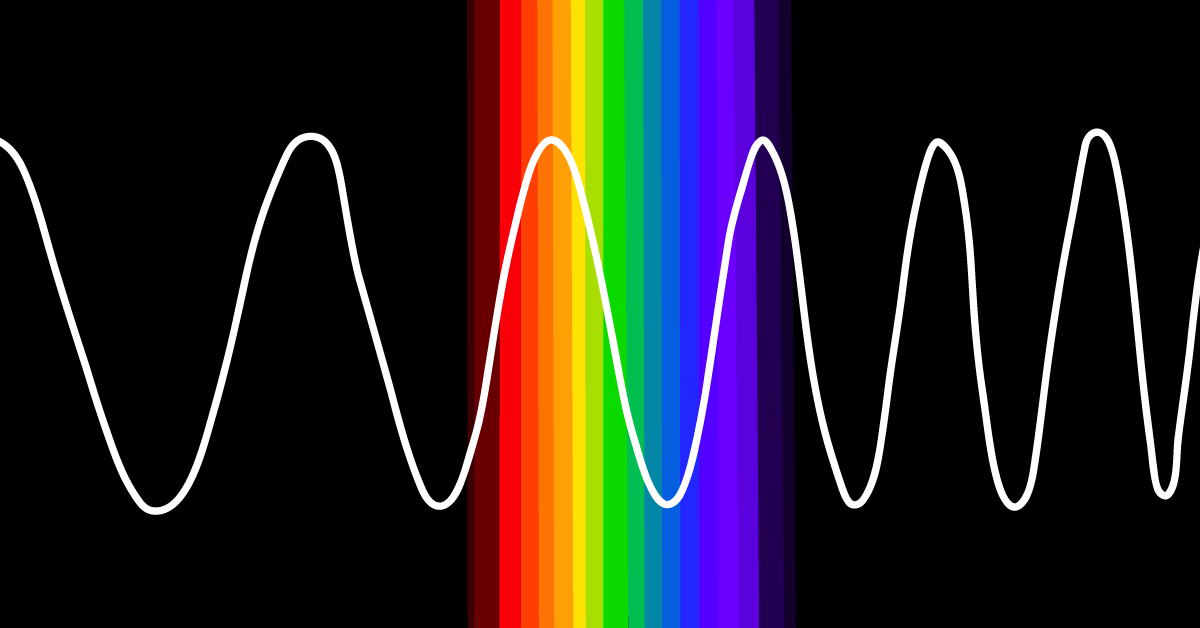
The flow of photon energy through space is defined as electromagnetic (EM) radiation. This EM radiation exhibits a wave-particle duality characterized by its frequency, wavelength, and energy.1
EM frequency, wavelength, and energy
As a wave, EM radiation is quantified by its frequency and wavelength. The frequency denotes the number of wave cycles that pass a specific point per second, expressed in hertz (Hz).
Similarly, the wavelength represents the distance between two consecutive high or low points of a wave, spanning atomic-scale distances to thousands of kilometers.1 As a particle, the EM energy is expressed in electron volts (eV) and is directly proportional to its frequency but inversely proportional to its wavelength.1
Figure 1 illustrates the relationship between the frequency, wavelength, and energy of EM radiation.
Figure 1: Courtesy of Cindy Hui, OD.
The electromagnetic spectrum
The EM spectrum encompasses the entire range of radiation, which can be grouped into distinct bands or regions. From the shortest to the longest wavelengths are: gamma radiation, X-ray radiation, ultraviolet (UV) radiation, visible light, infrared (IR) radiation, microwave radiation, and radio waves. Each of these categories can be further subdivided.1
Table 1 provides the EM radiation classifications and corresponding frequency, wavelength, and energy on the EM spectrum.
