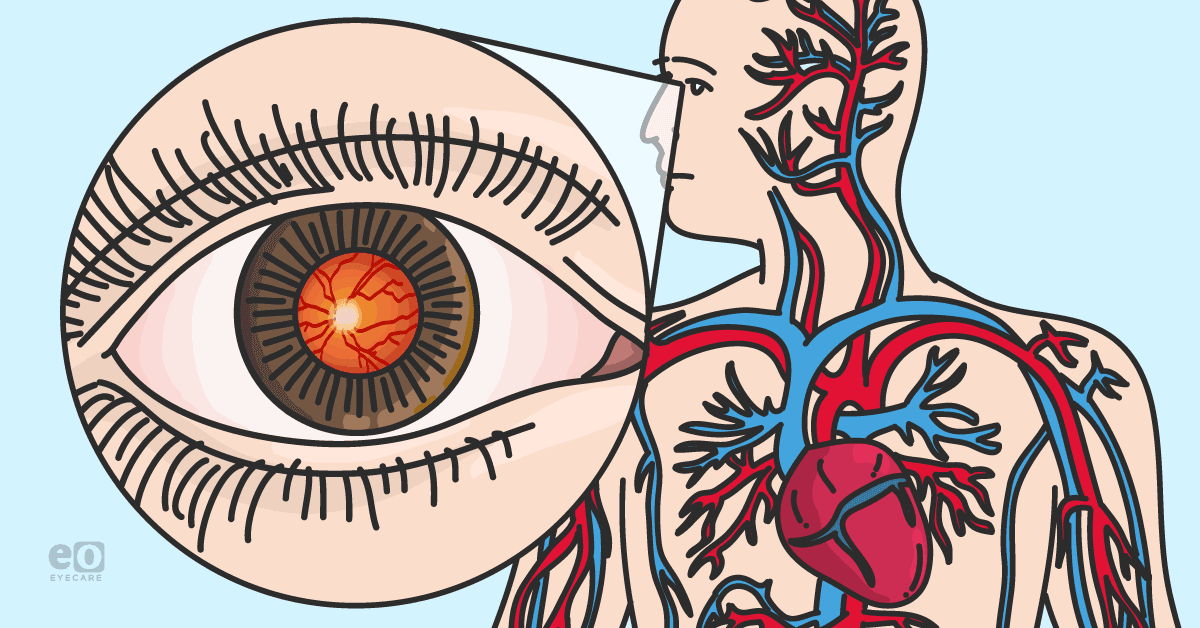
The eyes are a window to a patient’s systemic health. Optometrists must consider the overall health status of each patient to understand how their health can impact their eyes and vision.
This article will give an overview of common non-ophthalmic diseases that optometrists might encounter during a comprehensive eye exam. It will review how these non-ophthalmic conditions are, in fact, relevant to optometrists because of their ocular manifestations as well as how to address them and/ or make an appropriate referral.
Diabetes
Diabetes is well recognized as a systemic condition with potential for ocular involvement, in fact, it is the leading cause of blindness in working adults. The likelihood of ocular manifestations correlates directly to the length of time since diagnosis; a 10% chance of ocular complications after 15 years and 75% chance of ocular manifestations after 20 years. Whether or not the patient is treated with insulin and the patient’s overall glycemic control are also correlated to the likelihood of diabetic eye disease.
Additional risk factors for developing diabetic retinopathy include concurrent obesity, hypertension, and smoking history. For those reasons, the aforenoted are the few pertinent points to incorporate in case history for a diabetic patient.1
Primary care physicians and endocrinologists often refer patients for an annual retinal exam and in that case, they may have no related symptoms. If a diabetic patient is experiencing vision blur (despite best refractive correction) this could be suggestive of several possible complications. Firstly, diabetes does accelerate cataract development, and if this is the case a patient may complain of consistent blur, increased glare, and light sensitivity along with vision not feeling “crisp.”
If the complaint is more of a fluctuating blur (sometimes a patient will report that their glasses “seem to work better” than other times), it is important to ask the patient if this seems to correspond to their glycemic level; they may be experiencing a temporary refractive shift (if it is a phakic patient) due to uncontrolled blood sugar levels.
Patients who have diabetic retinopathy could potentially present with an array of symptoms ranging from none to blurred or distorted vision or vision loss in severe cases. Diabetic retinopathy (Figure 1) may impact vision through presence of macular edema, or in more moderate-severe cases vitreous hemorrhaging or tractional retinal detachment.
Figure 1: Photo courtesy of Kevin Cornwell, OD
A complete, dilated ocular health exam will uncover and differentiate these signs and symptoms. Imaging modalities such as OCT to detect macular edema or fundus photography to document and monitor diabetic retinopathy are indicated as appropriate. All diabetic patients should be educated on the importance of blood sugar level control in prevention of sight threatening complications.
