It seems as though
scleral lenses are finding their way into articles, blogs, lectures, and journals now more than ever, and for good reason. Even though these lenses have been around since the late 19th century, our understanding of their benefits and, in turn, their utilization has seemed to skyrocket in the last handful of years. In this article, we will review just a few of the numerous indications for scleral lens fitting, as well as discuss some tips and pearls.
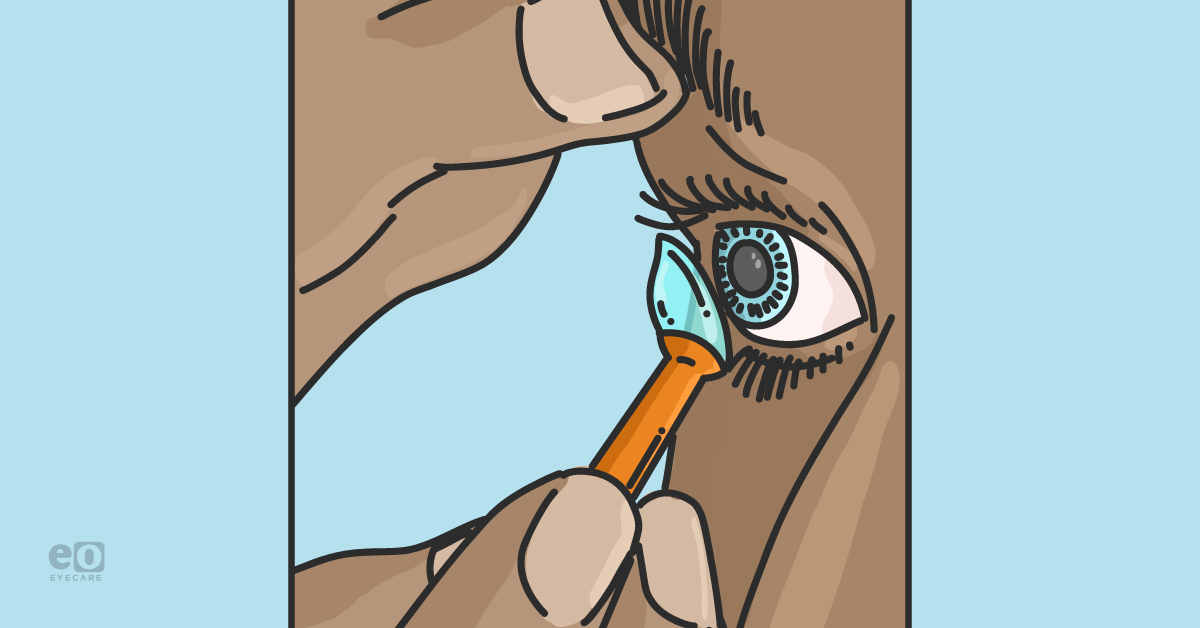
Scleral lens fitting basics
The
early steps of a scleral lens fit include careful ocular health assessment, measuring refraction, and deciding how the lenses will be ordered. Fitting sets are available from a number of scleral lens brands such as
Zenlens,
Custom Stable,
Jupiter, and
Onefit, to name a few. Each fitting set will typically have its own recommendations for selecting a starting lens, and these typically rely on the previously-mentioned keratometry measurements, shape selection (prolate or oblate lenses), and the measurement of the horizontal visible iris diameter (HVID). Lenses can also be fit using empirical measurements, scleral profilometry, or impression-based molds.
“These more advanced methods can yield amazing fitting results and can reduce the number of remakes needed to reach a satisfactory fit.”
Whether you’re a student learning about scleral lenses in class or you’ve been fitting them for years in practice, these lenses can seem intimidating at times. I regularly tell patients that one reason these lenses require a dedication of time during their fitting is that a standard
soft contact lens can be adjusted in about four or five parameters, while there are easily triple this many options when it comes to tinkering with a scleral lens fit. They are extremely customizable and have many uses, so let’s get into five conditions to manage with scleral lenses.
1. Primary corneal ectasia
The two primary corneal ectasias a practitioner may run into are
keratoconus (KC) and pellucid marginal degeneration (PMD). These conditions involve an inflammatory and progressive thinning process of the cornea that causes anterior protrusion and the development of irregular astigmatism, visual aberrations,
scarring, and other compounding issues.
1“Opinions may vary, but one of the ‘bread and butter’ conditions to tackle with a scleral lens is keratoconus.”
Depending on the severity, these patients may not have adequate vision with their current glasses or other forms of contact lenses, and their vision quality may have the potential to be greatly improved with the optics provided by a scleral lens. The best way to determine the visual improvement from a scleral lens is to simply put one on.
Pearl #1: Choosing the lens shape, prolate or oblate, largely depends on the location of the cone or ectasia. If the cone is central or slightly inferior, as is classic, a prolate lens can be a great choice. In cases of ectasia where the protrusion is peripheral, such as post-refractive, oblate lenses are typically my first lens of choice.
Figure 1 features corneal topographical maps that illustrate keratoconus.
Figure 1: Image courtesy of Alex Tharman, OD
2. Post-refractive surgery corneal ectasia
Corneal ectasia can also follow procedures such as
laser-assisted in situ keratomileusis (LASIK), photorefractive keratectomy (PRK), or radial keratotomy (RK). These patients are typically used to a certain level of vision quality that has degraded since the time of their surgery, and their motivation to return to that previous clarity can be high.
