An acute angle closure crisis (AACC) is a true
ocular emergency that requires immediate and appropriate management in order to prevent irreversible vision loss, which can occur within hours or days if left untreated. According to a study by Sng et al., only one episode of an AACC is sufficient to cause peripapillary retinal nerve fiber layer thinning, mild visual field defects, and optic disc pallor.
This article will outline:
- How to identify, diagnose, and treat an AACC
- Highlight a step-by-step emergency management protocol to avert the crisis and stabilize the patient in a prompt and efficient manner
- Follow-up care for optometrists in states with restricted laser authority
- Referral guidelines
Pathophysiology
Primary angle closure disease
Primary angle closure disease (PACD) is a spectrum of disease relating to anterior chamber angle narrowing. Multiple anatomical features and physiological mechanisms can cause PACD, with pupillary block being the main process in the majority of cases.
Pupillary block
A pupillary block occurs when there is abnormal contact between the iris and the lens, which prohibits the aqueous flow from the posterior to the anterior chamber, causing a pressure difference between the two. This pushes the iris forward and creates contact with the trabecular meshwork and/or peripheral cornea, resulting in angle closure.2
Plateau iris configuration
Additionally, different lenticular features, such as size, shape, and position, can result in a shallow anterior chamber, which contributes to PACD. Variations in iris and ciliary body anatomies, such as iris thickness, anterior iris insertion, or anterior ciliary position, can also cause the peripheral iris to come into contact with the trabecular meshwork.
“In contrast to pupillary block-induced angle closure, plateau iris configuration is characterized by anteriorly positioned ciliary processes which push the iris root forward.”
This creates a peripherally narrow anterior chamber and centrally deep anterior chamber, inducing angle narrowing via anteriorly positioned ciliary processes. Plateau iris configuration patients who have had a
patent laser peripheral iridotomy (LPI) can still have persistent angle closure, known as plateau iris syndrome.
3Figure 1 illustrates the differences between an open angle (diagram a) versus a narrow/closed angle (diagram b). Note the resulting iris bombe caused by the pupillary block and greater posterior chamber pressure.
Figure 1: courtesy of Cindy Hui, OD
Identifying the spectrum of PACD
Iridotrabecular contact (ITC) is defined as the iris appearing to touch the anterior chamber angle at the posterior pigmented trabecular meshwork, or more anterior structures, as observed on gonioscopy without compression. Quantifying ITC is essential when classifying the different forms of PACD.2
Primary angle closure suspect
Patients with greater than or equal to 180 degrees of ITC, no peripheral anterior synechiae (PAS), normal IOP, and
no optic nerve damage are considered primary angle closure suspects (PACS). These patients have potentially occludable angles based on their anatomical structure and should be considered for LPI or followed with serial gonioscopy.
Primary angle closure and primary angle closure glaucoma
Patients that have at least 180 degrees of ITC and an elevated IOP or presence of PAS are classified as having primary angle closure (PAC). If glaucomatous optic neuropathy is present, then the patient has progressed to primary angle closure glaucoma (PACG).
Acute angle closure crisis
If the anterior chamber angle is obstructed suddenly, the IOP can rapidly rise to high levels and cause clinical signs and symptoms associated with high IOP. These patients are classified as undergoing an acute angle closure crisis. While an AACC may be self-limiting, it can recur, and the fellow eye is also at risk of an AACC. Several classes of drugs have the potential to trigger an AACC in one or both eyes.
Drug classes that can trigger AACC include:
- Adrenergic agents
- Anticholinergic agents
- Cholinergic agents
- Sulfa-based medications
- Anticoagulants
- Serotonergic agents4,5
Chua et al. found that topical mydriatics precipitated one in five cases of AACC in their study.6 Even so, the overall risk of patients developing an AACC after pupillary dilation is very low, reported occurring in only 0.03% of dilated patients.7
Acute ITC, recurrent ITC, and secondary angle closure
It’s important to note that iridotrabecular contact can occur acutely as in an AACC or chronically as in PACS, PAC, and PACG. All forms of ITC can lead to IOP elevation with subsequent
glaucomatous optic neuropathy. Recurrent angle closure can cause functional damage to the trabecular meshwork, leading to ocular hypertension even when ITC is resolved.
