Ocular emergencies can show up at any place or time, and it’s important for eye doctors to be up to the challenge of diagnosing and treating them. An ophthalmic emergency is anything that can threaten vision within a short period of time. Certain types of emergencies may be more time-sensitive than others, but all need to be taken care of in an efficient manner. Here, we will discuss different types of traumatic ophthalmic emergencies that may show up in your clinic.
Corneal abrasion
Exam findings
- Epithelial defect that stains with NaFl
- No infiltrate
- May have underlying corneal edema
- May have mild anterior chamber reaction
Treatment
- Use of topical prophylactic antibiotic drops or ointment 4 times daily.
- Bandage contact lens should be utilized only if the patient reliable and defect is sterile.
Keep an eye out for the development of an infiltrate or worsening anterior chamber cell as these can be signs of a corneal ulcer.
Case 1: Corneal abrasion
The patient in Figure 1 developed a
corneal abrasion after removing his contact lenses from his eyes. He developed significant and immediate pain, tearing, and photophobia. Fortunately, there was no evidence of infection and the condition resolved well with prophylactic antibiotics.
Figure 1: Contributed by author.
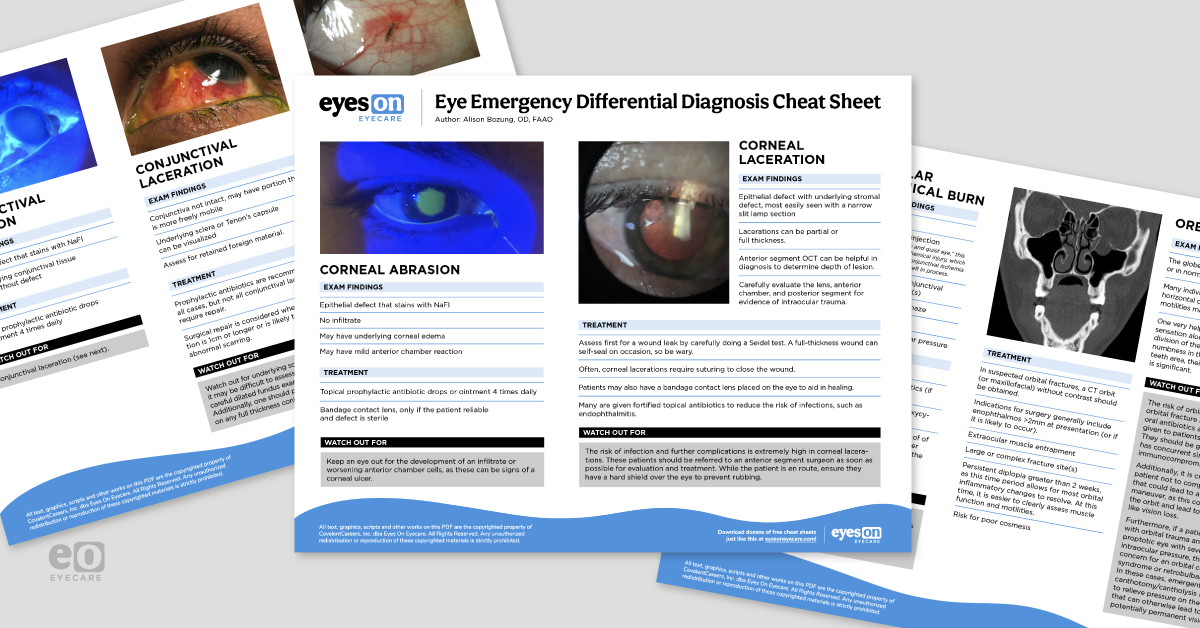
To give you all the information from this article in an easy-to-access format, we have created an Eye Emergency Differential Diagnosis Cheat Sheet.
Download the cheat sheet now!
Eye Emergency Differential Diagnosis Cheat Sheet
Utilize this cheat sheet with side-by-side comparisons of common traumatic ocular emergencies.
Corneal laceration
Exam findings
Treatment
- Assess first for a wound leak by carefully doing a Seidel test. A full-thickness wound can self-seal on occasion, so be wary.
- Often, corneal lacerations require suturing to close the wound.
- Patients may also have a bandage contact lens placed on the eye to aid in healing.
- Many are given fortified topical antibiotics to reduce the risk of infection/endophthalmitis.
The risk of infection and further complications is extremely high in corneal lacerations. These patients should be referred to an
anterior segment ophthalmologist as soon as possible for evaluation and treatment. While the patient is en route, ensure they have a hard shield over the eye to prevent rubbing.
