Until 2011, the general consensus in the eyecare community was that dry eye was an aqueous deficiency problem, and treatments were targeted toward managing the symptoms of dry eye rather than directly treating the condition.1,2
Then, Caroline Blackie, OD, and Donald Korb, OD, who have been on the front lines of
meibomian gland dysfunction (MGD) research for many years, argued that doctors should proactively look for MGD and dry eye disease (DED) will follow.
2 This represented a major shift in prior thinking.
3The link between dry eye disease and MGD
Dry eye happens when the
ocular surface system cannot adequately protect itself from desiccating stress, such as wearing a contact lens, working long hours on computer screens, or being in dry environments. Decades of clinical evidence point to MGD as the main culprit and the root cause of most cases of dry eye disease.
1,4,5 Recent research indicates that 86% of patients who have dry eye have MGD.
6When MGD is not treated, it causes or worsens dry eye symptoms, including dryness, burning, itching, tearing, and foreign body sensation.7 In addition, visual effects of MGD include reduced tear breakup time (TBUT), tear film instability, and evaporative dry eye disease. Since MGD can be asymptomatic, expressing glands and checking gland morphology is recommended during routine eyecare visits.8
Shifting the mindset to treat MGD in DED patients proactively
Since Drs. Korb and Blackie argued to look for MGD to treat dry eye disease in 2011, MGD is now widely recognized as a leading cause of dry eye disease. Even though DED is defined as a multifactorial disease that can affect the ocular surface and tear film, practitioners most often actively screen for MGD during routine eyecare visits.9
Dry eye disease is one of the most common reasons people seek eyecare and its prevalence is only likely to increase due to an aging population, increased use of screens, and environmental changes.
9 However, early screening, treatment, and lifestyle modifications can provide better results and keep MGD in a prolonged asymptomatic phase.
10 Meibomian gland dysfunction overview
Pathophysiology of MGD
While MGD is multifactorial and complex, its pathophysiology is thought to be driven by epithelial hyper-keratinization, which leads to duct obstruction, meibum stasis, cystic dilation, and eventual disuse acinar atrophy and gland dropout.4
There are many risk factors for MGD, including
contact lens wear, hormonal changes, age, makeup use, and skin diseases.
2Signs and symptoms of MGD
MGD and evaporative dry eye disease can have very similar symptoms.
10 In my clinical practice, it seems that every person
experiences dry eye a little differently. When discussing their reported symptoms, most patients rationalize their symptoms as having allergies, not getting enough sleep, overwearing their contacts, or getting soap in their eyes.
Signs and symptoms of MGD include:1
- Watering
- Burning
- Itching
- Stickiness
- Light sensitivity
- Red eyes
- Grittiness
I often have to explain to the patients that their symptoms might be transient, but MGD and dry eye cause them. To make matters worse, the condition is progressing while they try different palliative treatments. We have to educate our patients on newer treatment options beyond artificial tears.
Screening for meibomian gland dysfunction
Screening methods for dry eyes include SPEED questionnaires, vital stains to check for corneal or conjunctival damage, MMP-9 testing for inflammation, and meibography for gland integrity.6
The doctor must put together a
diagnostic puzzle for the patients and help them connect the dots between their symptoms and MGD, as one study showed that patients who self-reported symptoms have a low accuracy for MGD diagnosis.
11Clinical studies linking MGD and DED
The following studies were chosen for three primary reasons. First, they are global in nature (Singapore, Austria, Thailand, India, etc.), which demonstrates that
DED and MGD are global issues, with eyecare professionals worldwide making a collective effort to solve this ongoing puzzle.
Secondly, each study seeks to determine which screening test and/or clinical observation will best allow the doctor to diagnose this condition earlier in order to have the maximum impact on the patient's life.
Third, these studies take varied approaches to both diagnose and treat the patient while taking into consideration the clinical utility of the test in terms of availability, ease of use, and cost. To this end, some studies incorporate more advanced instrumentation (Lipiview, meibography, etc.) along with traditional dyes and observation.
Singapore specialty dry eye clinic study on MGD and dry eye subtypes
This
study evaluated screening methods and associated factors of MGD and dry eye disease in 200 patients in a specialty dry eye clinic.