Both acute and chronic ITC can induce the formation of PAS, which, in turn, can further narrow the angle. An underlying pathology, such as iridocorneal epithelial syndrome, inflammation, neovascularization, or uveitis, can cause secondary angle closure.8
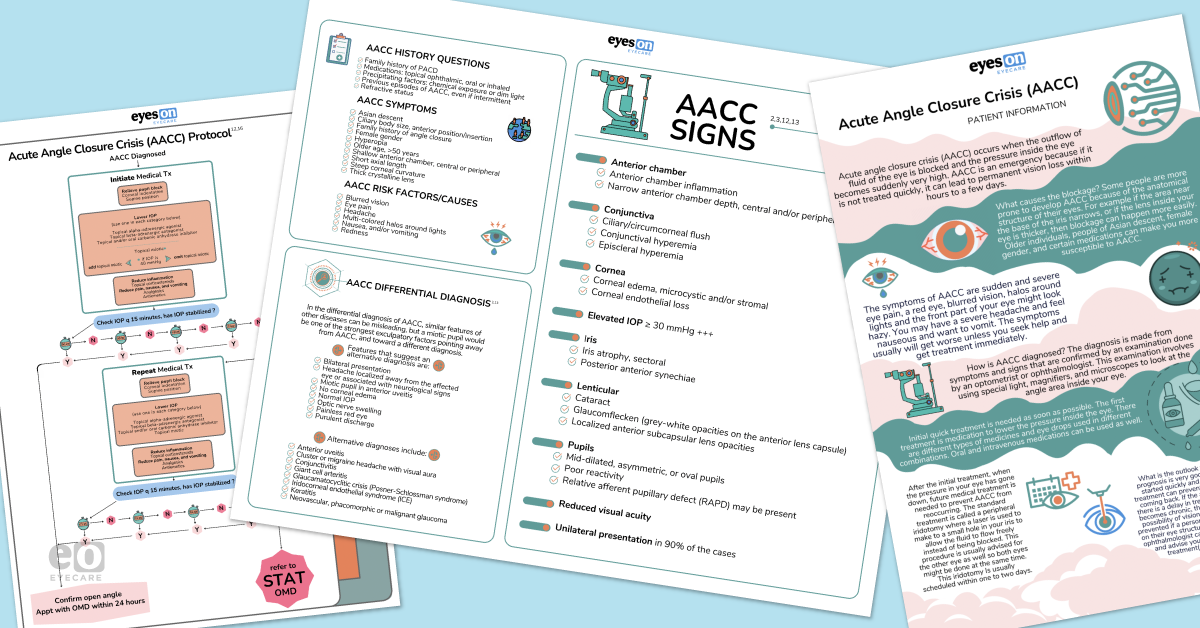
Download the Acute Angle Closure Crisis Protocol Cheat Sheet
📝
Acute Angle Closure Crisis Protocol Cheat Sheet
Use this cheat sheet and emergency kit as guides for treating an acute angle closure crisis.
Prevalence and demographics of primary angle closure
The considerable differences in the prevalence of PAC amongst ethnic and racial groups have been well documented, with the highest rates of PAC occurring in Innuit, Chinese, and other Asian populations.9
A recent review by Zhang et al. estimated that the global population of PACG was 17.14 million for people 40 years and older in 2020. Asia has the highest population, accounting for 70% of PACG worldwide. Their meta-analysis found three significant risk factors for PACG: female gender, older age, and Asian descent.10
Still, Day et al. noted that 0.4% of the European population over 40 years old had PACG. Their analysis suggested that PACG might be two to four times more common in the European population than estimated in previous studies.11
Risk factors for AACC
Demographic risk factors and causes of an AACC:
- Asian descent
- Ciliary body size, anterior position, and insertion
- Family history of angle closure2,3
- Female gender
- Hyperopia
- Older age, above 50 years old
- Shallow anterior chamber, central or peripheral
- Short axial length
- Steep corneal curvature
- Thick crystalline lens12,13
Presentation
The signs and symptoms of an AACC are the results of not only ultra-high levels of IOP but also the dramatic speed at which it occurs.