Case 2: Corneal laceration
In Figure 2, a middle-aged patient was working on construction when a metal nail flew up striking him in the eye. The patient thought the nail was stuck “to the contact lens” and removed it himself prior to presentation. The patient was diagnosed with a self-sealing, full-thickness corneal laceration. In the left photo, you can see a wound that passes through the entire thickness of the cornea. On retro-illumination in the right image, you can visualize a focal
cataract that developed due to violation of the lens capsule when the nail entered the eye. The wound was Seidel positive, and the surgery was done to close the corneal wound as well as remove the lens due to the capsule violation.
An
intraocular lens was placed in the sulcus at the time of surgery. The patient was given intravitreal antibiotics, a tetanus shot, and started on fortified antibiotic drops due to the nature of the unjust. At last follow up, his vision was 20/20 with spectacle correction.
Figure 2: Contributed by author.
Traumatic iritis
Blunt trauma to the eye may cause inflammation, most often seen in the anterior chamber. The most common symptoms of traumatic iritis or hyphema are photophobia, pain, and
redness of the eye. Traumatic iritis occurs when direct trauma to the eye results in inflammation of the iris tissue and subsequent release of white blood cells, proteins, and other inflammatory mediators into the anterior chamber.
Exam findings
- White blood cells and haziness (flare) in anterior chamber
- Occasionally, a hypopyon can form if severe
- Traumatic mydriasis possible
Treatment
- Topical corticosteroids (QID to Q2h)
- Cycloplegic agents (BID to TID)
- Patients may also take pain-relieving medications as needed.
Evaluate for iris damage such as iris sphincter tears leading to traumatic mydriasis. It is important to document and educate the patient about this so they are aware the pupil may be large permanently, even after discontinuation of cycloplegics.
Case 3: Traumatic iritis
The patient in Figure 3, with traumatic iritis, presented with redness, photophobia, and pain of his eye. On examination, you can visualize white blood cells and flare in the anterior chamber.
Figure 3: Contributed by author.
Traumatic hyphema
Exam findings
Traumatic hyphemas can be caused by the same mechanism as traumatic iritis, but they more often manifest with iris damage which leads to hemorrhage.
- A microhyphema consists of suspended red blood cells in the aqueous humor.
- A “classic” hyphema reveals layered blood inside the anterior chamber.
Treatment
Medications
- Topical corticosteroids (QID to Q2h)
- Cycloplegic agents (BID to TID)
Additional
- Patients should be advised to reduce or eliminate strenuous activity.
- Patching the patient's eye during sleep prevents rubbing, and sleeping with their head elevated can help keep blood out of the visual axis.
- It is generally not necessary to stop blood thinners, but if pain relief is needed, non-blood thinning agents such as acetaminophen are generally preferred.
Elevated intraocular pressure is relatively common in hyphemas, and the risk increases with the grade of hyphema. Watch the IOP carefully and treat with aqueous suppressants when needed. In patients of African or Middle-Eastern descent, it may be prudent to assess for
sickle cell disease or trait, as these individuals have a higher chance of uncontrolled IOP. Patients with uncontrolled IOPs or evidence of corneal blood staining (seen as a golden hazy coloration of the posterior stroma due to severely elevated IOP with hyphema) may need a surgical AC washout.
Traumatic hyphemas increase the risk of angle recession and traumatic glaucoma, so be sure to do
gonioscopy once the eye has healed from its acute trauma and the blood has completely cleared (generally recommended to wait 1 month). Continue to follow these patients at least on a yearly basis as elevated intraocular pressure may present weeks or even years later.
Case 4: Traumatic hyphema
This teenage male presented after being hit in the eye with a friend’s swinging cell phone charger. He presented with an interesting location of his small hyphema, located temporally, suspected due to sleeping position the night prior.
Figure 4: Contributed by author.
Conjunctival abrasion
The conjunctiva may be a source of injury, particularly with sharp objects. A conjunctival abrasion occurs when there is damage to the epithelial cell layer only. This type of injury is relatively common and should not lead to any negative long term effects. A conjunctival laceration occurs when there is deeper injury, so caution should be exercised to rule out penetrating damage.
Exam finding
- Epithelial defect stains with NaFl.
- The underlying conjunctival tissue is intact without defect.
Treatment
Treatment consists of topical prophylactic antibiotic drops or ointment 4 times daily. With conjunctival abrasion, you should always be aware of the possibility of conjunctival laceration.
Conjunctival laceration
Exam findings
- Conjunctiva is not intact, may have portion that is more freely mobile.
- Underlying sclera or Tenon’s capsule can be visualized.
- Assess for retained foreign material.
Treatment
Treatment consists of prophylactic antibiotics, which is recommended in all cases; not all conjunctival lacerations require repair. Surgical repair is considered when the laceration is 1cm or longer or is likely to lead to abnormal scarring.
Watch out for underlying scleral laceration; it may be difficult to assess initially, but a careful dilated fundus exam is critical. Additionally, one should perform a Seidel test on any full thickness conjunctival laceration.
