Pseudophakic cystoid macular edema (PCME), also referred to as Irvine-Gass Syndrome, is characterized by
swelling of the macula due to fluid accumulation, typically occurring a few weeks to months following cataract surgery. It has been found to be the most common complication of
cataract surgery, as well as the most common cause of decreased visual acuity following cataract surgery. The prevalence of PCME is somewhat difficult to determine, as various studies define it differently.
PCME and cataract surgery
Furthermore, the incidence of this clinical entity continues to decrease with ever-improving cataract surgery techniques leading to potentially fewer complications. As we know from our clinical practice and from the literature, PCME is invariably subclinical and self-limiting but can become chronic in patients, resulting in some level of permanent vision loss.1,2
Pathogenesis and risk factors for PCME
While the exact mechanism for PCME is still debated, there is a consensus that increased vascular permeability due to inflammatory mediators, such as prostaglandins, seems to be the most likely culprit. It has been postulated that other factors, such as
vitreomacular traction (VMT) and light toxicity, can also play a role.
3Unsurprisingly, patients with increased postoperative inflammation, like those that experience more complicated surgery, tend to develop PCME more frequently and perhaps worse than those with minimal inflammation.
Ocular and systemic conditions have also been found in studies to increase the risk of PCME. Diabetes stands out as the most common risk factor with an increased propensity towards developing PCME, which ladders up with
diabetic retinopathy severity. Also, some reports have found an increased risk of PCME in patients using prostaglandin analogs for glaucoma, but this is not yet well established.
2Risk factors for PCME include:4,5
PCME diagnostic tools
Traditional methods for the evaluation of cystoid macular edema (CME), as well as PCME, include slit-lamp biomicroscopy, indirect ophthalmoscopy, and
fundus photography. However, mild edema can be very difficult to appreciate, depending on the extent of the edema and the eyecare practitioner’s experience. Therefore, methods such as FA and OCT have shown greater utility in patients with decreased visual acuity.
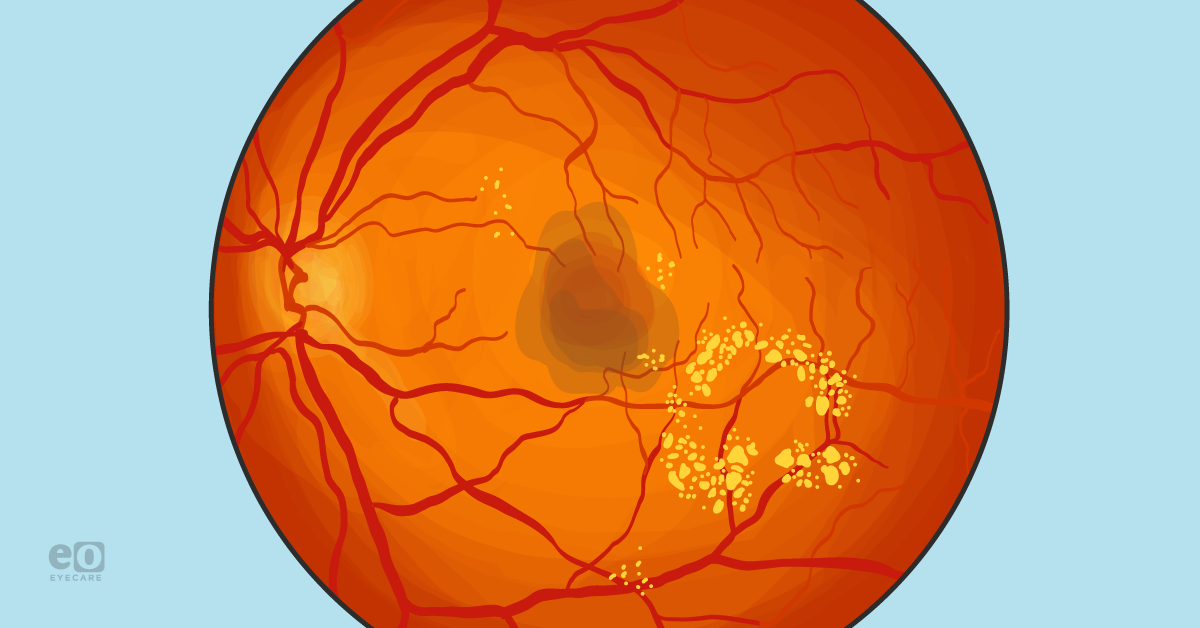
Fluorescein angiography
Traditional FA can demonstrate fluorescein leakage in a characteristic petaloid pattern without optic nerve involvement.6,7
Figure 1 is fluorescein angiography imaging showing fluorescein that leaked into the patient’s macular area.
Figure 1, Image courtesy of Mohammad Rafieertary, OD, FAAO
Optical coherence tomography
In recent years, OCT has become the
standard diagnostic tool for identifying PCMEs due to its non-invasive nature and widespread accessibility. Taking it one step further, the advent of spectral domain and swept source technologies has transformed two key areas: image acquisition time and image quality.
“These significant leaps forward improve the ability to discriminate fine details and potentially lead to earlier treatment in these patients.”
Additionally, OCT can be used as a
tool for progression analysis to quantitatively monitor a patient’s response to treatment. However, it should be noted that the amount of fluid leakage and edema observed does not always correlate with visual acuity.
6,7Figure 2 shows an OCT image of a patient with macular thickening, as well as cystic spaces, in both the inner nuclear and outer plexiform layers. This is coupled with a pigment epithelial detachment with overt inner/outer segment junction disruption.
