Dropless cataract surgery is a safe and successful pharmacological advancement and treatment alternative to traditional cataract surgery with topical medications, where only half of patients achieve above a 50% rate of compliance administering postoperative drops.1
I have had patients express concerns about the rigorous, post-operative drop schedule for cataract surgery, especially those who may be older or may not have someone to help them with the aftercare of surgery. When speaking with these patients, I will introduce the treatment possibility of dropless cataract surgery.
I have found that many patients have not heard of this option before and sometimes the elimination of needing drops postoperatively has been the deciding factor for some of my patients whether or not to proceed with surgery. Increasing accessibility and awareness to cataract surgery treatment alternatives is important and will make a thoughtful difference in a patient’s overall cataract surgery experience.
Cataract prevalence and current treatment options
Cataracts are one of the most common, yet treatable, causes of vision loss around the world. In the United States alone, around 5 million cataract surgeries are performed each year and the amount of surgeries needed each year increases as the global population ages.2
Modern cataract surgery has developed remarkably since its initial inception, through innovative advancements in technology. These developments have improved the efficacy, accuracy, and comfort of having surgery. In today’s world, patients often have several options to choose from relating to their surgery. Pending their candidacy, there may be a selection of premium IOLs that a patient can elect to have placed in their eye. Patients may also choose to have laser-assisted surgery versus traditional surgery. Now more recently, patients may have different treatment options available to them as well.
Preventing infection and inflammation after cataract surgery is crucial to the success of an operation. While topical medication has historically been the mainstay of perioperative treatment, technological advancements have made way for injectable medication that can replace the need for topical drops.
What is dropless cataract surgery?
Dropless cataract surgery is a therapeutic advancement and treatment alternative that reduces the need for pre- and post-operative topical medication involved with having cataract surgery.
During surgery, a compounded antibiotic steroid suspension is injected intracamerally into the patient's eye after the IOL has been placed. A commonly used injectable is Trimoxi which is a preservative-free, single-use dose composed of Triamcinolone and Moxifloxacin.3 Other compounds, such as Dex-Moxi, utilize dexamethasone and may provide less cloudy vision side effects but will have a higher risk for a steroid response.4
The eye absorbs the injected medication over several weeks, working to control inflammation and prevent infection as the patient is healing. Some patients with pre-existing conditions such as diabetes and epiretinal membranes may still need to use an NSAID topically after surgery to decrease the risk of macula edema. The majority of patients however will go on to have successful visual outcomes without the worry or burden involved with traditional topical medication usage.
Hurdles of traditional cataract surgery medications
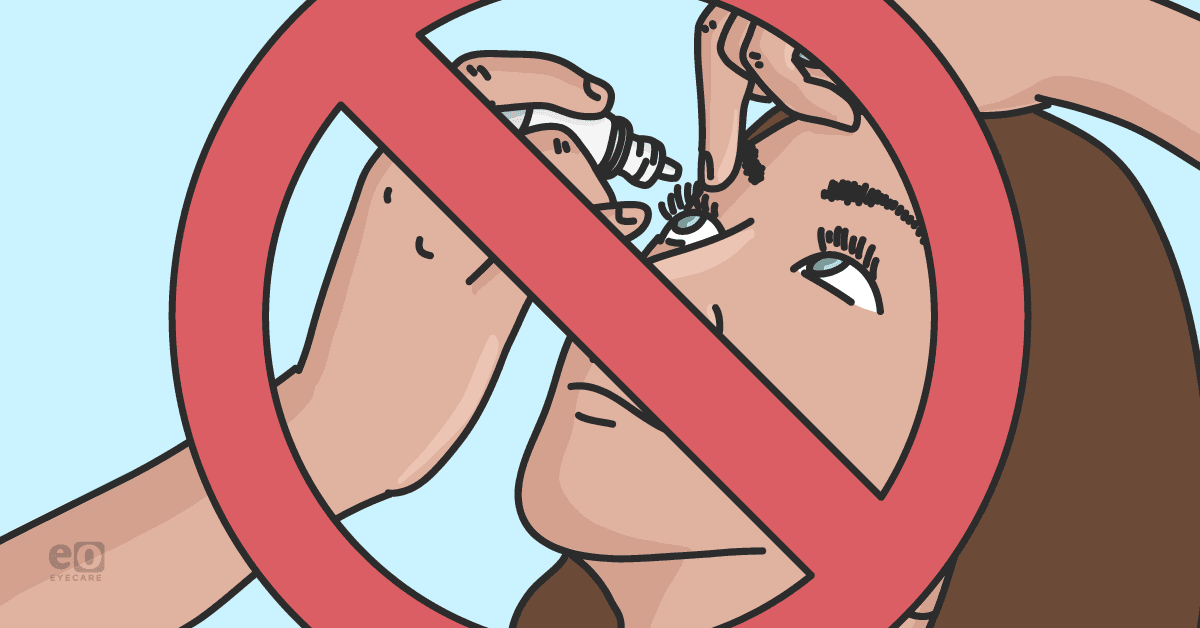