Case 5: Conjunctival laceration
In this case, the patient presented with a full thickness conjunctival laceration after the metal tip of a flat-edge screwdriver struck him directly in the eye. The conjunctiva had partially retracted back and was thickened. There was no underlying scleral wound, and the dilated exam was unremarkable. Though the defect was over 10mm long, the patient opted to forgo repair. He healed without infection, but there was a thick ridge of conjunctival scarring remaining.
Figure 5: Contributed by author.
Conjunctival foreign body
For conjunctival foreign bodies, an exam will detect material embedded under the conjunctiva. In addition, there will be NaFl staining at the entry site if injury is recent. Recommended treatment involves removal of the foreign body after application of topical anesthetic and a prescription for prophylactic antibiotics.
Before removing a bulbar subconjunctival foreign body, ensure there is NO scleral penetration. Complete dilated fundus exam and use a Seidel test to assess the area before removal.
Case 6: Conjunctival foreign body
This male patient presented after a vehicle tire exploded near his face while he was working. Here, you can see a rod-shaped foreign body in the subconjunctival space. Fortunately, he did not have any globe penetrating trauma. The foreign body was removed without complication at the slit lamp.
Figure 6: Contributed by author.
Orbital fracture
Orbital fractures can occur as a result of head or direct ophthalmic trauma. The most common causes of orbital fractures include sports-related injuries, motor vehicle accidents, altercations, and falls in the elderly. Patients will often present with a history of trauma, pain with or without eye movement, periocular swelling and ecchymosis, and
double vision.
Exam findings
- The globe can be proptotic, enophthalmic, or in normal position.
- Many individuals will complain of horizontal or vertical diplopia, and the motilities may be limited.
- One very helpful clue is assessing sensation along the V2 nerve (maxillary division of the trigeminal)–if a patient has numbness in that area, their chance of a floor fracture is significant.
Treatment
- In suspected orbital fractures, a CT orbit (or maxillofacial) without contrast should be obtained.
- Indications for surgery generally include: enophthalmos >2mm at presentation (or if it is likely to occur).
- Extraocular muscle entrapment.
- Large or complex fracture site(s).
- Persistent diplopia greater than 2 weeks, as this time period allows for most orbital inflammatory changes to resolve. At this time, it is easier to clearly assess muscle function and motilities.
- Risk for poor cosmesis.
The risk of orbital cellulitis after orbital fracture is quite low, however, oral antibiotics are still frequently given to patients for prophylaxis. They should be given if the patient has concurrent sinus infection or is immunocompromised. Additionally, it is critical to advise the patient not to complete any activities that could lead to a Valsalva-like maneuver, as this could force air into the orbit and lead to complications like vision loss.
Furthermore, if a patient presents with orbital trauma and has a proptotic eye with severely elevated intraocular pressure, there is a high concern for an orbital compartment syndrome or retrobulbar hematoma. In these cases, emergent
surgical canthotomy/cantholysis is required to relieve pressure on the optic nerve that can otherwise lead to acute and potentially permanent
vision loss.
Case 7: Orbital fracture
This patient presented with pain on eye movement, eyelid swelling, and limited upgaze of the left eye. He reported recent trauma during an altercation. He endorsed numbness of the skin on the left maxillary dermatome when compared simultaneously to the right side. CT imaging reveals a left orbital floor fracture without any muscle entrapment. He did not require immediate surgery, and he failed to return for his 2 week follow up.
Figure 7: Contributed by author.
Ocular chemical burns
Chemical burns of the eye are generally divided into two categories: acidic and alkaline. While both can be very detrimental to the ocular surface, alkaline chemicals are considered to have a higher chance of more severe injury due to their ability to saponify cellular lipid membranes and penetrate further into tissue. Regardless of the chemical, it is critical to check the pH of the eye(s) immediately and begin irrigation. The severity of the injury can be determined by utilizing widely available via the Roper-Hall classification scheme or the more updated Dua classification from 2001.
Exam findings
- Pain
- Conjunctival injection
- Corneal and conjunctival epithelial defect(s)
- Corneal haze
- Symblepharon
- Elevated intraocular pressure
Treatment
Treatment depends on the level of injury.
Case 8: Ocular chemical burns
This male presented for emergency eye care after exposure to an alkaline substance in the left eye. Here you can see the diffuse chemosis (left) along with a large area of epithelial loss highlighted by sodium fluorescein dye (right). The pH was 9 on arrival, and the patient’s eye was irrigated multiple times to normalize the ph to 7.
Figure 8: Contributed by author.
In summary
Optometrists often serve as the frontline in eye emergencies. Remember the importance of quickly triaging the emergency, obtaining a complete history, and thoroughly evaluating the eye. With a solid understanding of ophthalmic emergencies and a methodical approach, any eye doctor can feel confident either directly managing or appropriately referring—whatever comes through the door!