Symptoms of an AACC include:
- Blurred vision
- Eye pain
- Headache2
- Multi-colored halos around lights3
- Nausea and/or vomiting
- Redness12,13
Signs
Table 1 demonstrates further physiological signs optometrists can use to identify an AACC.2,3,12,13
Table 1, courtesy of Cindy Hui, OD
Diagnostic tests for AACC
Specific historical questions regarding family history, previous incidents, and especially precipitating factors are useful in diagnosing AACC.
Traits that can indicate a patient for an AACC include:
- Family history of PACD2
- Medications: topical ophthalmic, oral, or inhaled3
- Precipitating factors: chemical exposure or dim light
- Previous episodes of AACC, even if intermittent12
- Refractive status13
Differential diagnosis
Table 2 displays patient traits that indicate a differential diagnosis of an AACC.2,13
Table 2, courtesy of Cindy Hui, OD
Gonioscopy
Gonioscopy is the gold standard for diagnosis and should be performed on both eyes in any patient where an AACC is suspected. In particular, dynamic or compression gonioscopy helps to distinguish a truly closed angle from ITC or PAS. Performing
gonioscopy in a dark room helps bring out the angle features, but if visualization is further complicated by corneal edema, topical glycerin can be used to clear the cornea to obtain a better view.
2 Anterior segment imaging
Anterior segment imaging should be considered when a gonioscopy assessment is challenging, as there is good evidence demonstrating a general agreement between gonioscopy and anterior segment imaging findings.
Anterior segment optical coherence tomography (AS-OCT) uses long-wavelength, near-infrared light, while ultrasound biomicroscopy (UBM) utilizes ultrasound frequencies for imaging. Both techniques allow high-resolution visualization of the ocular architecture, especially the anterior chamber angles and structures concerning an AACC.
14,15 Treatment protocol for AACC
Treating the sequelae of an AACC involves immediately attending to the AACC, preventing the recurrence of an AACC in the affected eye, and preventing an AACC in the fellow eye.
While there are generalized protocols for urgent treatment of an AACC with a high variability of regimens with topical and systemic drug choices, overall treatment goals remain the same. Eyecare professionals should aim to eliminate pupil block, lower IOP,
reduce inflammation, and relieve patient symptoms of pain, nausea, and vomiting.
1) Relieve pupillary block
Corneal indentation
Corneal indentation (CI) can mechanically open the angle, forcing aqueous through the trabecular meshwork, thereby reducing IOP. Masselos et al. described this technique as a quick and effective way to reduce IOP in an AACC.19
Different instruments can be used to perform a CI, including a small-diameter gonioscopy lens, such as a four-mirror lens, a glass rod, or even a cotton-tipped applicator. When using a four-mirror lens, the technique suggested by Masselos et al. is achieved by applying 30 seconds of pressure on and then 30 seconds of pressure off. This is repeated for three to four cycles. The endpoint is identified when the trabecular meshwork is visualized post-indentation.19
Supine position
Having the patient lie flat on their back in the supine position can relieve the pupil block as it allows the lens iris diaphragm to move posteriorly with gravity, which may relieve some of the pupil block.20 The protocol developed by Choong et al. for their own clinic instructed their AACC patients to lie in the supine position for the entire time, other than when they were being tested.16
2) Lower IOP
To reduce the IOP as quickly as possible, the AACC protocol recommends using one drug in each category in a concerted effort, as each medication works with a different mechanism to lower IOP.2
Aqueous suppressants
Aqueous suppressants lower the IOP by blocking aqueous humor production. They include topical alpha-adrenergic agonists, topical beta-adrenergic antagonists, and carbonic anhydrase inhibitors (CAI).18
Topical alpha-adrenergic agonists:
- Apraclonidine 0.5%
- Brimonidine 0.2%
Apraclonidine is contraindicated in patients with severe, uncontrolled cardiovascular disease.