Traditionally, patients undergoing cataract surgery are required to perioperatively take an antibiotic, a steroid, and an NSAID. These medications are to be used for several weeks, all with different dosages and various tapering schedules. This can cause confusion for some patients and affect their ability to comply with the correct post operative recommendations.
Patients may not always remember to take their drops or they may have confusion on how to use them. Patients with physical limitations, such as arthritis, may have difficulty administering the drops themselves. The use of the medications is time consuming as patients are expected to wait several minutes in between each drop that they instill.
These medications can also be expensive or difficult to obtain if they are not covered by insurance, causing some patients to be out of pocket upwards of several hundreds dollars. The burden of having a direct responsibility in the success of their cataract surgery outcomes can induce anxiety in some patients.
Benefits of dropless surgery
Dropless surgery offers a simplified and easier treatment plan for patients since the need for topical drops is decreased. Patients will benefit from having less anxiety over medication burdens. Patients do not need to worry about obtaining and purchasing prescription drops and the medication that is injected is usually included in the cost of the surgery.
The risk for infections is decreased as there is less of a risk of patient non-compliance that comes from confusion or remembering to take multiple drops. Endophthalmitis occurs in up to 0.2% of all cataract surgery cases. Patients who have had an injection are five times less likely to have an occurrence than those who have undergone tradition topical medications.4 The risk of endophthalmitis is reduced when antibiotics are injected directly into the vitreous since the nutrient rich composition of the vitreous is often a habitable place for bacteria to grow.5
Additionally, patients with pre-existing corneal surface disorders such as dry eye will benefit from the decrease in ocular surface irritation that can come from preservatives in topical medications.6
Potential risks of dropless surgery
Patients should be aware that there are risks involved with having dropless cataract surgery. Although studies have shown that it is a safe procedure, the following risks can occur.
1) IOP spike
Immediately following the injection, IOP will temporarily elevate due to the increase of fluid in the eye. IOP should be carefully monitored for a steroid response throughout the post op period. Use caution in patients who are known steroid responders or who have glaucoma. The risk for a steroid response after cataract surgery in patients who have glaucoma increases by 3.72%.7
2) Hemorrhagic Occlusive Retinal Vasculitis (HORV)
Studies have shown that the incidence of HORV may possibly be associated with the use of vancomycin.8 Formulas without vancomycin can still be used to provide sufficient antibiotic coverage.
3) Breakthrough inflammation
Some patients may still experience elevated amounts of inflammation after surgery. One study showed that this occurred in 5% of patients.9
These patients will need to be placed on topical drops including an NSAID to decrease inflammation. These patients may have pain, redness, and light sensitivity. It may be advantageous to prophylactically supplement dropless surgery with a once a day NSAID drop to decrease risk of rebound iritis and cystoid macular edema for patients with known risk factors.
4) Pain
Patients may feel discomfort at the injection and surgical incision sites. Symptoms can be mitigated with the use of artificial tears or a once a day NSAID drop.