11 The study was conducted in a hospital clinic, the Singapore National Eye Center, from 2006 to 2007.
The subjects were evaluated for dysfunctional tear syndrome (DTS), meibomian gland disease, corneal fluorescein staining, Schirmer test (ST) result, fluorescein tear break-up time (TBUT), and subjective symptoms.11
In all patients examined, evaporative dry eye was the most common type at 58%, followed by the mixed evaporative and aqueous tear deficiency types at 30.5%. Mixed-type dry eye had the most severe fluorescein staining in the central and inferior cornea.11
Singapore MGD/DED study methods
The study specifically looked for predisposing risk factors such as history of dry mouth, previous or current contact lens wear, known history of diabetes mellitus, rheumatoid arthritis, thyroid disease, or ocular surgery such as
LASIK or cataract surgery.
11 Subjects were also asked about the use of oral contraceptives, hormonal preparations, antihistamines, antispasmodics, and drugs for hypertension, depression, and Parkinsonism.
Referral to the specialty dry eye clinic had no specific criteria, but one ophthalmologist evaluated all referred patients. Assessment of dry eye included a TBUT test, grading of corneal fluorescein staining, and tear secretion.11 The examining doctor recorded spots of corneal fluorescein staining over the central zone and the superior, inferior, nasal, and temporal quadrants.11
How was dry eye measured?
An adapted Ocular Surface Disease questionnaire was used, and all symptoms were graded as 0 (never present) or 1, 2, 3, or 4 (always present at least once a day in the past week).11 Dry eye was classified according to Delphi Consensus Dysfunctional Tear Syndrome (DTS) levels, in which DTS I was the mildest, followed by II, III, and IV (most severe).11
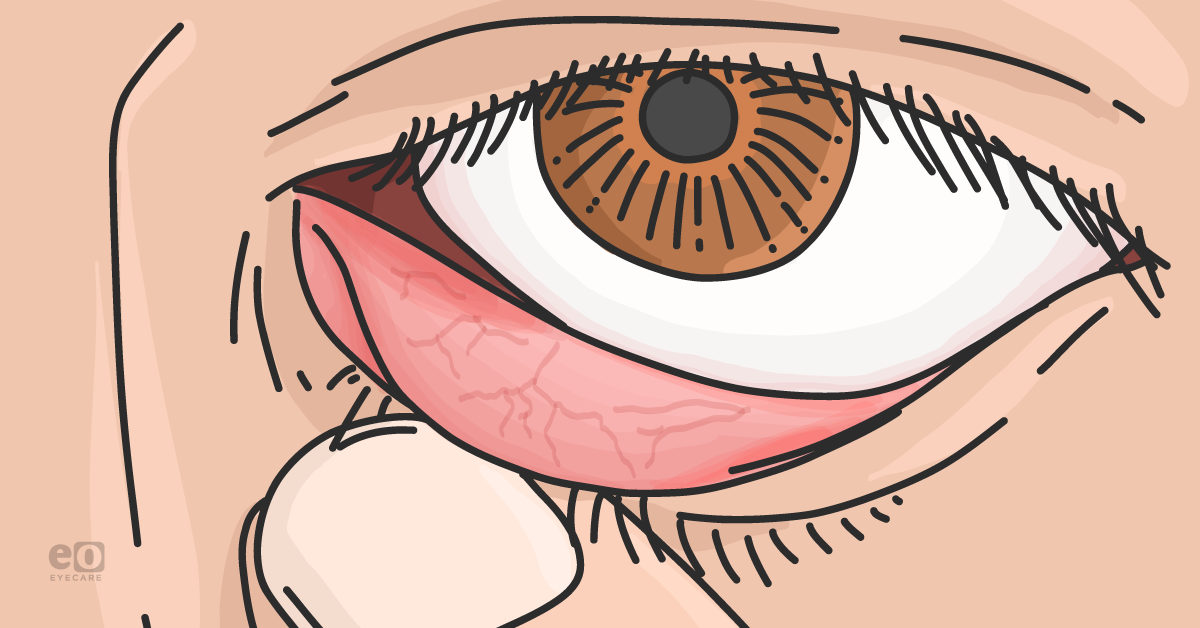
The severity of MGD was screened using Yamaguchi grading, microscopic signs of MGD, and expressivity of the meibomian glands.11 Expressibility of the MG was evaluated by gentle pressure on the lower eyelids, and the expressed secretion was graded as watery or viscous.
