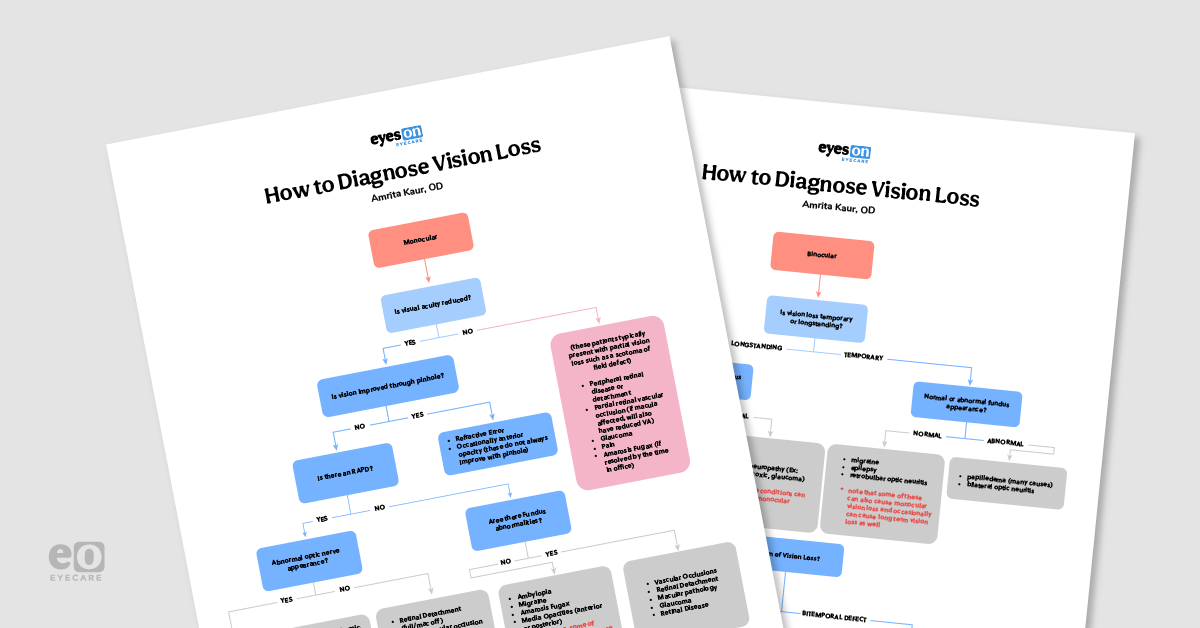
When a patient presents with vision loss it can be terrifying not only for the patient but for you as an eye care provider too! While there are seemingly innumerable causes of vision loss, simply breaking down a patient’s signs and symptoms can help the practitioner make a diagnosis. This flowchart and accompanying article serve as a guide for the practitioner regarding common causes of vision loss.
Please note: This piece discusses some of the most common causes of vision loss, but it is not a comprehensive discussion on every possibility for vision loss. As always, the practitioner should use their best clinical judgment on a case by case basis.
Monocular vs binocular vision loss
The first question to ask to hone in on a cause for the vision loss is, “Is the vision loss in one or both eyes?” If the patient reports the vision loss is binocular, we want to determine if this vision loss is/was temporary or if it is longstanding. A detailed history helps to deduce the duration of the vision loss, but sometimes we do not know yet if the presenting vision loss will be resolved with limited time and treatment or if it will be longstanding.
Note: Vision loss does not merely refer to a reduction in central visual acuity, but pertains to peripheral vision and scotoma defects as well.
📚
Download the Vision Loss Flowchart!
This colorful and comprehensive flowchart is 100% free!
Temporary vs longstanding vision loss
If the binocular vision loss was transient (lasting generally less than 24 hours), consider
complex migraine or occipital epilepsy. With these conditions, the fundus and optic nerve appearance will likely be normal.
1 These patients are typically best referred to and managed by neurology.
Retrobulbar optic neuritis is another cause of temporary vision loss that presents with normal appearing optic nerves and fundi. Optic neuritis itself indicates an inflammation of the optic nerve, and retrobulbar cases occur behind the lamina cribrosa, thus the optic discs appear normal.2 However, this vision loss is generally not fleeting, but rather seems to resolve over weeks or even months. With most cases of optic neuritis, vision reaches near normal function after 6 months, but occasionally a patient’s vision is altered for life.
While any
optic neuritis can present with bilateral vision loss, the majority of cases present as acute unilateral pain and vision loss.
2,3Although most cases of optic neuritis are retrobulbar in nature, about one third of active cases will present with visible optic disc swelling.
3,4 Optic neuritis is associated with demyelinating lesions, infections, inflammatory conditions, and autoimmune disorders.