Progression of ectasias is something that should be measured and monitored; this can usually best be done with topographical mapping, though it’s worth remembering that ectasias can show the earliest changes on the corneal back surface. Measuring these changes would require
tomography scans, and if that cannot be done at your office, I would suggest referring to another provider to obtain that information.
Pearl #2: As with refractive surgery itself, centration of the treatment area is critical when trying to obtain the best quality of vision possible. The more complex the scleral design, the more important centration becomes.
Figure 2: Image courtesy of Alex Tharman, OD
3. High astigmatism or ametropia
When it comes to large prescriptions or significant amounts of astigmatism, we all know that
contact lenses can provide better vision for patients with less image distortion. The spectacle lenses can also have moderate weight or lens thicknesses which pushes patients to wear their contacts.
“Because of this, soft lenses are an easy go-to, though at a certain point they too have their limits.”
Contact lens manufacturers vary, but lens options start to become significantly thinner past sphere powers of +12.00 diopters (D) and -15.00D, and cylinders of -2.75D, not to mention the need for
presbyopic correction (if applicable). Again, the scleral lens can offer a great amount of customization in this realm as well. Prescriptions can be fine-tuned in quarter steps, unlike many commercial soft lenses, all while providing exceptional stability in eyes with difficult corneal shapes to fit by using a lens that contours the surface rather than vault it.
Pearl #3: Performing an autorefraction after allowing a patient’s lens(es) time to settle can really speed up the refraction process. Remember, because of the “tear lens” provided by the scleral lens, their initial prescription may not be remotely close to the prescription needed in the scleral lens.
Figure 3 shows topographical maps that demonstrate eyes with moderate regular astigmatism.
Figure 3: Courtesy of Alex Tharman, OD
4. Ocular surface disease
The spectrum of ocular surface disease severity is vast and ranges from superficial punctate keratitis (SPK) all the way to Stevens-Johnson syndrome. For these patients, the main concern or reason for a scleral lens fit is the
optimization of their ocular health, while the vision improvement is icing on the cake or negligible for some.
“As with all scleral lens cases, but especially for patients with ocular surface disease, the fit of the lens is extremely important.”
The lens diameter needs to be well considered, and if we’re trying to cover conjunctival tissue, a larger lens should be chosen than if we were simply trying to protect the cornea.
2 For patients with ocular surface disease, the lens is there to protect the surface itself. These patients may still need to overcome
symptoms of dryness or improve lens comfort because there are other missing pieces of the puzzle. This can include care of their lids, ocular inflammation, and giving consideration to the solutions used in their scleral wear and care.
Pearl #4: Stain, stain, stain. A little fluorescein can go a long way in assessing the fit of a scleral lens. Dye on the eye itself upon lens removal can highlight areas of corneal touch, edema, dryness, lens compression, or other complications of surface disease or poor fit. Dye placed under the lens can help visualize the lens vault, and when the strip is applied on top of a lens, we can better understand the wetting dynamics of the lens or scleral edge lift.
Figure 4 shows the corneal staining for the eyes of a patient using scleral lenses with diffuse SPK and mild compression rings.
Figure 4: Image courtesy of Alex Tharman, OD
5. Post-corneal transplant
Full-thickness
corneal transplants can demonstrate incredible amounts of visual distortion and irregular surfaces. These eyes may have undergone the procedure of a full corneal transplant for a number of different reasons, but their management afterward is imperative when it comes to preserving their new tissue.
In patients who underwent a penetrating keratoplasty (PK), maintaining the graft integrity and health is vital.3 Careful attention should be paid to any sutures left in place and, of course, the junction where the host and donor tissue meet. These cases should be followed closely, and keeping their corneal specialist in the loop and involved is also beneficial.
Pearl #5: Oxygen transmissibility is a key consideration with grafts since there can be less tear exchange than in other lens modalities. It’s usually best to take advantage of high Dk materials when available, keep the lens as thin as possible, and trending clearance on the shallower side while not comprising the graft.
Rapid-fire pearls
The name of the game with scleral lenses is normally to clear the cornea, but by how much is a question whose answer can have a good deal of variation. The bottom line is the “correct” amount of clearance is the amount the patient does well with from a vision and health perspective.
“Some patients require more clearance for vision benefits or to allow for more lens settling through the day, while other eyes will tolerate less clearance just fine.”
While it can be a great joy to see these patients’ lives improved through the vision or comfort provided by scleral lenses, we should also keep in mind other aspects of the management of each individual case. For example, the current initial standard of managing keratoconus progression is moving towards
corneal collagen crosslinking (CXL), and if progression is noted after this, we need to consider other options to stop this change if possible.
Of course, no treatment plan, contact lenses included, comes without risks. It is always important to understand what may occur in cases of contact lens misuse, improper wear or care, or the effects a poor fit may have and how to manage these incidents.
4 These complications can be nasty, but there are helpful resources available that outline
good management protocols should they arise.
5Final thoughts
Now you’re ready to get out there and start addressing some of the above conditions through the
use of scleral lenses. Patients that fall into the above groups are surely already in your practice, and if they’re not yet, they will be. Even if you as a practitioner don’t fit scleral lenses, understanding the many ways they can be utilized will better help you serve your patients.