Dysphotopsias are divided into two categories: positive dysphotopsias (PD) and negative dysphotopsias (ND). Positive dysphotopsia is generally described as a bright artifact of light (arcs, streaks, halos, rings, or starburst) occurring centrally or mid-peripherally. Negative dysphotopsia is often described as the absence of light, which can manifest in the form of a dark, temporal arching shadow.
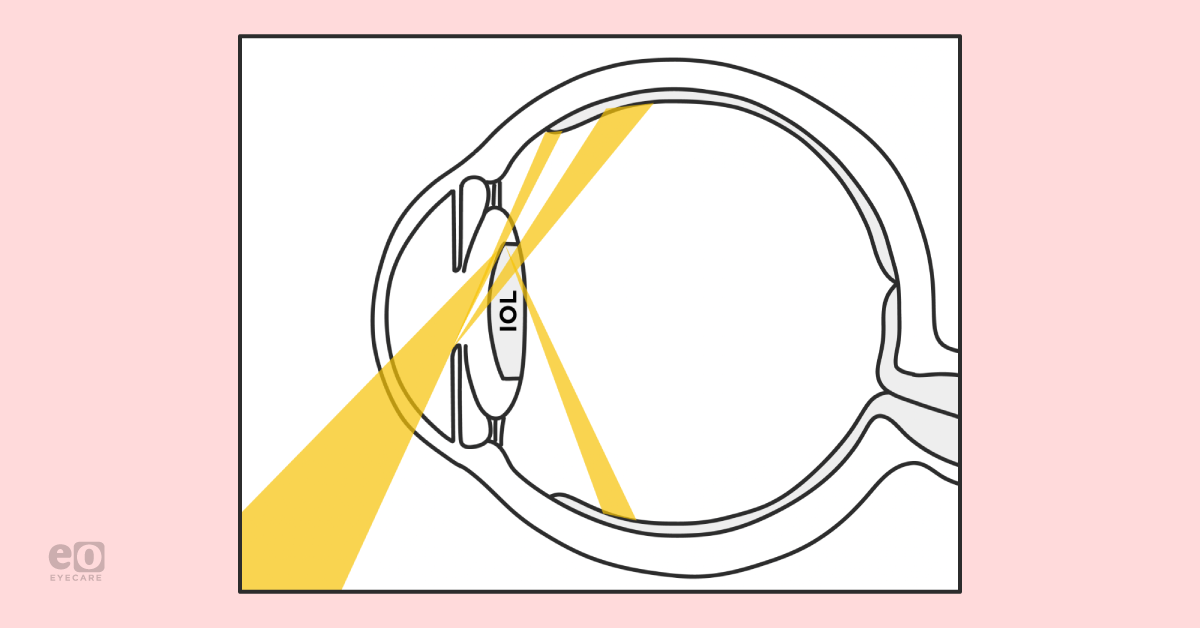
Figure 1 illustrates the mechanism by which oblique light source can cause positive or negative dysphotopsia.
Figure 1
Prevalence of dysphotopsia
Some studies have shown that up to 1 in 2 patients will experience some form of dysphotopsia at some time after
cataract surgery with about 20% of patients reporting dysphotopsias on postoperative day 1.
1, 2What causes positive dysphotopsia (PD)?
There are a few major causes of PD:
Edge design
Edge design of the
intraocular lens (IOL) has been demonstrated to be the primary factor in causing PD. Prior to the 1990s, rigid polymethyl methacrylate (PMMA) was basically the only IOL available and had smooth rounded edges. The edge design changed with the advent of foldable IOLs.
Square or truncated edge IOLs reflect light onto the retina, especially when that light enters the eye at an oblique angle. The optical principle was likely the same in the old PMMA IOLs but the rounded edge scattered the light over a larger area of the retina and therefore usually wasn’t perceived by patients. In fact, the first report of PD was not until 1993,3 though PMMAs had been in use for many decades, further confirming that edge design is a primary driver of PD.
Unfortunately this means there has been a tradeoff, decreasing risk of PCO but increasing risk for PD. This design is unlikely to go away because of how effectively squared or truncated edge IOLs prevent PCO.4
IOL material
The IOL edge design plays a greater role in causing PD than the material or shape of the IOL. With this being said, Masket and Fram have reported success with exchanging IOLs for patients suffering from chronic PD, with a success rate >85% when replacing acrylic IOL with silicone or copolymer.5
Other factors that have been found to contribute to PD include a high index of reflection (I/R) and high surface reflectivity.4
What causes negative dysphotopsia (ND)?