Topical beta-adrenergic antagonists:
- Timolol 0.5%
- Betaxolol 0.5%
Timolol is contraindicated in patients with pulmonary disorders, uncontrolled heart failure, and severe bradycardia. Betaxolol is the alternative drug of choice if timolol is not advised.18
Carbonic anhydrase inhibitors (CAI), topical, oral, and IV:
- Brinzolamide 1%
- Dorzolamide 2%
- Acetazolamide 500mg
- Methazolamide 100mg
Acetazolamide and brinzolamide should be avoided in patients with sulfonamide allergies and renal or hepatic impairment. Instead, oral methazolamide can be used in patients with kidney problems.18
Miotics
Miotics lower IOP by pulling the iris away from the trabecular meshwork.18
During an AACC, when the IOP is greater than or equal to 40mmHg, the pupillary sphincter muscle may be ischemic and unresponsive to topical miotic agents. Pilocarpine should not be administered until the IOP is less than or equal to 40mmHg.
Further, high concentrations of pilocarpine, such as pilocarpine 4%, can produce ciliary body thickening, increase vascular permeability and congestion of the iris, and push the iris lens diaphragm anteriorly, which aggravates pupil block. One hour after initiation of the AACC medical treatment, and when the IOP is less than or equal to 40mmHg, improved blood supply to the iris increases pilocarpine responsiveness. Pilocarpine should be administered at that time.18
Therefore, at the beginning of an AACC treatment, if the IOP is less than or equal to 40mmHg, administer pilocarpine 1 to 2%, two doses spaced 15 minutes apart. After 1 hour, and if the IOP is under 40mmHg, instill pilocarpine 1 to 2% every 15 to 60 minutes, up to a total of two to four doses maximum.18
Hyperosmotic agents
Lastly, hyperosmotic agents aid in deepening the
anterior chamber by dehydrating the vitreous.
18Hyperosmotic agents:
- Oral glycerol 1.0 to 1.5g/kg
- Oral isosorbide 1.5 to 2.0g/kg
- IV Mannitol 1 to 2g/kg (500ml of 20%)
Glycerol is contraindicated in patients with diabetes. Isosorbide is an alternative in diabetic patients. Mannitol is contraindicated in patients with renal failure, heart failure, pulmonary issues, or severe dehydration.
3) Reduce inflammation
Topical corticosteroids
To decrease inflammation, optometrists can recommend topical
corticosteroids to patients.
18Topical corticosteroids:
- Prednisolone 1%
- Loteprednol 0.5%
4) Relieve symptoms of pain, nausea, and vomiting
To relieve symptoms of pain, nausea, and vomiting in patients with AACC, optometrists can use analgesics and antiemetics.18
Medications for treating pain, nausea, and vomiting:
5) Tips for stabilizing an AACC
The AACC protocol involves treatment over a maximum 2-hour time window in which to stabilize the patient. Time starts after administering treatment, with an IOP status check every 15 to 30 minutes. If the IOP has not stabilized after one hour, then the second round of medical treatment is dispensed, with IOP status checks continuing for another hour.16
If the AACC is not successfully treated within the 2-hour time frame, the patient should be transferred immediately to an ophthalmologist.
An AACC is considered “broken” or stabilized when the IOP has returned to normal levels, the pupil is miotic, and the angle is open. Low IOP in itself is not indicative of stabilization; if the angle is not open, the IOP will rise again. Gonioscopy should be performed to confirm that the angle is indeed open. Once stabilized, the patient can then be transferred to an ophthalmologist within 24 hours for further care.
It is worth noting that normal or low IOP post-AACC is not well defined in the literature. The
American Optometric Association (AOA) believes the IOP target should be less than or equal to 20mmHg,
12 while other organizations define satisfactory IOP as less than or equal to 35mmHg, or a reduction of greater than 25% of the presenting IOP.
16Table 3 summarizes the goals, actions, and medications used in the AACC treatment protocol.2,16-18
Table 3, courtesy of Cindy Hui, OD
Consult an ophthalmologist within 24 hours
Once the AACC has been successfully averted, medical intervention should occur within 24 hours with the purpose of maintaining an open angle. Findings by Chua et al. observed that when patients did not present for medical attention until 3 days or more, later on the rate of
glaucoma increased from 22.6% to 60.8%.