Those without any sign of retinopathy are advised to follow up in 1-2 years. Those patients who do have signs of mild retinopathy may be asked to follow up in 6 months to a year and more frequently if moderate retinopathy is present. If moderate-severe or severe non-proliferative retinopathy or any suspicion of proliferative retinopathy or macular edema is present this warrants prompt referral to a retinal specialist for likely fluorescein angiography and treatment.2 If concerning diabetic eye signs are noted, it would also be recommended to get in contact with the patient’s primary care provider and/or endocrinologist.
Hypertension
Patients with hypertension are commonly encountered in the optometry exam lane since about 30% of Americans have this diagnosis.3 Uncontrolled hypertension increases the risk of several ocular conditions including retinal artery and vein occlusions, non-arteritic ischemic optic neuropathy, and retinal hemorrhaging. Hypertension also increases the risk of age-related macular degeneration (Figure 2), thyroid eye disease, and diabetic retinopathy.4 On case history, time since diagnosis should be investigated along with compliance to treatment regimen and additional risk factors such as alcohol/tobacco use and family history.3
Figure 2: Photo courtesy of Kevin Cornwell, OD.
Changes to the retinal blood vessels are what lead to ocular manifestations and complications; this occurs in 3 stages:
- During the vasoconstrictive phase, attenuation of the retinal arterioles can be observed on fundus exam.
- During the second phase, the sclerotic phase, further blood vessel shape and coloration changes are noted. These are crossing changes, further narrowing of retinal arterioles and copper and silver wiring appearance.
- The third phase, when the blood-retinal barrier has been broken, can manifest clinically as exudates, hemorrhaging, and cotton wool spots. In severe cases of malignant hypertension bilateral disc edema can be present.3
Symptoms of hypertensive patients presenting for an optometry exam can vary based on the severity. They may range from no symptoms/signs at all to blurred vision or vision loss. Ocular findings can include retinal hemorrhaging or exudation as well as disc edema (typically associated with new headaches and visual blur/distortion). If the latter is the case, the patient’s blood pressure should be taken to confirm then the patient should be referred STAT to the emergency department.3
All hypertensive patients should receive a routine dilated fundus exam with appropriate imaging studies as indicated. Blood pressure should be taken as part of the optometric exam for all hypertensive patients (if possible) and certainly for any patient manifesting with retinal changes from hypertension.
All patients with hypertension should be educated on the importance of blood pressure control in prevention of sight-threatening complications. It is also important to co-manage and communicate with the patient’s primary care physician if increased blood pressure or concerning ocular signs should arise.
Hyperlipidemia and carotid artery stenosis
Hyperlipidemia is very common among patients since approximately 30% of Americans have this condition. It is often concurrent with diabetes and/or hypertension. Cholesterol plaques can be extremely dangerous because they can break off (often from the carotid artery) and travel to distal retinal arterioles where they block blood flow. Patients experiencing this may report transient vision loss (amaurosis fugax) along with the transient ischemic attack (TIA).
Aside from the increased risk of plaques, hyperlipidemia can also lead to lipid build up along the walls of retinal blood vessels. This can lead to slowed, hypoperfused flow or temporary lack of perfusion altogether. Clinically this can manifest as ocular ischemic syndrome with patients typically reporting unilateral reduced vision with ocular pain. Dilated fundus exam would show mid-peripheral unilateral hemorrhages 360 degrees on the side of the patient with substantial carotid artery stenosis.5
Patients with hyperlipidemia and/or carotid stenosis disease should be counseled on regular follow ups with their cardiologist and/or vascular surgeon. They should also be educated on the signs and symptoms of TIA and advised to return promptly for evaluation should they occur.
Autoimmune and inflammatory diseases
Autoimmune and inflammatory diseases such as systemic lupus erythematosus and rheumatoid arthritis can be commonly encountered in the primary care optometrist’s office. In addition, others such as spondyloarthropathies, sarcoidosis, Sjogren’s syndrome and inflammatory bowel disease can exhibit the same or similar presentations. Ocular manifestations can range from ocular surface disease to posterior segment disease; therefore, it is important to keep this medical history in mind throughout the entirety of your ocular health exam.
Anterior segment conditions associated with autoimmune disease include dry eye syndrome, keratitis, episcleritis and uveitis.6 Ocular surface disease can present with symptoms of redness, burning, irritation, tearing, foreign body sensation and/or light sensitivity if keratitis is present. These can be managed with traditional methods of a lubrication regimen, punctal plugs, environmental alterations and possibly a low-dose steroid regimen.