While the causes of PD are mostly well understood the causes of ND are multifactorial and have been somewhat of a mystery, though recent optical modeling in the laboratory has helped clarify factors involved in ND.
IOL placement
Holladay and Simpson helped shed light on causative factors of ND with ray-tracing techniques that model the
pseudophakic eye. They found a sort of “illumination gap” is perceived when there is a gap between the light refracted by the nasal edge of the IOL onto the nasal retina and the light that slips between the iris and the lens onto the nasal retina. This is seen as a temporally located crescent or arc shaped shadow.
6 The nasal bridge prevents this phenomenon from occurring on the temporal retina which is why patients are much less likely, if at all, to report ND occuring in the nasal visual fields.
Frustratingly for both patient and surgeon, ND is more likely to occur more with a “perfect” cataract surgery–one with perfect centration, perfect capsulorrhexis overlap of the lens and an immaculate posterior capsule.5 ND only occurs with in-the-bag IOL implantation and has not been reported to occur with any other IOL placement, such as ciliary sulcus, anterior chamber, or scleral-fixated IOLs.
Other factors
Unlike PD, IOL material or shape is not likely to be a major component of ND. Laboratory modeling has suggested that these and other factors, such as smaller pupils, large positive angle kappa, steep posterior IOL, short axial distance of IOL behind iris, and nasal anterior capsule overlying the IOL, may contribute to ND.6 Some interventions target these factors with some success as discussed below.
Recent studies by Masket et al. show that ND may also have a neurological component. ND scotomas, confirmed by Goldmann visual field were reduced in 4 out of 5 patients when the contralateral eye was occluded indicating that there is more to this condition than just the retinal illumination gap, though the illumination gap is probably a prerequisite to the neurological component.7, 8
We can be certain there is still much to learn about ND, and the body of knowledge on the condition will grow as time goes on.
Positive dysphotopsia: what you need to know
Patients can complain of unwanted images, such as streaks, arcs, flickers, flashes or starbursts. Importantly, these are elicited by an external light source, often obliquely placed.
Vitreoretinal traction can cause similar symptoms but will be present without external light.
4Figure 2 shows an example of streaks, arcs, flare, flashes or starbursts that can be experienced by patients reporting positive dysphotopsia.
Figure 2 "Night Street" by mrhayata is licensed under CC BY-SA 2.0.
Testing for positive dysphotopsia
Almost by definition, dysphotopsia is something the patient can see but that you cannot see, as a result, there is no objectively reliable test for PD. Clinicians must rely on subjective symptoms as reported by the patient.
Positive dysphotopsia treatment
For both PD and ND it is important to understand that most symptoms should be given the chance to resolve on their own (and most in fact do). Over time, in a process called neuroadaptation the brain will gradually adapt by ridding unwanted visual stimuli from perception.9 Examples of this include the blind spot created by the optic nerve or refractive phenomena that occur through the natural pupil or lens. A new IOL adds another ingredient to the mix. This leads to the first point:
Patient education
Once other causes of the visual complaints have been ruled out, reassure your patient and provide counseling regarding neuroadaptation. They may have visited several other providers before you and were told they were perfectly fine, which is frustrating since they know what they see! However, at this point they may be so fixated on the unwanted image(s) that it may be difficult for neuroadaptation to take place.
Use of miotics
Time
Neuroadaptation takes time (months), and unfortunately is less likely to occur with PD than ND. However, if several months to a year have passed, and miotics have already been trialed, consider…
Lens exchange
Of course, exchange for rigid PMMA can also be performed but is generally avoided as this would require a larger 7mm incision.5 It is important to note that YAG capsulotomy would make IOL exchange more challenging; it is prudent to rule out PD as a cause for a patient reporting visual complaints before prematurely performing a YAG capsulotomy for PCO.
And again… patient education
Unfortunately, for a minority of patients, nothing will alleviate their unwanted symptoms. Understand that it may not be possible to completely eliminate unwanted visual symptoms for every patient. In these cases, make sure you are on the same page, and that they have an understanding of what is happening. While there is no guarantee, at the very least they will see the lengths you have gone to help solve their problem and have an appreciation for your efforts.
