Scleral lenses have gained popularity as a valuable therapeutic option for management of corneal irregularity, ocular surface disease, and post-surgical corneas. These large diameter rigid gas permeable lenses vault the entire cornea and limbus with a fluid reservoir that helps hydrate the cornea and protects the ocular surface against the mechanical shearing forces of the eyelids, making them an ideal option for treating ocular surface diseases.
With advancements in technology and improvements in material availability, sclerals are now available in higher oxygen permeability (Dk) materials, different lens coatings, and can be designed with front and back surface toricity, peripheral elevations such as microvaults, notches, and 3-D mapping techniques for a precise fit and optimal patient comfort.
In Figure 1, the image on the left shows a large-scleral lens 18mm in diameter, whereas the image on the right shows a 14.8mm diameter mini-scleral lens.
Figure 1
Fitting philosophy
Scleral lenses are primarily fit on sagittal depth instead of traditional keratometric values.
1 Diagnostic fittings can help expedite the fitting process and can provide valuable information on parameter modifications required for an optimal fit. When initiating a diagnostic fit, it is important to select an appropriate lens that vaults the cornea with an initial corneal vault of 200-250 microns and limbal vault of 100 microns. It has been reported that for a lens thickness of 250 microns, a 200 microns central clearance and 50 microns limbal clearance optimizes oxygen transmission to the cornea.
3 This is key when working with patients with endothelial compromise given the risk of corneal edema with scleral lens wear.
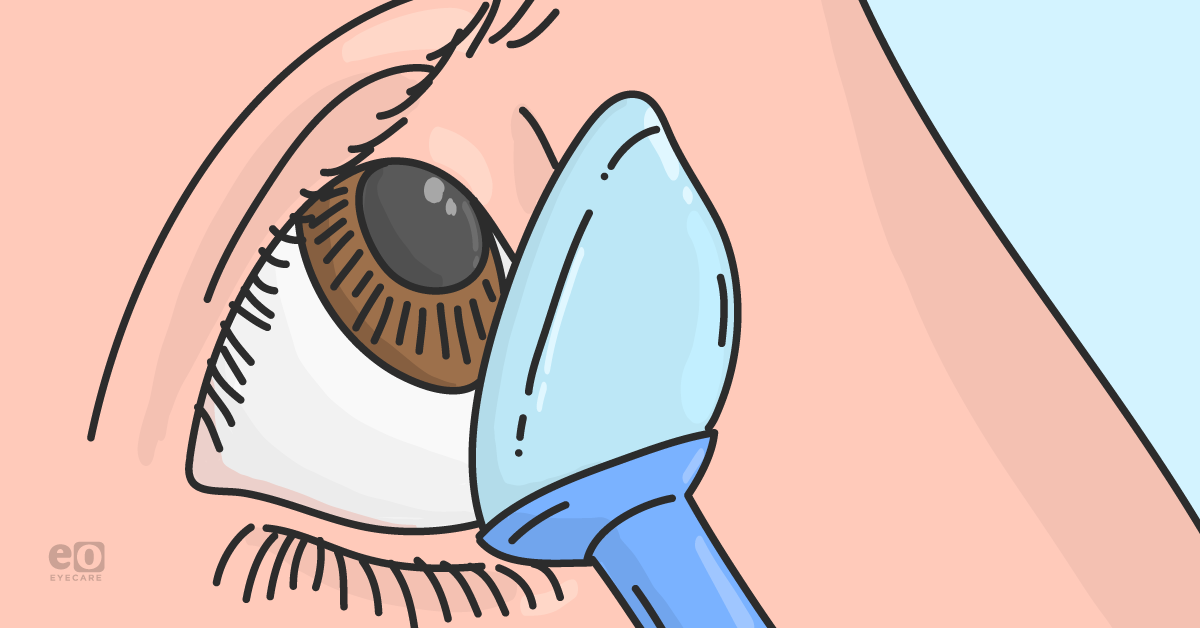
Figure 2 illustrates an optic section of a scleral lens over the cornea showing an optimal clearance for a fluid reservoir.