| Classes | Wavelength (λ) | Frequency (f) | Energy (E) |
|---|
| Gamma Rays | 10pm | 30EHz | 124keV |
| X-Rays | 100pm to 10nm | 3EHz to 30PHz | 12.4keV to 124eV |
| Ultraviolet | 10 to 380nm | 3PHz to 750THz | 3.1 to 10.2eV |
| Visible Spectrum | ~380 to 750nm | 780THz to 400THz | 1.65 to 3.27eV |
| Near Infrared (NIR) | 1μm | 300THz | 1.24eV |
| Mid Infrared (MIR) | 10μm | 30THz | 124meV |
| Far Infrared (FIR) | 100μm | 3THz | 12.4meV |
| Microwaves | 1mm to 1m | 300GHz to 300MHz | 1.24meV |
| Radio Waves | 1m to 100Mm | 300MHz to 3Hz | 1.24μeV to 12.4feV |
Table 1: Courtesy of Cindy Hui, OD.
Abbreviations from Table 1:
- pm-picometer
- nm-nanometer
- μm-micrometer
- mm-millimeter
- m-meter
- Mm-megameter
- EHz-exahertz
- PHz-petahertz
- THz-terahertz
- GHz-gigahertz
- MHz-megahertz
- Hz-hertz
- keV-kiloelectronvolt
- eV-electronvolt
- meV-millielectronvolt
- μeV-microelectronvolt
- feV-femtoelectronvolt
Lasers and the electromagnetic spectrum
The device known as a “laser” is based on the acronym for "light amplification by stimulated emission of radiation.” Lasers can produce beams of light that are coherent—a unique attribute that allows the beam to be adjusted for size, wavelength, and duration. For instance, laser beams can be concentrated into a tiny spot, kept within a tight frequency range, and produced in slow or ultrafast pulses.2
Figure 2 illustrates laser beam wavelength, coherency, and direction compared to other sources. A represents how a general source, such as a star, can produce electromagnetic radiation in different wavelengths, directions, and phases.
B demonstrates a light-emitting diode (LED), which emits light of a single wavelength that is incoherent (out of phase) in different directions. C shows a laser producing a concentrated beam of EM radiation that is coherent (in phase), directional, and of a distinct wavelength.
Figure 2: Courtesy of Cindy Hui, OD.
Laser interactions with biological tissue
When lasers interact with biological tissues, they produce specific effects based on photothermal, photochemical, and photodisruptive interactions.
- Photothermal Interactions: Turn light energy into heat, resulting in photocoagulation, where proteins denature, and photovaporization, which evaporates water from tissues, clinically seen as tissue burns.3
- Photochemical Interactions: Photochemical reactions are changes caused by light absorption. They involve (1) photoablation, fragmenting tissue polymers; (2) photoradiation, causing tissue damage when light combines with a photosensitizer; and (3) photodynamic effects, representing the cellular response following photosensitizer activation, the foundation for photodynamic therapy (PDT).4
- Photodisruptive Interactions: Create plasma or shock waves that cut through tissues.3
Lexicon of lasers
The terminology and abbreviations associated with lasers are extensive. Keep reading for a clear explanation of essential definitions and a compilation of the most frequently used lasers in eyecare.
Light sources
As
outlined in Figure 2, a general light source, such as a star, emits EM radiation in various wavelengths, phases, and directions. In comparison, an LED produces light of a specific wavelength that is incoherent (out of phase) and radiates in all directions.
In contrast, a laser generates a focused beam of EM radiation that has a distinct wavelength, is coherent, and travels in a specific direction.
Frequency doubling
Frequency doubling is a process in which a laser light, when passed through a special crystal, produces light with twice the frequency (or half the wavelength) of the original laser light.2 Changing wavelengths alters the laser's penetration abilities and its biological effects.
Continuous wave vs. pulsed lasers
Continuous wave lasers emit a steady, unbroken beam of light, whereas pulsed lasers release light in distinct bursts, with durations that can range from microseconds to milliseconds.2
Ultrafast lasers, a subset of pulsed lasers, produce exceptionally short pulses, typically in the picosecond (one trillionth of a second), or femtosecond (one quadrillionth of a second) range.
Laser vocabulary
- Q-switched Lasers: A Q-switched laser is a type of pulsed laser that produces high-intensity, short-duration pulses. They are particularly useful for applications requiring high power in brief durations.2
- Gain Medium: A gain medium is the material in a laser used to amplify the light signal, usually a solid, gas, or liquid.