Negative dysphotopsia: what you need to know
Common patient complaint
Most patients describe a dark arc or crescent shaped shadow located temporally.
Figure 3 is an example of temporal scotomas experienced by patients reporting negative dysphotopsia.
Figure 3: Provided by Matthew Chang, MD
Testing for negative dysphotopsia
Goldmann kinetic testing can be used for objective evaluation in patients with ND. One study found that patients with ND demonstrate
constricted visual fields or temporal scotomas that correspond to the position of the reported shadow.
7,8 However, like PD, clinicians rely mostly on subjective reporting by patients.
Negative dysphotopsia treatment
Similar to the above treatment of PD, conservative management is attempted first as most symptoms resolve within the first several weeks after surgery. The incidence decreases from around 20% after surgery to 3% at 1 year.1,2 Alongside reassurance and neuroadaptation counseling, patients can try glasses with a thick temple piece to block light from the side that is stimulating ND.
One study found that inferotemporal placement of the IOL haptic caused a 2.3x decrease in incidence of ND on postoperative Day 1. However this was no longer statistically significant after postoperative Week 1.10
One article references occluding the affected eye for a few weeks as a way to cure ND.11
YAG capsulotomy
If conservative management fails, the least invasive intervention is removal of the nasally located anterior capsule. This may help by eliminating the reflection of the anterior capsulotomy edge on the nasal retina or by decreasing iris-to-IOL distance, which reduces the previously discussed retinal illumination gap.9 This has been reported to be 60% successful.6
Piggyback IOL
If the above fails, a sulcus IOL may be placed. A sulcus IOL theoretically helps by scattering light at the nasal edge of the IOL which prevents a shadow from forming on the retina.12 This has been reported to be around 80% successful in a small sample size.12
Reverse optic capture
In this intervention the IOL edge is raised above the lip of the anterior capsule while the haptics remain in the bag. This method of resolving ND has been supported both clinically and through laboratory modeling.13 Be aware that the optic may still slip back into the bag and lead to recurrence of symptoms. In addition, in this situation, the posterior IOL edge is no longer inhibiting epithelial cell migration; this may lead to accelerated PCO development.
Nasal IOL truncation
Alapati et al. reported a case of one patient with recurrence of ND after reverse optic capture. They amputated the nasal optic edge in a so-called “in-the-bag nasal IOL optic truncation” which completely resolved symptoms. They believe that the truncated edge causes increased light scatter and eliminates the retinal shadow in ND.14
IOL exchange
Finally, as a last resort, IOL exchange can be considered. So far the literature reports mixed results, with various materials or edge designs used to varying effect. This further supports the primary theory that the position of the lens may be more important than what materials it is made from.9,13
Patient education
Again, just like with PD, it may not be possible to completely eliminate unwanted visual symptoms for every patient. Reassurance and counseling is key to maintaining a strong physician-patient relationship.
Patient recommendations (especially for night driving and halos)
Before cataract surgery, it is important to proactively counsel patients on the potential for unwanted images. As mentioned above, most symptoms of dysphotopsia will resolve with time.
Postoperatively, sometimes the most important action is to simply listen to a patient's frustrations and concerns. Telling patients they have had a perfect cataract surgery may only aggravate them and inhibit neuroadaptation as they focus on distracting symptoms with no explainable cause. Residual refractive error and
dry eye disease can also be a cause of unwanted images and should be treated.
Patients who place independence from glasses at near and intermediate distance of prime importance, and who would prefer a multifocal IOL, should be especially cautioned about glare and halos especially during night driving. These are a type of diffractive dysphotopsia separate from PD and ND discussed above.
What is currently being done to reduce risk of dysphotopsia?
To reduce the risk of dysphotopsia some changes that have been made in the ophthalmic industry include creating thinner square edged IOLs, leaving the IOL edge unpolished, moving optical power to the anterior portion of the optic, and rounding the anterior part of the IOL edge. Unfortunately, since the posterior square edge on the IOL is still present, while these changes may be beneficial, the incidence of PD still remains significant.4
Specific IOLs for ND have been designed with a groove on the anterior edge designed to capture the
anterior capsulotomy. In this way the optic overlaps over the capsule rather than the capsule overlapping the optic which is similar to the reverse optic capture technique. In Europe, this as well as two other IOLs that employ capsulotomy fixation have not had any reports of ND in clinical trials.