Figure 2, Image courtesy of Mohammad Rafieertary, OD, FAAO
Fundus autofluorescence
Lastly, some recent studies have advocated for the use of
fundus autofluorescence (FAF), a non-invasive imaging technique that evaluates lipofuscin release within the retina using various filters and wavelengths of light.
Similar to traditional FA imaging, a petaloid-like pattern is typical to observe in vivo. Two important caveats to note are that this technique is not as widely adopted, and it may not be as sensitive as either of the previously mentioned methods.8
PCME prevention
In a perfect world, the prevention of PCME would include the least-invasive surgery with minimal complications, short surgery time, and the nominal use of anti-inflammatory topical medication to manage postoperative pain and inflammation. There is some debate regarding what is the best agent used postoperatively—is it topical steroids, non-steroidal anti-inflammatory drugs (NSAIDs), or both?
“Since the current rate of PCME is relatively low, it has been a challenge in studies to statistically prove one agent holds an advantage over the other.”
Studies seem to indicate that the prophylactic use of anti-inflammatory drugs—whether steroids, NSAIDs, or both—after surgery improves short-term visual prognosis. However, using these agents does not appear to affect long-term visual outcomes. The use of these medications in high-risk patients, such as
patients with diabetes or other known risk factors, may be more beneficial.
9Treatment for PCME
As a reminder, the rate of PCME is relatively low with
modern cataract surgery. However, when it happens, it can occur weeks to months after surgery and is often associated with suboptimal vision. Corticosteroids and topical NSAIDS are generally the first lines of treatment for PCME, either individually or in combination.
One accepted management strategy would be to initiate treatment with a generic NSAID and topical corticosteroid and then potentially switch to a more expensive, branded topical NSAID if there is no vision improvement after 4 to 6 weeks.10
In certain persistent cases, referral to an ophthalmologist would be warranted for a retina consult to potentially perform an intravitreal injection of corticosteroids or
anti-VEGF agents when medically necessary.
Treating chronic PCME
In eyes with chronic PCME, an ophthalmologist might consider performing a pars plana vitrectomy (PPV), especially if there is concurrent vitreomacular traction.9,10 Oral acetazolamide might be utilized as a secondary treatment in patients who are unresponsive to steroids and/or NSAIDs but is not widely used.10
“We recommend having a collaborative relationship with your local comprehensive ophthalmologist and retina colleagues when you deem these cases might need surgical intervention.”
It should be noted that while NSAIDS have been approved for the treatment of PCME, their use beyond 14 days may result in corneal epithelial breakdown, corneal thinning, corneal erosion,
corneal ulceration, or perforation. Further, both topical and intravitreal steroids have been associated with increased intraocular pressure (IOP) when used either on- or off-label. This means that eyecare practitioners should monitor these patients carefully for IOP spikes at follow-up visits.
9PCME case report
A 77-year-old Caucasian male presented with a chief complaint of worsening vision in both eyes (OU) following
cataract surgery 6 months ago. The patient’s systemic history was significant for diabetes mellitus type II,
hypertension, atrial fibrillation, and hyperlipidemia.
The patient’s ocular history was significant for large physiological optic nerve cupping OU and, more recently, pseudophakia with posterior chamber intraocular lens implants (PCIOL) OU. Unaided entering acuities were 20/60 right eye (OD) and 20/20 left eye (OS), with no improvement on pinhole or refraction. Additionally, entrance examination revealed pupils were equal and reactive to light OU, confrontation visual fields were full to finger counting OU, and extraocular muscles were full and unrestricted OU.
A slit lamp examination showed that anterior segment findings were within normal limits OU with Goldmann applanation tonometry measured 10mmHg OU. The dilated fundoscopic evaluation showed well-centered and clear lens implants OU, C/D ratios 0.4 round OD and 0.5 round OS, and
mild non-proliferative diabetic retinopathy OU.
Macular OCT was performed due to decreased best-corrected visual acuity OD, displaying intraretinal
cystic spaces consistent with cystoid macular edema in the right eye of variable size. There was also a slight distension of the outer plexiform layer and a mostly unremarkable scan in the left eye, with the exception of a likely recent posterior vitreous detachment (noted subtle hyper-reflectance in the foveal center).
Figure 3 demonstrates OCT imaging highlighting intraretinal cystic spaces.
Figure 3, Provided by Steven Ferrucci, OD, FAAO
Figure 4 shows OCT imaging highlighting a posterior vitreous detachment.
Figure 4, Provided by Steven Ferrucci, OD, FAAO
Based on the patient's chief complaint, coupled with the proximity in the timing of the symptoms to his cataract removal, it was suspected that the etiology of the edema was secondary to surgery, although diabetic macular edema could not be completely ruled out. The patient was initiated on ketorolac tromethamine 0.5% QID OD and prednisolone acetate 1% QID OD for 1 month. At the 1-month follow-up visit, the patient reported visual improvement with unaided entering acuities of 20/20 OD and OS.
Consequently, the follow-up macular OCT found complete resolution of cystoid macular edema, leading us to taper off his topical medications.
Figure 5 features OCT imaging demonstrating a full resolution of the pseudophakic cystoid macular edema.
Figure 5, Provided by Steven Ferrucci, OD, FAAO
Conclusion
While less common in the era of modern cataract surgery, PCME still remains the leading cause of suboptimal vision in the weeks to months
following cataract surgery. Both the prevention and treatment revolve around the use of topical anti-inflammatories, either NSAIDs, steroids, or a combination thereof.
Eyecare practitioners should always suspect the presence of PCME in patients with decreased vision following cataract surgery, especially if there are any associated risk factors identified throughout the examination.