Figure 2
These large diameter lenses do have a tendency to settle on the eye, so allowing 30 minutes to an hour of settling in the clinic before examining the lens can help maximize information needed for making appropriate lens changes, especially for the lens haptic. While the lens may look like a good fit at initial application, the fitting might change as the lens sinks into the conjunctiva tissue post-settling. Once the lens settles, the scleral lens haptic should be evaluated to ensure that it is well aligned with the sclera and to avoid any impingement or blanching of the blood vessels.
In cases of toric haptics, assessing the position of toric markings helps assess stability of the lens on the eye.
Selecting lens parameters
Diameter
Horizontal visible iris diameter (HVID) can be used as a starting point for diameter selection. Starting with a lens that is 4-5mm larger than the HVID can help achieve a sufficient clearance over the limbus. Patients with conditions like megalocornea or a larger HVID may require a larger scleral lens diameter to avoid bearing on the limbus.
In addition, when working with patients with an advanced ectatic cornea in the mid-peripheral area, it can be challenging to vault the peripheral corneal elevations. In such cases, larger diameter lenses can achieve a sufficient vault to clear the peripheral cornea and allow for an even weight distribution at the landing zone.1,2,4
Scleral haptics
Sclera is non-rotationally symmetrical with increasing asymmetry past the corneal apex. Mini-sclerals fit closer to the limbus and are less prone to having issues with a mismatch between scleral toricity and lens haptic. However, when working with large diameter lenses, a toric or quadrant specific haptic can help achieve a better scleral alignment as it provides an even bearing across the scleral surface. In cases of improper toricity, patients exhibit issues such as blanching or fogging in the tear reservoir.1,2,4
In Figure 3, blanching or compression of conjunctival blood vessels can be noted at the lens edge. In such cases, flattening the landing zone can alleviate the concern.
Figure 3
Blanching results from localized pressure from the scleral haptic that reduces conjunctival blood flow. Adding toricity to the lens haptic can help with reducing compression of the conjunctiva blood vessels. When blanching is noted at the lens edge, flattening the haptic can resolve the issue (Figure 3). However, in cases where compression is noted under the scleral lens landing zone closer to limbus, it indicates a heel-toe effect where the scleral lens lands too harshly on the conjunctiva resulting in hyperemia. Steepening the haptic can alleviate compression and can achieve a smoother lens landing.1,2
Over-refraction
When assessing vision with a trial scleral lens, it is helpful to begin with an auto-refraction measurement over the lens. It can be used as the starting point for manifest over-refraction. A sphero-cylindrical over-refraction is often useful to assess the best visual potential for the patient and to rule out concerns with flexure.
Residual
astigmatism can result from two different factors: internal or lenticular cylinder and flexure. A quick way to identify the root cause is by performing topography over the scleral lens. If there is astigmatism detected over the lens, flexure is the culprit. However, in a well-fitted lens, if there is no astigmatism noted on topography over the lens, then the cause of residual astigmatism is true lenticular astigmatism. In cases of true lenticular cylinder, front surface toricity can help correct the refractive issue.
Another option to minimize flexure is by altering lens thickness, however, it does reduce oxygen transmissibility to the cornea which should be taken into consideration.1,5,6
Indications
Keratoconus
Keratoconus is a bilateral, asymmetric, progressive ectasia that results in corneal steepening and irregular astigmatism.
7,8 Corneal steepening secondary to ectasia results in irregular astigmatism,
9 reduced visual acuity,
9 and increased visual distortions that can be corrected with non-surgical methods such as scleral lenses. In such cases, since the ectasia is centered or slightly inferiorly decentered, starting with a prolate scleral lens design can help achieve clearance over the central cornea and vault the ectasia.