4,15References
- Bournas P, Drazinos S, Kanellas D, Arvanitis M, Vaikoussis E. Dysphotopsia after cataract surgery: comparison of four different intraocular lenses. Ophthalmologica. 2007;221(6):378-383. doi:10.1159/000107496
- Osher RH. Negative dysphotopsia: long-term study and possible explanation for transient symptoms. J Cataract Refract Surg. 2008;34(10):1699-1707. doi:10.1016/j.jcrs.2008.06.026
- Masket S, Geraghty E, Crandall AS, et al. Undesired light images associated with ovoid intraocular lenses. J Cataract Refract Surg. 1993;19(6):690-694. doi:10.1016/s0886-3350(13)80336-7
- Masket S, Fram NR. Pseudophakic Dysphotopsia: Review of Incidence, Cause, and Treatment of Positive and Negative Dysphotopsia. Ophthalmology. 2021;128(11):e195-e205. doi:10.1016/j.ophtha.2020.08.009
- Masket S, Rupnick Z, Fram NR, Kwong S, McLachlan J. Surgical management of positive dysphotopsia: U.S. perspective. J Cataract Refract Surg. 2020;46(11):1474-1479. doi:10.1097/j.jcrs.0000000000000307
- Holladay JT, Simpson MJ. Negative dysphotopsia: Causes and rationale for prevention and treatment. J Cataract Refract Surg. 2017;43(2):263-275. doi:10.1016/j.jcrs.2016.11.049
- Makhotkina NY, Berendschot TT, Nuijts RM. Objective evaluation of negative dysphotopsia with Goldmann kinetic perimetry. J Cataract Refract Surg. 2016;42(11):1626-1633. doi:10.1016/j.jcrs.2016.09.016
- Masket S, Magdolna Rupnik Z, Fram NR, Vikesland RJ. Binocular Goldmann visual field testing of negative dysphotopsia. J Cataract Refract Surg. 2020;46(1):147-148. doi:10.1097/j.jcrs.0000000000000001Wenzel M, Langenbucher A, Eppig T. Ursachen, Diagnose und Therapie der negativen Dysphotopsie [Causes, Diagnosis and Therapy of Negative Dysphotopsia]. Klin Monbl Augenheilkd. 2019;236(6):767-776. doi:10.1055/s-0043-112855
- Hu J, Sella R, Afshari NA. Dysphotopsia: a multifaceted optic phenomenon. Curr Opin Ophthalmol. 2018;29(1):61-68. doi:10.1097/ICU.0000000000000447
- Henderson BA, Yi DH, Constantine JB, Geneva II. New preventative approach for negative dysphotopsia. J Cataract Refract Surg. 2016;42(10):1449-1455. doi:10.1016/j.jcrs.2016.08.02
- Wenzel M, Langenbucher A, Eppig T. Ursachen, Diagnose und Therapie der negativen Dysphotopsie [Causes, Diagnosis and Therapy of Negative Dysphotopsia]. Klin Monbl Augenheilkd. 2019;236(6):767-776. doi:10.1055/s-0043-112855
- Makhotkina NY, Dugrain V, Purchase D, Berendschot TTJM, Nuijts RMMA. Effect of supplementary implantation of a sulcus-fixated intraocular lens in patients with negative dysphotopsia. J Cataract Refract Surg. 2018;44(2):209-218. doi:10.1016/j.jcrs.2017.11.013
- Henderson BA, Geneva II. Negative dysphotopsia: A perfect storm. J Cataract Refract Surg. 2015;41(10):2291-2312. doi:10.1016/j.jcrs.2015.09.002
- Alapati NM, Harocopos GJ, Sheybani A. In-the-bag nasal intraocular lens optic truncation for treatment of negative dysphotopsia. J Cataract Refract Surg. 2016;42(12):1702-1706. doi:10.1016/j.jcrs.2016.11.002
- Masket S. Development of an anti-dysphotopic IOL. Exp Rev Ophthalmol. 2018. https://doi.org/10.1080/17469899.2018. 1560263.Figure 3 is an example of temporal scotomas experienced by patients reporting negative dysphotopsia.