Note: The most common cause of demyelinating optic neuritis is multiple sclerosis (MS).4
Be sure to differentiate nerves with apparent optic neuritis from those presenting with
papilledema, another cause of bilateral vision loss. Papilledema is optic disc swelling caused by high intracranial pressure (ICP). In contrast to optic neuritis, papilledema is most commonly bilateral and symmetric, and only in longstanding or severe stages affects central visual acuity.
Generally, vision loss in acute stages of papilledema presents with enlargement of blind spots. There are numerous causes of papilledema, but common causes include intracerebral masses or hemorrhages, head trauma, hypertensive crisis, idiopathic intracranial hypertension, meningitis, hydrocephalus, spinal cord lesions, and idiopathic causes.5-8
Remember that while there are many causes of disc edema, the edematous nerves are only referred to as papilledema if the cause is from ICP. Patients with ICP may also present with headaches,
diplopia, pulsatile tinnitus, or even photopsia.
5-7Treatment of any optic nerve edema or inflammation often depends on the underlying cause, but given that we may be uncertain of what this is, prompt referral to the emergency department is often warranted. Be sure to inform the ED of your findings and the patient symptoms. It may be necessary to specify that the patient needs neuro-imaging. If neuro imaging is inconclusive, ask the ED to consider lumbar puncture as well.
When binocular vision loss is longstanding or of gradual onset, we again want to observe if the fundus exam appears normal or not. If the fundus exam is normal, this is most likely some type of neurological vision impairment. Often, the vision loss will present with some type of peripheral vision defect.9,10 Therefore, we next want to assess what the pattern of vision/field loss is.
A visual field is an invaluable tool in assessing all of the aforementioned conditions but is particularly helpful in assessing binocular vision loss with normal appearing fundi.
Identifying the pattern of vision loss with a visual field
If the defect is bitemporal, consider a chiasmal lesion (often related to the pituitary gland). Note that anterior chiasmal lesions may produce a junctional scotoma (an ipsilateral central scotoma and contralateral superior temporal scotoma) or only a monocular defect.10
If the defect is a homonymous hemianopia, it is likely caused by a post-chiasmal lesion. Depending on the site of lesion, the hemianopia can vary in shape and pattern. Generally, the more posterior the lesion in the optic pathway, the more congruous the hemianopia will be. Recall that the visual defect will be the opposite side of the lesion; a right sided lesion in the occipital cortex produces a left hemianopia.9,10
Posterior circulation strokes are common culprits of these types of visual field defects, but other causes may include cardiac embolism, head trauma, epilepsy, infection, or eclampsia to name a few.9 While the vision loss from cortical blindness is often longstanding, the symptoms may be acute for the patient when they present to our office, so it is important we perform all appropriate testing and take a detailed history in forming a diagnosis.
On our end, we always want to perform visual field testing, color vision, and pupil testing at minimum.
If our testing points to a neurological defect or cortical lesion (or if inconclusive), these patients will need to be referred for neuroimaging and further evaluation, typically by neuro-ophthalmology or neurology.
Figure 2: Visual field defects
For more on visual pathway and visual field defects and access to Tyler Mathenia's full cheat sheet, click here.
When longstanding bilateral vision loss presents with obvious optic nerve abnormalities on fundus exam, there are a host of optic neuropathies to consider. While most optic neuropathies occur unilaterally, many congenital, hereditary, toxic, compressive, and nutritional deficiency related optic neuropathies occur bilaterally.
11-14 Optic nerve pallor is a hallmark of a long-standing nutritional or toxic optic neuropathy.
Bilateral optic nerve cupping can be seen in congenital, compressive, glaucomatous, and even methanol poisoning optic neuropathies, though these often also present unilaterally.11
Monocular vision loss and visual acuity
Now that we have considered some major causes of bilateral vision loss, we may begin to consider causes of monocular vision loss. After taking a thorough history, the first clinical step in narrowing down differential diagnoses in monocular vision loss is to assess if the patient’s visual acuity is reduced. If a patient notes vision loss but their central acuity is NOT reduced, we are likely dealing with a partial vision loss like a scotoma or a peripheral field defect.15
When presented with monocular peripheral vision loss, it is crucial to perform a thorough dilated exam to rule out the following pathology.
Peripheral retinal disease, breaks, or
retinal detachments are common causes of monocular peripheral vision loss, as long as the macula is not involved.
15-17 We know there are limitless ways of obtaining a retinal break/detachment, so a proper history is paramount to assess for this possibility.
The most common symptom of a retinal detachment is sudden painless loss of vision. If it affects the macula there will obviously be blurring of the central vision, but it is often the partial retinal detachments that present with field loss or shadowing in a particular area of vision.