Breakdown of Yamaguchi grades 0 to 4:
- Yamaguchi grade 0 is the least severe to indicate a posterior location of the mucocutaneous junction (Marx's line).11
- Yamaguchi grades 1 and 2 are intermediate positions of Marx's line. Microscopic signs of MGD included the presence of misdirected lashes, the fragility of lashes, scurf formation, irregularity of the MG orifice, loss of expressibility of the MG, and formation of plaques.11
- Yamaguchi grade 3 is the most severe to indicate an anterior position of the Marx's line relative to the meibomian gland (MG) orifices.11
Singapore MGD/DED study results
The mean age of the patients was 52.2 ± 14.9 years, and 62.5% were women.11 Of the participants, 87% were Chinese, and 13% were of minority ethnicity (3.5% Asian Indians, 2% Caucasians, 1.5% Malay, and 6% other).11
Additionally, 11.5% of the patients were wearing contact lenses currently, and 19.5% had a history of dry mouth. Within the patient population, 1.5% had a known history of diabetes mellitus, 3% had
rheumatoid arthritis, 5.5% had thyroid disease, and 1.0% had undergone ocular surgery (LASIK or cataract).
11This clinic-based study showed that a simple MGD screening test based on the position of Marx's line in the eyelid was correlated to TBUT and visual functional difficulties.11 Tear secretion was associated with early morning or nocturnal discomfort, whereas abnormal TBUT was associated with discomfort in windy conditions.
Fluorescein staining in the central and inferior cornea was most severe in mixed evaporative and hyposecretory dry eye. The sex of the patient predominantly influenced the corneal staining.11
Takeaway: Based on this clinic-based study conducted in Singapore, an MGD screening test based on the anteriorization of Marx's line provides clinical information. When used in conjunction with conventional dry eye tests such as Tear Secretion, TBUT, and fluorescein staining, this screening test is associated with reversibility of visual blurring and difficulty in reading.11 More studies are needed to evaluate MGD screening in people without dry eye.
Austrian dry eye clinic: prevalence of MGD, tear film, and ocular surface parameters
This
study in Austria looked at the prevalence of meibomian gland dysfunction and its association with tear film and ocular surface disease (OSD) in dry eye patients.
12 The researchers retrospectively evaluated records of 1,372 consecutive patients from a dry eye clinic at the Medical University of Graz, Austria, between 2004 and 2010 and evaluated symptoms and objective tear film and ocular surface parameters.
12The mean age was 54.3 ± 17.8 years, and 71.3% were female.12 The study excluded patients who had undergone ocular surgery in the past 6 months.12 The patients were then classified into different subgroups, including pure MGD, pure aqueous tear deficiency (ATD), MGD combined with ATD, pure anterior blepharitis (AB), Sjögren's syndrome (SS) without MGD, and SS together with MGD.
Austrian dry eye clinic MGD/DED study methods
Researchers evaluated fluorescein tear film break‐up time (FBUT), and the Schirmer test was carried out without prior application of a local anesthetic. Further evaluation of the ocular surface was performed by lissamine green staining, and the researchers checked for the presence of telangiectasia, erythema, and irregularity of the lid margins.12
Statistically, 70.3% (765 patients) of the investigated population had signs of
meibomian gland dysfunction, and their mean age was 55.4 ± 16.6 years.
12 The intensity of symptoms did not differ between subgroups, and 50.8% (490 patients) of MGD patients had Schirmer test values ≤10mm at 5 minutes.
12 The fluorescein break‐up time and Schirmer test values were significantly higher in the pure AB and MGD groups.
The pure MGD group showed a significantly lower fluorescein staining of the cornea compared to the other groups, except for pure AB.12 Lissamine green staining of the ocular surface was present in all groups but was least pronounced in the pure MGD and AB groups.