- Doped: A doped laser uses a gain medium, like a crystal or gas, infused with specific impurities to amplify light at particular wavelengths. The type of impurity determines the emitted light's wavelength.2
- For instance, Nd:YAG lasers have neodymium-doped crystals, while Er:YAG lasers use erbium-doped ones.
- Ablative, Fractional, and Non-Ablative Lasers: Lasers can be classified as fully ablative, fractional (or fractionally ablative), and non-ablative.
- Fully ablative lasers vaporize an entire layer or portion of tissue.
- Fractional lasers treat a tissue fraction, creating microscopic zones and preserving surrounding tissues for faster recovery.
- Non-ablative lasers target underlying tissue without affecting the outer surface.
Types of lasers
Lasers can be classified based on the type of gain medium—solid, gas, or liquid dye.
Solid-state lasers
Solid-state lasers have a solid material, like a ruby rod or crystal, and are known for their high output power.
Examples of solid-state lasers used in ocular procedures include:
- Diode
- Erbium:Glass (Er:Glass)
- Erbium-doped yttrium aluminum garnet (Er:YAG)
- Femtosecond
- Holmium-doped yttrium aluminum garnet (Ho:YAG)
- Neodymium-doped yttrium aluminum garnet (Nd:YAG)
- Neodymium-doped yttrium aluminum garnet potassium titanyl phosphate (Nd:YAG-KTP)
- Potassium titanyl phosphate (KTP)
- Q-switched neodymium-doped yttrium aluminum garnet (Nd:YAG)
- Ruby
- Yttrium aluminum garnet (YAG)
Gas lasers
Gas lasers use gas or a mixture of gases and are known for producing stable continuous wave outputs.
Examples of commonly used gas lasers include:
- Argon
- Carbon dioxide (CO2) laser
- Excimer
- Krypton
- Xenon arc
Liquid dye lasers
Liquid dye lasers use organic dyes dissolved in solvents and can emit a wide range of wavelengths depending on the dye used. The pulsed dye laser (PDL) and long-pulsed (LP PDL) are examples of liquid dye lasers.
EM radiation in ophthalmic imaging
Optical coherence tomography
Most OCT devices, like spectral-domain OCTs (SD-OCT), utilize IR light (820 to 870nm). In contrast, swept-source OCTs (SS-OCT) operate at a longer IR wavelength of 1050nm to improve imaging of deeper structures such as the choroid.5
Scanning laser ophthalmoscopy
Scanning laser ophthalmoscopy (SLO) works by passing a focused laser beam across the retina to generate a two-dimensional image. Confocal SLO (cSLO) boosts the contrast and definition of SLO with a spatial filter.
Together with SD-OCT, cSLO facilitates multicolor imaging from blue (488nm), green (515nm), and infrared (820nm) lasers, eliminating the need for a separate fundus camera.6
Fundus fluorescein angiography
In FFA, blue light (465 to 490nm) stimulates fluorescein dye,7 whereas in ICGA, near-infrared light at 800nm energizes indocyanine green dye.8
Fundus autofluorescence imaging
Short-wavelength fundus autofluorescence (SW-FAF) implements a 488nm blue light to detect lipofuscin buildup, indicating metabolic concerns in the RPE.9 Similarly, in near-infrared autofluorescence (NIR-FAF), the autofluorescence of melanin in the RPE and choroid is detected using wavelengths of 787 to 800nm.9
Near-infrared reflectance
Near-infrared reflectance (NIR-R) illuminates the retina with an 820nm light for subretinal imagery. OCT devices often feature a high-contrast NIR setting onboard.10
Laser Doppler flowmetry
In laser Doppler flowmetry (LDF), NIR light interacts with blood cells, producing a Doppler shift that generates a blood flow velocity map. LDF can be used to study blood flow in the retina, choroid, and ONH.11
Similarly, laser Doppler holography (LDH) offers enhanced blood flow resolution over LDF by examining sequences of interference patterns or holograms.12 Finally, laser speckle flowgraphy (LSFG) utilizes the changing speckle patterns of coherent laser light at 830nm as it interacts with moving blood cells, providing real-time retinal blood flow data.13
Corneal applications of EM radiation
Laser-assisted in situ keratomileusis
Variations of LASIK
Innovations designed to minimize flap-related complications have led to numerous variations of the LASIK procedure. Some of these variations incorporate the use of the femtosecond (FS) laser for corneal flap creation.