We also want to be wary if a patient presents with symptoms described as flashes of light, new floaters, or a curtain or veil over their vision. Risk factors for retinal detachment and tears include ocular surgery, family history, myopia, lattice degeneration, trauma, and genetic connective tissue disorders to name a few.16, 17 Regardless of cause, these typically require prompt referral for treatment or prophylaxis.
There are also a myriad of retinal diseases that may cause peripheral vision loss, from hereditary or infectious to autoimmune causes.
15-18 Of note, the most common retinal dystrophy is
retinitis pigmentosa (RP), which affects about 1 in 3,000 individuals. It often begins with the notable night-blindness and progressive field loss before eventually disrupting central visual acuity.
18Glaucomatous vision loss
As mentioned above, glaucomatous damage can be a cause of bilateral peripheral vision loss, but keep in mind that it can also cause unilateral or asymmetric peripheral vision loss. We know that uncontrolled
glaucoma causes characteristic damage to the optic nerve’s ganglion cells and axons with corresponding visual field loss.
20 Often, the nasal visual fields are the first to be affected.
19,20If adequately controlled in time, most forms of glaucoma can be halted with minimal to no peripheral vision loss. However, if it progresses, patients may experience tunnel vision, decreases in color vision and contrast sensitivity, and even loss of central vision.19
Generally (not always) the culprit of glaucoma is elevated intraocular pressure, and the resulting vision loss is gradual.
19,20 One major exception to a gradual onset of glaucomatous vision loss is acute angle closure that presents with sudden onset blurry vision (generally unilateral), with accompanying pain, photophobia, nausea, headache, and corneal edema.
20 Treatment of all types of glaucoma varies by the type and severity.
19,20Partial retinal vision loss: BRVO, BRAO, CRAO
Partial monocular visual loss may also result from vascular issues, namely branch
retinal vessel occlusions. A branch retinal vein occlusion (BRVO) results from blockage of a retinal vein (other than the central retinal vein) at an arteriovenous crossing. If the macula is not involved, patients may present with only a scotoma or mild field defect in the corresponding area, or may not even note any significant vision loss.
15,21A BRVO involving the macula, however, will cause obvious central vision loss due to resulting macular edema. Note that vein occlusions must be discerned from other retinal vascular issues such as
diabetic retinopathy, which can also cause both peripheral and central vision loss. Most BRVO’s occur in the superotemporal retina. While most BRVO’s tend to have a good visual prognosis over time, they need to be monitored closely for neovascular complications such as glaucoma.
15, 21A retinal artery occlusion occurs when a retinal artery is occluded from an embolus, vasculitis, inflammation, or coagulpathies.22 This results in infarction of the retina, and therefore acute vision loss to the area of the artery’s distribution. A branch retinal artery occlusion (BRAO) often presents with altitudinal or sectoral defects, but may present with a central scotoma if the macula is involved.
The majority of BRAO’s present with visual acuity of 20/40 or better.23 A central retinal artery occlusion (CRAO) on the other hand, commonly has a final visual acuity of 20/400 or worse. A CRAO that presents in an eye with a cilioretinal artery, however, tends to have improved visual outcome as the macula is spared from infarction.22,24
Always remember that giant cell arteritis is a potential cause of any retinal artery occlusion, and must promptly be ruled out.22-25
On occasion, a patient may have an episode of amaurosis fugax, which may also cause a monocular, transient loss of the full or partial visual field. Vision may be near normal by the time the patient presents to the office.29 We will go into detail about this condition below.
What happens when a patient’s visual acuity is reduced?
Now we may begin to consider differentials in monocular vision loss when a patient’s visual acuity is reduced. When central acuity is reduced, we always want to determine if the visual acuity can be improved with pinhole before proceeding. If vision can in fact be improved with pinhole, first consider refractive error.15 Often patients mistakenly report a loss of vision, when it is in fact blurry vision. If this change in refractive error has occurred suddenly, we need to rule out systemic causes such as diabetes.26
Additional causes of monocular blur or loss of vision that can be corrected with pinhole acuity are media opacities such as lens, corneal, or even vitreal abnormalities. Note however, that if severe, these conditions do not always correct to improved VA with pinhole acuity.15
If monocular vision loss acuity cannot be corrected with pinhole, next determine if an RAPD is present in that eye. If there is no RAPD, closely examine the fundus and its structures for any abnormalities. If the fundus appears normal, consider
amblyopia. Adult patients will likely not present on an emergent basis with this, as they will realize it is longstanding, but it is an important differential to remember, particularly with children. Recall that amblyopia may result from refractive, deprivation, and strabismic causes.