The patient in Figure 4 presented with an advanced case of Pellucid Marginal Corneal Degeneration (PMD) significant corneal thinning inferiorly.
Figure 4
It typically presents as a bilateral, progressive condition that results in inferior peripheral corneal thinning 1-2 mm from the limbus, extending from 4-8 o’ clock.10,11 Corneal topography resembles a “butterfly” pattern with against-the-rule astigmatism.10,11 Since, the ectasia is typically peripheral, a common problem noted with corneal gas permeable lenses is the inferior decentration of the lens, in such cases using an oblate scleral lens design can help in achieving clearance over the ectasia. In advanced cases of ectasia, a large diameter scleral lens can help achieve sufficient clearance over the mid-peripheral elevations.
Salzmann’s nodular degeneration
In Figure 5, depicting Salzmann’s nodular degeneration, the image shows a patient with a Salzmann’s nodule in the mid periphery as indicated by the white arrow.
Figure 5
Salzmann’s nodular degeneration is a non-inflammatory, slowly progressive, degenerative condition that commonly occurs in those between 50-60 years of age.12,13 It presents as grayish-blue elevated nodules anterior to Bowman’s layer in the mid-periphery of the cornea that may cause steepening of the cornea.12,13 In such cases, corneal gas permeable lenses may hit the peripheral nodules, and scleral lenses, specifically an oblate design, can help achieve clearance over the peripheral elevations.
Penetrating keratoplasty (PK)
Patients with corneal transplants are excellent candidates for scleral lenses as the lens can mask irregular corneal astigmatism and enhance visual quality. However, the use of the lens is controversial for PK patients due to their unknown effects on the graft and endothelium. A healthy adult has an endothelial cell density of 2000-2500 cells/mm2, however as the endothelium decompensates and drops below 500-1000 cells/mm2, there are concerns of corneal edema, haze, and reduced vision. Lens modifications such as increasing the Dk of the lens material to maximize oxygen permeability, adding fenestrations, reducing wear time, and flattening landing zone can help with reducing complications.1,14
Neurotrophic corneas
Neurotrophic keratopathy is a condition marked by impaired corneal innervation due to damage of the trigeminal nerve. Decreased or absent corneal sensation can result in epitheliopathy. Most common causes of the condition are herpetic infections, acoustic neuromas, diabetes, and ocular toxicity from medications. Scleral lenses can provide a protective fluid reservoir that can promote corneal healing and visual rehabilitation.
1,14 Figure 6 depicts a patient with neurotrophic cornea with chronic dryness, epithelial defects, and scarring.
Figure 6
Limbal Stem Cell Deficiency (LSCD)
LSCD can be congenital or acquired later in life from inflammatory episodes of Steven-Johnson Syndrome, chemical burns, and
chronic contact lens wear. Patients with LSCD typically present with scarring, corneal neovascularization, and decreased vision. In such cases, scleral lenses can provide visual rehabilitation and protection of limbus from mechanical trauma while maintaining a moisture chamber for the ocular surface.
1,14Troubleshooting techniques for specialty contact lenses
Midday fogging
One of the common concerns noted with scleral lenses is midday fogging or air bubbles getting trapped under the lens. It can arise from a scleral lens edge lift off from the conjunctival tissue resulting in a portal of entry for tear exchange. Applying fluorescein after lens application can help assess lens edge lift off (Figure 7). If fluorescein seepage occurs in one of the meridians of the haptic after dye instillation, the lens is most likely flexing with each blink and pumping debris in the tear reservoir resulting in midday fogging. Steepening the lens edge for better scleral alignment can help reduce patient symptoms and prevent aggravation of papillary reaction.1
As seen in Figure 7, pooling of fluorescein shows the location of seepage and lens edge lift off.
Figure 7
Poor lens wettability
Figure 8 depicts fogging on the front surface of the lens (image on the left), which can result from poor wettability of lens material and ocular surface disease. Adding HydraPEG coating, treating ocular surface disease, and changing lens material can help with such concerns (image on the right).