Anti-inflammatory medications such as cyclosporine (Restasis, Cequa) or lifitegrast, (Xiidra) work particularly well in this group since aqueous deficient dry eye secondary to lacrimal gland dysfunction is often the cause. In severe cases, serum tears, eyelid surgery, and scleral contact lenses may be considered.7
Patients presenting with uveitis will most often complain of blurred vision, aching eye pain, and light sensitivity. This condition can be unilateral, bilateral, and/or recurrent and treated with anti-inflammatory therapy. Posterior segment (more severe) signs include scleritis, vitritis, choroiditis, vasculitis, and macular edema. These conditions require systemic anti-inflammatory treatment, co-management with retina specialists, internists and sometimes even hospitalization. The impact of these conditions is not limited to the eye and similar effects are often concurrently found in other body systems requiring prompt intervention.8
When discussing these conditions during patient history, it is important to also inquire as to medications being used for treatment. Therapy with Plaquenil or methotrexate, for example, can have ocular implications of their own (macular and optic nerve disease) and require regular monitoring.
Neurologic conditions
Roughly 60% of patients with a history of stroke have some form of residual vision impairment.9 Patients with a history of stroke can have visual field defects, hence making the visual field an important part of the optometric exam. This can give the doctor information about where the infarct occurred and important information about how the patient may be functioning.
Visual field deficits, such as hemianopia, can impact a patient’s everyday tasks like ambulation and reading.10 Field loss can also instigate visual midline shift syndrome in some patients which is an alteration in spatial awareness.9 Having a stroke can also impair eye teaming and fusion abilities and with visual perception and processing. A patient with stroke history may be co-managed with a neurologist and neuro-optometrist if vision therapy is indicated.
The signs of acute stroke can include diplopia and vision loss along with confusion, slurred speech, hemi facial and/or paralysis of one side of the body. Any of these signs will warrant immediate medical attention.9
Multiple sclerosis is a demyelinating disorder that often has ophthalmic manifestations; more than half of people living with this condition experience a related eye issue at some point in their life.11 Optic neuritis is most common and often presents alongside symptoms of blurred or dimming vision and pain on eye movement. While visual acuity can recover to its original level in some cases, however some patient’s do experience vision loss, color vision changes and contrast sensitivity loss after an episode.
Multiple Sclerosis can also affect ocular motility resulting in nystagmus or internuclear ophthalmoplegia which could present with symptoms of diplopia, blur, oscillopsia and difficulty reading. Examination testing on patients with multiple sclerosis should include monocular color vision testing, optic nerve studies such as OCT, and visual field testing to determine blind spot enlargement (especially if optic neuritis is suspected).
Careful analysis of extraocular motility is also crucial.12 It is important to remember that optic neuritis can also be retro-bulbar and if suspected based on patient history and symptoms, referral or co-management with a neurologist or neuro-ophthalmologist is appropriate.
Thyroid disease
Thyroid gland disorders have an incidence of almost 20% in the female population and 13% in the male population.13 Grave’s disease (leading to hyperthyroidism) and Hashimoto’s thyroiditis (leading to hypothyroidism) are the two most common thyroid conditions. Thyroid Eye Disease (TED) is an autoimmune condition where ocular tissue is attacked; it is most associated with hyperthyroidism but can also be present with euthyroid or hypothyroid states.14
Ocular signs can include puffiness around the eyes, proptotic appearance due to eyelid retraction, dry eye and irritation (especially if exposure issues are present). More severe signs can include proposis, involvement of extraocular muscles causing restricted motilities, and/or diplopia, severe corneal disease, or superior limbic keratopathy. In very severe cases, compression of the optic nerve can occur and result in optic neuropathy. It is important to remember that the ocular signs do not always correlate with severity of disease state.14
When taking the medical history of a patient with Grave’s disease, it is very important to ask about a history of smoking since this significantly increases the risk of ocular disease. Stress and hypertension have also been linked to increased severity of TED.14 Treatment for ocular surface disease is the most common intervention required. If more severe disease is present where extraocular muscles are involved, the optic nerve is threatened, or strabismus is induced, decompression surgery by a specialist is recommended. Strabismus and eyelid surgeries may also be indicated.14,15
Conclusion
Diabetes, hypertension, high cholesterol, neurologic disease, autoimmune disease, and thyroid disease are a few of the more commonly encountered systemic health conditions our patients may be diagnosed with. It is important for optometrists to take information gathered on medical history and know the clinical correlates so that we can inquire as to specific signs or symptoms that may suggest ocular involvement.
Furthermore, optometrists should understand what the potential serious ocular consequences are of these systemic conditions and when to refer or co-manage patients. This will provide patients with the most successful outcomes.