Takeaway: This study showed that MGD is a major cause of ocular discomfort and is often combined with a reduced aqueous tear secretion.12 A good baseline evaluation with newer technologies such as noninvasive tear film break-up time, osmolarity testing, visualization of the lipid layer as well as meibomian gland imaging is needed for a more objective analysis of dry eye disease.12
Indian tertiary care hospital prevalence and association of MGD with dry eye severity
This
study’s goal was to find out the prevalence and association of MGD and dry eye, including asymptomatic individuals having MGD and dry eye in patients that are 30 to 80 years old.
13 The study, which included 389 patients, occurred between February 2020 and February 2021 at an outpatient department (OPD) of a rural tertiary care hospital in central Gujarat, India.13 The study excluded patients with dry eye related to Sjögren's syndrome, cicatricial pemphigoid, and chemical injuries.
Indian hospital MGD/DED study methods
The participants completed the standardized OSDI questionnaire and provided personal and past history, including the use of
systemic drugs, hormonal pills, comorbidities such as diabetes mellitus, hypertension, thyroid disease, refractive surgeries, cataract surgeries, or use of contact lenses.
13 The researchers evaluated meibomian gland morphology by checking meibomian gland orifices, expressibility and quality of meibum, and meibomian gland dropout.
In this study, 758 out of the 778 eyes showed changes characteristic of MGD, with a 97.4% prevalence of MGD. Of 389 participants, 356 (91.5%) had dry eyes.13
Furthermore, the study results showed that the prevalence of MGD increased with age, and higher MGD scores were found to increase with dry eye severity.13 The highest MGD scores were observed when the tear break-up time was ≤5 seconds.13
Takeaway: Higher MGD scores were associated with an increase in dry eye severity, suggesting MGD is a contributory factor for dry eyes. As 219 (56.3%) of the participants with dry eye were asymptomatic, it shows that diagnosis and treatment of MGD and dry eye is critical.13
Thailand DED prevalence in medical students during COVID-19 pandemic study
During the COVID-19 pandemic, medical students were at high risk for developing dry eye symptoms due to the increasing use of computers for online lectures. Medical students were asked to complete a semi-structured questionnaire and given a LipiView II interferometer examination.14
The survey questionnaire had four sections: demographic data with pre-existing medical conditions, risk factors for DED, psychological stress, and a dry eye questionnaire using the Ocular Surface Disease Index (OSDI).14 All participants were examined with the LipiView ocular surface interferometer.
Chiang Mai University DED prevalence study methods
The study excluded participants who had ocular diseases such as ocular infection, allergy, autoimmune disease, history of ocular surgery or trauma within 3 months, and those using punctal plugs or topical ocular medications other than
artificial tears.
14 Participants who used artificial tears were instructed to stop the use 6 hours before the LipiView II examination.
The LipiView II ocular surface interferometer was used to measure lipid layer thickness (LLT), meibomian gland dilatation (tortuosity), meibomian gland dropout, and blinking pattern. A single experienced Lipiview II observer (CT) subjectively evaluated the meibomian gland dropout in both upper and lower eyelids using a validated Meibograde grading 4-point scale from 0 to 3 in which grade 0 is 0 to 25% meibomian gland loss; grade 1, 26 to 50% loss; grade 2, 51 to 75% loss; and grade 3, more than 75% loss.
For this survey, 528 medical students completed all questionnaires and the meibomian gland evaluation using the LipiView II interferometer, and the prevalence of DED based on symptoms was 70.8%.14 Based on the OSDI scores, 24.8 % of the medical students had mild dry eye disease, 18.8% had moderate DED, and 27.8% had severe DED.14
Using an average Meibograde of 0.75 as a cut-off, 60.98% (322 of 528) of the medical students had total MGD with 100% specificity of MGD diagnosis.14 Of these, the prevalence of asymptomatic MGD was 17.61% (93 of 528), and symptomatic MGD was 43.37% (229 of 528).14
Takeaway: This study showed a high prevalence (70.8%) of symptomatic DED in medical students.14 Contact lens wear, psychological stress, and prolonged use of computers significantly correlated with the risk of DED.14 The prevalence of MGD in medical students was 60.98% and was mostly symptomatic.14
Current treatments for DED and MGD
Five
FDA-approved medications (Tyrvaya, Cequa, Restasis, Xiidra, and Eysuvis) for dry eye disease are currently available.