- FS Laser-Assisted LASIK (FS-LASIK): Harnesses a femtosecond laser for precision flap creation.14
- Transepithelial Photorefractive Keratectomy (tPRK) and Transepithelial Phototherapeutic Keratectomy (tPTK): Both employ the excimer laser for ablation following manual debridement. The distinction lies in their intent—PRK is refractive, while PTK is therapeutic, treating anterior corneal degenerations, dystrophies, and other keratopathies.
- Similarly, tPRK and tPTK utilize the excimer laser for both epithelial debridement and corneal ablation.15,16
- PresbyLASIK: In this procedure, a corneal flap is formed using either a microkeratome or an FS laser. The distinctive aspect of PresbyLASIK is the adjustment of the excimer laser ablation pattern to establish multiple focal zones.17
Table 2 provides a comprehensive overview of LASIK variations, including those not discussed in this text, as well as a summary of refractive procedures and the respective lasers used.
| Corneal Procedure (Refractive) | Excimer Laser | Femtosecond Laser |
|---|
| LASIK and Epi-LASIK | X | |
| Laser Subepithelial Keratomileusis (LASEK) | X | |
| Mitomycin C LASEK (MMC-LASEK) | X | |
| PresbyLASIK | X | |
| PRK | X | |
| tPRK | X | X |
| Femtosecond Laser-Assisted PresbyLASIK | X | X |
| Femtosecond Laser-Assisted LASIK (FS-LASIK) | X | X |
Table 2: Courtesy of Cindy Hui, OD.
Refractive corneal lenticule extraction
Refractive corneal lenticule extraction (RCLE) procedures involve the removal of a corneal disc, or lenticule, to correct refractive errors.
In FS lenticule extraction (FLEx), an FS laser creates a corneal flap and lenticule, whereas in
small incision lenticule extraction (SMILE), the FS laser forms the lenticule and side-cut incision, providing access for lenticule removal.
15FS laser-assisted intrastromal corneal implantation
FS laser-assisted intrastromal corneal implant procedures utilize FS lasers to make precise corneal channels for the insertion of implants such as intrastromal segments to address refractive errors or
keratoconus.
18Laser thermokeratoplasty
Laser thermokeratoplasty (LTK) engages a Ho:YAG laser operating at 1200nm to correct hyperopia by inducing peripheral corneal collagen shrinkage.
19 Conversely,
conductive keratoplasty (CK) applies radiofrequency energy (350 kilohertz [kHz]) to the peripheral cornea.
20EM radiation in corneal treatment procedures
Several keratoplasty procedures apply the FS laser (to make incisions and sculpt the donor graft tissue) and the excimer laser (to ablate the cornea). Also, UV light is used for corneal strengthening techniques.
Corneal surgical procedures that utilize lasers or UV light include:
- FS Laser-Assisted Deep Anterior Lamellar Keratoplasty (FS-DALK): Incorporates the FS laser for incisions to separate the stroma from Descemet’s membrane.21
- FS Laser-Assisted Descemet Stripping Endothelial Keratoplasty (FS-DSEK): The laser prepares the donor tissue and makes the graft incision.21
- FS Laser-Assisted Descemet Membrane Endothelial Keratoplasty (FS-DMEK): Uses the FS laser for both the recipient incision and donor tissue preparation.19
- FS and Excimer Laser-Assisted Endothelial Keratoplasty (FS-FELEK): Features a combined approach in which the FS laser handles donor graft fabrication and the excimer laser manages tissue ablation.21
- Corneal Cross-Linking (CXL) and Photorefractive Intrastromal Cross-Linking (PiXL): Both are corneal strengthening procedures that use 365nm UV light in conjunction with riboflavin (vitamin B2) drops.22
- PiXL is a modification of the CXL protocol distinguished by the use of UV light that is geometrically arranged.23 The UV light used in CXL and PiXL can be sourced from a laser or non-laser device.