5) Retinal detachment
As with all cataract surgeries, retinal detachments are a rare but present risk occurring in up to 3.6% of all cataract surgery patients.10
Post-operative care
Patients will need to follow the standard post operative appointment schedules to be seen 1 day, 1 week and 1 month after surgery. It is necessary to educate patients prior to surgery that they may experience temporary side effects from the injection that can affect their vision.
I would reassure patients that their immediate vision following cataract surgery is not likely to be their end result vision. Patients may experience cloudy and blurry vision for several days and floaters may linger for weeks until the medication has been completely absorbed.
I would carefully review the signs and symptoms of a retinal tear or detachment with patients and discuss that if they should occur, it is necessary to rule out any retinal pathology with a dilated exam since many of the symptoms can present similarly.
Upon dilation, the injectable material will be viewable using a BIO. The suspension will appear as a whitish, cloud-like coalescence that is sitting inferiorly in the vitreous and will absorb over time. Patients should be carefully monitored for any breakthrough inflammation and I would advise them to return for an evaluation if they experience any decrease in vision, pain, redness, or light sensitivity.
Prognosis
Studies have shown that dropless cataract surgery with the use of an injection is a suitable substitute for a traditional post-operative drop schedule to decrease the risk of infection and inflammation post operatively. The procedure has a high success rate and a 2018 study8 showed that patients obtained successful visual outcomes following surgery and did not go on to need any drops post operatively to manage inflammation or infection. Patients will have improved compliance, less medication burden and an overall simplified experience.
References
- Hermann MM, Ustündag C, Diestelhorst M. “Electronic Compliance Monitoring of Topical Treatment after Ophthalmic Surgery.” International Ophthalmology. U.S. National Library of Medicine. https://pubmed.ncbi.nlm.nih.gov/20373127/.
- “Future of Cataract Surgery Seems Promising.” Healio. https://www.healio.com/news/ophthalmology/20210126/future-of-cataract-surgery-seems-promising#:~:text=At%20present%2C%20approximately%204%20million,and%20nearly%2028%20million%20worldwide.
- “Tri-Moxi+™* – 0.6ml – Single Use Vial.” ImprimisRx, 17 Mar. 2022, https://www.imprimisrx.com/formulation/tri-moxi-plus/.
- Ibach M. “Less Is More: What You Need to Know about Dropless Cataract Surgery.” Review of Optometry. 15 May 2017. https://www.reviewofoptometry.com/article/less-is-more-what-you-need-to-know-about-dropless-cataract-surgery.
- Dexter A. “The Scoop on Dropless Cataract Surgery.” The Scoop on Dropless Cataract Surgery. https://blog.optoprep.com/the-scoop-on-dropless-cataract-surgery.
- “Debating the Merits of Dropless Cataract Surgery.” Healio. https://www.healio.com/news/ophthalmology/20141223/j241_3224_02_news_print_2
- Bojikian KD, Nobrega P, Roldan A, Forrest SL, Tsukikawa M;Chen PP. “Incidence of and Risk Factors for Steroid Response after Cataract Surgery in Patients with and without Glaucoma.” Journal of Glaucoma, U.S. National Library of Medicine. https://pubmed.ncbi.nlm.nih.gov/33428351/.
- Institute, aAssil Eye. “Dropless Cataract Surgery: Modernizing Perioperative...Current Opinion in Ophthalmology.” LWW. https://journals.lww.com/co-ophthalmology/fulltext/2021/01001/dropless_cataract_surgery__modernizing.1.aspx.
- Bardoloi, Narayan, et al. “Efficacy and Safety of Dropless Cataract Surgery.” Indian Journal of Ophthalmology.Wolters Kluwer - Medknow, June 2020. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7508123/#ref18.
- Olsen, Thomas, and Peter Jeppesen. “The Incidence of Retinal Detachment after Cataract Surgery.” The Open Ophthalmology Journal, Bentham Open, 2012. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3447164/.