27Realize that monocular blurry vision with a normal fundus may be transient, and the patient’s symptoms may have resolved by the time they present to the office. We still want to rule out more serious ocular pathology, but be sure to consider migraine in these cases, as mentioned previously. Vision loss secondary to migraine auras may occur in one or both eyes.1
As noted above, another cause of transient monocular vision loss that may not present with any fundus abnormalities is amaurosis fugax.29 Amaurosis fugax is generally a monocular, transient, and painless loss of vision resulting from an occlusion (often an embolus) of the internal carotid artery (ICA) circulation. The vision loss may last up to 30 minutes, but in most cases it lasts a few seconds to a few minutes. Multiple episodes may occur, in which case giant cell arteritis must be ruled out (discussed more below).
If an intraretinal Hollenhorst plaque is noted, be wary that a retinal artery occlusion has the potential to develop.
In rare occasions, ocular ischemic syndrome may also develop from the causative carotid artery occlusion. These patients often possess predisposing vascular risk factors, and are at an increased risk of stroke. Treatment should be centered around controlling such risk factors and warrant co management with cardiology, neurology, and a primary care provider.29
When there is no RAPD in monocular vision loss, but there are fundus abnormalities, a different set of differentials needs to be reviewed. We previously discussed vascular occlusions as a cause of partial/peripheral vision loss, but they can be a culprit of central or full field vision loss as well. While branch vein and artery occlusions generally only impact central vision if the macula is involved, central retinal vein and artery occlusions have a high likelihood of affecting the macula which results in poor visual prognosis. As mentioned above, a CRAO often has a VA worse than 20/400, unless there is macular sparing from a cilioretinal artery.22
If a CRVO is ischemic, most patients will present with a BCVA of worse than 20/200. If non-ischemic, however, there is a better chance of BCVA reaching better than 20/200 in most patients.15, 29
Retinal detachments and limitless retinal diseases may also contribute to a loss of central vision. We know from a previous section that retinal detachments involving the macula do disrupt central vision—and if they have not yet impacted the macula they need emergency prophylactic treatment.15-17 Describing all the types of retinal damage or diseases that cause a loss of monocular VA would be several articles in itself, but realize the causes can include congenital, hereditary, vascular, traumatic, inflammatory, and neoplastic sources.15, 30
In the same light, note that there are an innumerable variety of macular diseases that may cause monocular vision loss as well; this includes anything from diabetic macular edema or central serous retinopathy, to all forms of
macular degeneration.
15 Additionally, do not forget severe unilateral or asymmetric glaucoma as a thief of central vision, as we detailed previously.
19,20 Be mindful that while these monocular conditions do not generally present with an RAPD, there are always exceptions in severe cases.
15If there is an RAPD, we want to closely assess the appearance of the optic nerve. If there are no obvious optic nerve abnormalities, we do want to consider severe or unusual cases of some of the pathology we have already discussed. Conditions to consider include a full retinal detachment, advanced macular degeneration, retinal vascular occlusions, retrobulbar optic neuritis, posterior optic neuropathies, and post surgical optic nerve damage.1-6, 11-17, 21-25
Finally, we may consider visible optic nerve abnormalities in the cases of monocular vision loss with the presence of an RAPD. These cases primarily entail unilateral optic neuropathies and optic neuritis.
Optic neuropathies
Previously we discussed the possibility of optic neuritis occurring bilaterally, but the majority of causes occur as acute, unilateral, and often painful vision loss.2,3 Recall that optic neuritis is associated with demyelinating lesions (namely MS), infections, inflammatory conditions, and autoimmune disorders.2-4
Optic neuropathies stem from a variety of conditions. In addition to optic neuritis, quick-onset optic neuropathies often arise from ischemic, traumatic, and inflammatory causes. Compressive/neoplastic, toxic, and nutritional optic neuropathies, on the other hand, often progress over months. Compressive optic neuropathies may also take place over years before an obvious manifestation, as can hereditary optic neuropathies.11-14
Though we cannot go into detail about all of the particular optic neuropathies in this space, it is important to remember a few key conditions. If a patient age 50 years or older presents with sudden vision loss, we always want to rule out an arteritic anterior ischemic optic neuropathy (AAION) associated with giant cell arteritis (GCA). This is an ocular emergency and requires prompt workup and treatment, especially because it can progress to vision loss in the fellow eye if not addressed in time.
ESR and CRP need to be ordered in a timely manner; if these tests are negative, a temporal artery biopsy may be performed if GCA is still highly suspected. Often, anti-inflammatory treatment is initiated before test results are received due to the high risk of fellow eye involvement.36
Fundus exam will reveal diffuse optic nerve pallor and swelling, often with cotton wool spots (see Figure 4). Patients with AAION often also experience temporal or jaw pain, fatigue, weight loss, and diplopia.11,31,36
Hopefully this guide improves your confidence in managing cases of both bilateral and monocular vision loss—although we hope you do not need it often!