Figure 8
One of the challenges during fitting can be poor surface wettability of the scleral lens especially in patients with ocular surface disease. It causes anterior lens surface fogging, deposits, and can reduce the quality of vision.
Wetting angle is an important property of the lens material that determines the ability of a fluid to spread across the lens surface. A low wetting angle helps with an even distribution of fluid over the lens surface. Selecting the appropriate lens material selection, lens coatings, and co-management of ocular surface disease can alleviate such concerns. It is important to select a lens material with sufficient Dk and a low wetting angle to help improve anterior surface wetting. However, in cases where high Dk material lenses (such as
Boston XO,
Boston XO2) are required for compromised cornea, adding hydrophilic coating such as hydraPEG can provide relief with fogging concerns.
15Key takeaways
With advancements in scleral lens technology and material availability, this lens option has provided great therapeutic advantages for patients with corneal irregularities and ocular surface disease. It is important to consider both lens material properties such as oxygen permeability, wetting angle, lens coatings along with parameter adjustments to obtain a healthy fit.
References:
- van der Worp, E. A Guide to Scleral Lens Fitting [monograph online]. Forest Grove, OR: Pacific University; 2010. Available from: http://commons.pacificu.edu/mono/4/.
- DeNaeyer, G. The Scleral Lens Vault: Selecting Scleral Lens Diameter. Contact Lens Spectrum. 2014 (29): 46.
- Michaud, L., Van der Worp, E., Brazeau, D., Warde, R., Glasson, C.J. Predicting estimates of oxygen transmissibility for scleral lenses. Contact Lens & Anterior Eye. 2012; 35(6): 266-271.
- Jedlicka, J., Johns, L.K., Byrnes, S.P. Scleral Contact Lens Fitting Guide. Contact Lens Spectrum. 2010 (10 ).
- Shovlin, J.P. Fighting flexure: Here’s how to manage reduced visual acuity sometimes associated with scleral lens wear. Review of Optometry, 2020 (2).
- Shovlin, J.P. Getting back in shape: Practitioners faced with lens flexure should take note of how to solve the problem. Review of Optometry, 2016 (8).
- Rabinowitz, Y.S. Keratoconus. Survey of Ophthalmology. 1998; 42 (4): 297-319.
- Romero-Jimenez, M., Santodomingo-Rubio, J., Wolffsohn, J.S. Keratoconus: a review. Contact Lens and Anterior Eye. 2010; 33 (4): 157-166.
- Lawless M, Coster DJ, Phillips AJ, et al. Keratoconus: diagnosis and management. Australian and New Zealand Journal of Ophthalmology. 1989;17:33-60.
- Krachmer, J.H. Pellucid Marginal Corneal Degeneration. Archives of Ophthalmology. 1978; 96 (7): 1217-1221.
- Jinabhai, A., Radhakrishnan, H., O’Donnell, C. Pellucid corneal marginal degeneration: A review. Contact Lens and Anterior Eye. 2011; 34 (2): 56-63.
- Das, S., Link, B., Seitz, B. Salzmann’s nodular degeneration of the cornea: A review and case series. Cornea. 2005; 24 (7): 772-777.
- Maharana, P.K., Sharma, N., Das, S., Agarwal, T., Sen, S., Prakash, G., Vajpayee, R.B. Salzmann’s nodular degeneration. Ocular Surface. 2016; 14 (1): 20-30.
- Harthan JS, Shorter E. Therapeutic uses of scleral contact lenses for ocular surface disease: patient selection and special considerations. Clinical Optometry (Auckland). 2018;10:65-74.
- Siergey, J. L. Troubleshooting Nonwetting Scleral Lenses. CollaborativeEYE. Retrieved August 5, 2021, from https://collaborativeeye.com/articles/mar-apr-18/troubleshooting-nonwetting-scleral-lenses/