Table 3 summarizes corneal treatment procedures and associated laser(s).
| Corneal Procedure (Therapeutic) | Excimer Laser | UVA | Ho:YAG | Radio | Femtosecond Laser |
|---|
| PTK | X | | | | |
| tPTK | X | | | | X |
| CXL | | X | | | |
| PiXL | | X | | | |
| LTK | | | X | | |
| CK | | | | X | |
| FS-DALK | | | | | X |
| FS-DSEK | | | | | X |
| DMEK | | | | | X |
| FELEK | X | | | | X |
Table 3: Courtesy of Cindy Hui, OD.
EM energy in glaucoma and iridotomy procedures
Laser peripheral iridotomy
Laser peripheral iridotomy (LPI) is essential for relieving pupil block, increasing aqueous outflow, and preventing
acute primary angle closure (APAC) and related conditions.
24Historically, LPI used the argon laser, emitting blue-green light at 488 to 514nm. Today, the preferred lasers are the Nd:YAG-KTP laser (532nm) and the Q-switched Nd:YAG laser, which functions at 1064nm with less energy, consequently causing less damage to nearby structures.
For clarification, because the Nd:YAG-KTP laser emits light in the green spectrum, similar to the argon laser, it has been colloquially or mistakenly referred to as an "argon laser," a reference that persists today.
Argon laser procedures
Despite their diminished use in LPIs, argon lasers remain the laser of choice in argon laser peripheral iridoplasty (ALPI), argon laser pupilloplasty (ALPP), and argon laser trabeculoplasty (ALT).
The argon laser (1) delivers circumferential iris burns in ALPI, pulling the iris away from the anterior chamber angle;25 (2) modifies the pupil's size, shape, and position in ALPP;26 and (3) targets the trabecular meshwork in ALT.27
Selective laser trabeculoplasty
Selective laser trabeculoplasty (SLT) is similar to ALT, except the trabecular meshwork is targeted using a 532nm frequency-doubled Q-switched Nd:YAG laser.
27 Laser suture lysis
After
glaucoma surgery, laser suture lysis (LSL) ensures improved scleral closure using lasers like the argon, Nd:YAG (either 1064nm or 532nm), diode (840nm), krypton (647nm), or yellow Pascal (577nm) laser.
28CO2 laser-assisted sclerectomy surgery
Cyclophotocoagulation
Cyclophotocoagulation (CPC) reduces aqueous humor production and lowers IOP by targeting ciliary processes with laser energy.
Transscleral cyclophotocoagulation (TS-CPC) delivers this energy through the sclera with a specialized probe, eliminating the need for direct visualization of the ciliary processes. The 810nm diode laser is favored over the 1064nm Nd:YAG and 693nm ruby lasers for its depth and safety.30
Endoscopic cyclophotocoagulation
Endoscopic cyclophotocoagulation (ECP) integrates an 810nm diode laser for tissue ablation, a xenon (broad spectrum white) light source for clear tissue visualization, and a 632.8nm helium-neon (HeNe) laser aiming beam for precise targeting during ciliary process photocoagulation.
30 EM radiation in cataract-related procedures
FS laser-assisted cataract surgery
YAG capsulotomy
The Nd:YAG laser (1064nm) is the gold standard in YAG capsulotomy, a routine method to treat posterior capsule opacification following
cataract surgery.
32FS laser-assisted capsulotomy
Capsulotomies with the FS laser provide consistently sized and perfectly circular anterior capsulotomies, offering enhanced precision in centration and diameter compared to manual techniques.33
Plasma blade capsulotomy
Plasma blade capsulotomy administers radiofrequency (RF) energy for precise incisions in the anterior capsule without causing bleeding or collateral tissue damage.33
Precision pulse capsulotomy
Precision pulse capsulotomy (PPC), commercially known as
Zepto, deploys a focused, rapid, multipulse, low-energy RF discharge to produce precise capsulotomy outcomes.