6“Having the contact information for ophthalmologist referral with a map and directions, supports patient compliance with timely follow-up care.”
A study by David et al. found a statistically significant correlation between the delay of treatment and final outcome. Patients with less than a 24-hour delay after initial presentation had a more favorable outcome than those with 24 hours or more. They also found that the longer it took to terminate the AACC attack, the worse the long-term prognosis.21
Make a drop maintenance schedule
After the AACC has been neutralized, the patient should maintain a drop regimen until they are seen by an ophthalmologist for medical intervention. This maintenance drop regimen ensures that there is a reduction in aqueous production decrease in inflammation, an open angle is maintained, and prepares the patient for a laser peripheral iridotomy or other laser/surgical treatment.12
Post-AACC drop maintenance schedule:
- Topical beta-adrenergic antagonist (e.g., timolol 0.05% BID in the affected eye)
- Topical corticosteroid (e.g., prednisolone acetate 1% QID in the affected eye)
- Topical miotic (e.g., pilocarpine 2% QID OU)
Patient education
Patient and caregiver education is essential to successfully referring and transferring to an ophthalmologist for the continuation of medical care. The informational tools in the cheat sheet reinforce the importance of prompt follow-up care, prepare patient expectations on future procedures, and supports the patient throughout the entire process for the best possible outcome.
Follow-up and co-management of an AACC
Follow-up AACC treatment strategies
Once the patient presents for follow-up care, the ophthalmologist may perform various medical treatments depending on the AACC presentation.22
For a rapid reduction of high IOP
If the AACC treatment has not been successful, wherein the IOP is still high and/or pupil block remains present, many procedures are available for quick IOP reduction.
Medical procedures to rapidly reduce IOP caused by an AACC:
- Argon laser peripheral iridoplasty (ALPI) produces contraction burns at the peripheral iris causing an immediate deepening of the anterior chamber23
- Argon laser pupilloplasty (ALPP) is applied to the the iris surface of the pupillary dilator muscle and used in combination with other procedures, such as ALPI to achieve rapid reduction in IOP23
- Anterior chamber paracentesis performed with a paracentesis slit knife or 30-gauge needle
- Diode laser transscleral cyclophotocoagulation (DLTSC) is a possible alternative that lowers IOP rapidly and reduces corneal edema
- Micropulse transscleral cyclophotocoagulation is another alternative with a strong safety profile
For eliminating a pupil block after reducing IOP
Once the AACC has been overcome, the ophthalmologist may choose one or several methods with the aim of the treatment to prevent future angle closure by eliminating the pupil block mechanism.
Surgical procedures used to eliminate the pupil block mechanism:
- Surgical peripheral iridectomy
- Laser peripheral iridotomy
- Cataract extraction or clear lens exchange
Adjunctive procedures performed in combination with lens extraction:
- Phacoemulsification with goniosynechialysis can be less traumatic as the viscoelastic breaks down PAS with viscoelastic with fewer complications18
- Endoscopic cyclophotocoagulation (ECP) targets the ciliary body directly and achieves IOP lowering by reducing aqueous production
For controlling IOP
After the AACC, if the ophthalmologist notes persisting poor control of IOP, a combined phacotrabeculectomy might be considered.
Co-management
First follow-up 1 week after an AACC
After the initial postoperative exam for a medical AACC procedure,
such as after an LPI, a follow-up examination should be performed within 1 to 7 days.
12What to evaluate at the 1-week follow-up:
- Confirm iridotomy patency
- Assess IOP control
- Corroborate open anterior chamber angle
Subsequent 1-month follow-up
After 1 month, use a dilated fundus exam to check:
Repeat monthly follow-ups
As most iridotomy closures occur within the first 2 to 6 months, routine monthly evaluations should be conducted.12
At subsequent monthly follow-ups, monitor:
Long-term follow-ups
Long-term follow-up of patients who have undergone LPI is recommended every 6 to 12 months.12
Conclusion
AACC is a true ocular emergency, and knowledge of AACC and the exact treatment protocol allows effective and immediate action to prevent vision loss. In fact, having an AACC emergency kit in the optometric office would be beneficial for any practice, as all the supplies and resources would be collected and ready for use.