8 Recommending eye drops for DED is an easier conversation to have with patients because they expect that treatment option. Changing the paradigm in the patient’s mind to more advanced treatments, such as
in-office treatments, which are mostly out of pocket, is more challenging.
In-office treatments include Lipiflow thermal pulsation, TearCare, iLux, Mibo ThermaFlo, EyeXpress, Intense pulsed light, Blephex, and NuLids PRO.8 Most treatments target the function of the meibomian glands, while BlephEx and NuLids PRO target lid margin debris and the biofilm.
Intervening earlier in DED and MGD progression
Even just 10 years ago, doctors did not have the advanced devices to actively clean or remove biofilm and debris from the eyelid (microblepharoexfoliation), which we now know is key to keeping these patients healthy.
A patient’s natural response is experimenting with over-the-counter eye drops as conventional therapy for redness, dryness, and burning. Doctors need to change the paradigm early on in the disease process and recommend in-office treatments when palliative treatments do not help manage symptoms.
Recent research indicates better outcomes for patients with in-office treatments, such as
Lipiflow or iLux, compared with more conservative treatments, such as eyelid hygiene and warm compresses alone.
15Recommendations from the author on the OD’s role in MGD management
- Doctors need to be more proactive in looking for MGD. We cannot wait for the patient to complain about symptoms once the disease progresses.
- We, as practitioners, need to encourage patients to consider in-office treatments for both symptomatic cases and preventative care. In my clinic, most patients are surprised to see their meibography images and do not understand that their symptoms are linked to blockages in their oil glands.
- Don’t be discouraged when patients do not accept treatments immediately. After I evaluate the oil glands and review meibography and their symptoms, most patients appreciate the knowledge. Many will accept an in-office treatment immediately.
- The remaining patients think about the options and remember our conversation even a year later. I have primed them for the conversation about their eyelid health and the little glands in their lids.
- We need to shift the paradigm from palliative treatments to more active screening and treatment of the disease.
- Meibomian gland dysfunction is best treated early. We must diagnose MGD at the first sign of compromise, such as lid swelling and inflammation, rather than wait for late-stage symptoms.9
Patient education on the link between MGD and dry eye
Once the doctor has diagnosed MGD and teased out the patient’s symptoms, they must educate the patient. Delivering your findings and convincing the patient is perhaps the most challenging task. Many times, patients have become accustomed to their eyes feeling dry, watering, and burning over the years.
The chronic nature of the disease makes it difficult for patients to recognize the symptoms early on in the disease process. In my experience, after having an in-office treatment such as Lipiflow, iLux, or IPL, patients learn to recognize what good feels like.
They start to make the connection between the symptoms and the relief the treatments provide. So, once the symptoms return, they are more aware and notice changes in how their eyes feel. Now, they are much more accepting and willing to pay for re-treatments. The challenge is
educating patients on the tiny oil glands in their eyelids and how they impact the comfort of their eyes.
How to facilitate patient communication about MGD
Sharing information in an easy-to-understand manner and, most importantly, showing them imaging of their eyelids helps patients understand the nature of the problem. Repeating the message at every comprehensive exam helps solidify the need for treatment. Some patients may not agree to treatments immediately, but they will research and pay more attention to their habits and symptoms.
We need to get away from waiting for the patient to complain and be more active in both looking for MGD and
confidently recommending treatments. Practitioners must tell the patient with authority that meibomian gland dysfunction is a problem and needs treatment to prevent progression.
Closing thoughts
In our increasingly digital world, diagnosing MGD and dry eye disease early and routinely is crucial to
maintaining the patient’s ocular health. We know that by the time the patient is 50, we have lost most of the time to reverse the disease process, and all we are doing is slowing down progression. Dry eye screening in the patient’s 20s and 30s is critical for their long-term eye health.
8We have come a long way in dry eye diagnosis and treatments but there are still areas that need more understanding. Diagnosing and treating MGD and dry eye disease is a work in progress.