33Dye-assisted capsulotomy
In dye-assisted capsulotomy, the primary role of the dye is to stain the lens capsule, thereby improving its visibility. While many dyes do not require specific light for observation, certain light sources can enhance the viewing experience.
For instance, trypan blue and gentian violet do not need any specialized light. In contrast, fluorescein and indocyanine green dyes are optimally viewed using blue light (465 to 490nm) and near-infrared light (780 to 805nm), respectively.33
EM radiation in posterior segment procedures
Laser vitreolysis
Laser vitreolysis is a posterior segment procedure that applies the Nd:YAG laser to target vitreal floaters.34
Laser photocoagulation
Four primary types of lasers are used in laser photocoagulation to address
retinal pathologies:
35- The argon and frequency-doubled Nd:YAG (532nm) lasers serve as the primary tools for panretinal photocoagulation in proliferative diabetic retinopathy (PDR) and macular edema.
- The krypton red laser is particularly effective in treating choroidal neovascularization (CNV).
- Meanwhile, the diode laser, with its deep penetration capabilities, is most suited for managing retinopathy of prematurity (ROP).
Photodynamic therapy
Photodynamic therapy combines a photosensitizer and specific light to treat targeted tissues and conditions.
Verteporfin
AMD and
central serous chorioretinopathy (CSCR) use verteporfin (tradename: Visudyne), which is activated by light at 689nm. Originally developed for AMD-related CNV, PDT is not as widely used and is now secondary to anti-vascular endothelial growth factor (VEGF) therapy.
365-aminolevulinic acid
PDT produces antimicrobial and anti-inflammatory effects when a photosensitizing agent such as 5-aminolevulinic acid (5-ALA) is exposed to red light at 630 to 635nm.37
EM radiation in skin resurfacing procedures
Fully ablative and fractional lasers
CO₂ and Er:YAG lasers
Both the CO₂ and erbium-doped yttrium aluminum garnet (Er:YAG) lasers can function as either fully ablative or fractional instruments. These lasers are used in laser skin resurfacing for treating periorbital wrinkles, scars, and photodamage.38
Non-ablative lasers
Non-ablative lasers mainly target telangiectasias, which are dilated blood vessels near the surface of the skin.38 The 532nm and the 595nm pulsed dye laser (PDL) effectively treat facial vasculature, with the PDL also refining skin quality.
The long-pulsed PDL (LP PDL) between 500 to 1200nm addresses actinic keratoses (scaly patches) and sun spots, with improved outcomes using 5-ALA.38
Intense pulsed light (IPL) treats vascular and pigmented lesions, also with increased potency from 5-ALA.
38 The diode laser at 1450nm, Nd:YAG at 1320nm, and the Er:Glass laser at 1540nm focuses on refining skin texture.
38 Radiofrequency
Radiofrequency techniques induce deep dermal heat, stimulating collagen retraction and increasing collagen and elastin production. Thermage (6.78MHz) is approved for the rejuvenation and tightening of periorbital skin, while eMatrix (2.64MHz) is used to augment tissue volume in the upper eyelid and eyebrow region.
38 Gamma rays
Cobalt-60 (60Co), a radioactive isotope of cobalt, emits high-energy gamma photons after undergoing radioactive decay.
Gamma-ray sterilization
This gamma radiation emission is harnessed for sterilizing ophthalmic surgical devices and other products like irrigation kits, eye droppers, and ointments.39
Gamma knife surgery (GKS)
X-ray irradiation
The X-ray irradiation process utilizes photon radiation to sterilize and decontaminate, similar to gamma-ray sterilization. Although not as prevalent, X-ray irradiation is gaining traction in usage.41
Conclusion
While the use of these technologies does not necessarily require extensive knowledge of the underlying mechanics, having a deeper understanding offers insight into ocular disease pathophysiology while also adding credibility when discussing these procedures.
Understanding the entanglement between the electromagnetic radiation in the universe and the ocular applications and procedures not only deepens the understanding of optometry but also enriches the approach to patient care.