Steroids are a commonly prescribed drug for the treatment of several autoimmune and inflammatory conditions. Though steroid usage has many benefits, it can induce ocular hypertension with topical, periocular, intraocular administration, intranasal, inhalational, systemic use, and dermatological applications. If intervened at the right time, the ocular hypertensive response is usually reversible and can prevent a vision-threatening complication, like steroid-induced glaucoma.
Who is at risk for steroid-induced glaucoma?
- Patients with primary open angle glaucoma (POAG). Approximately 90% of POAG patients and 30% of glaucoma suspects might have an ocular hypertensive response to only a four-week course of topical dexamethasone 0.1%.1
- Patients with pigment dispersion syndrome or traumatic angle recession.2,3
- Patients under 10 years of age and older adults. Studies describing steroid-induced glaucoma have mainly focused on adults. However, children are known to have severe ocular hypertensive responses to topical steroids when compared to adults, and significant intraocular pressure (IOP) elevation has also been reported in infants treated with nasal and inhalational steroids.4
- Patients with a history of corneal surgeries, such as penetrating keratoplasty, Descemet’s stripping endothelial keratoplasty (DSEK), or refractive surgeries. Diagnosing steroid-induced glaucoma can be difficult in patients who have had corneal surgeries because of the falsely low IOP measurements from the thin central corneal thickness, corneal edema, and ocular rigidity changes.5,6
- Patients who have high myopia, diabetes mellitus, and connective tissue disease, especially rheumatoid arthritis.7,8,9
- Patients with endogenous glucocorticoid overproduction.10
How do these patients present upon examination?
Steroid-induced glaucoma is often asymptomatic. On examination, the eye is usually unremarkable. Upon discovering a patient has an elevated IOP of 10mm to 22mm beyond the normal range along with a medical history of steroid use, they are reported to have steroid-induced ocular hypertension.
Individuals who develop an increase in IOP following steroid use are referred to as "steroid responders." In severe cases, patients may complain of blurred vision from corneal edema or a steroid-induced posterior subcapsular cataract.11 Patients may also notice a visual field defect.11 A sudden spike in IOP may even cause a brow or eye ache.11
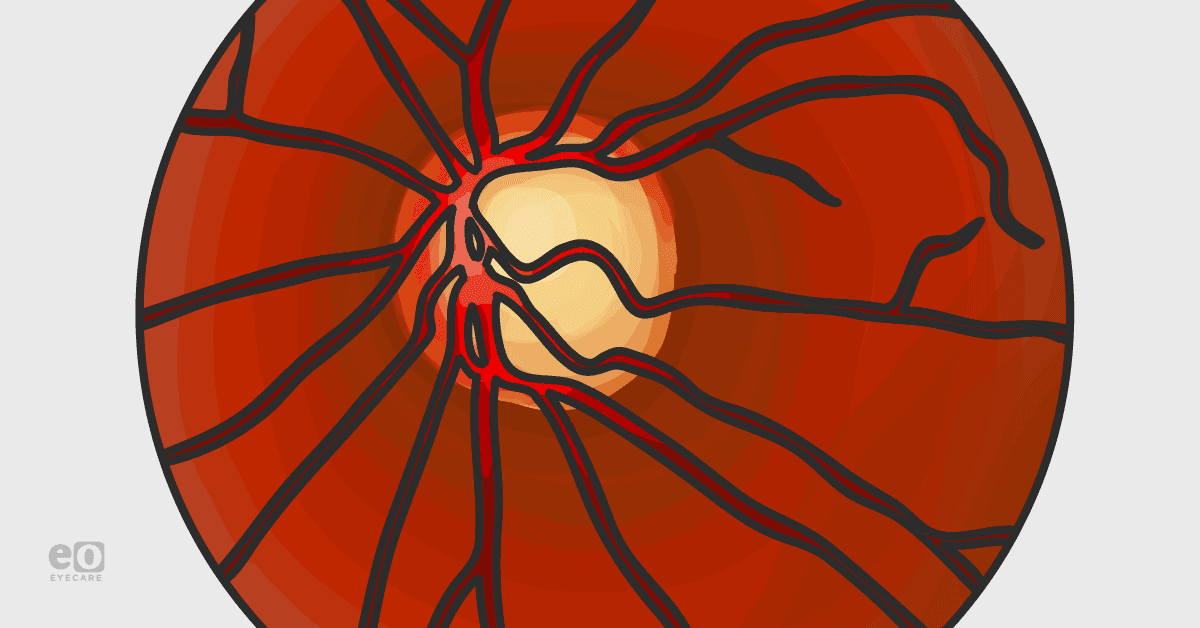
IOP elevation normally occurs three to six weeks following topical steroid use, but can occur earlier. Corticosteroid injections may cause IOP elevation after several months.11 IOP elevation of sufficient magnitude and duration can progress to steroid-induced glaucoma, leading to progressive damage to the optic nerve and visual field.
Steroid-induced glaucoma can present clinically different, depending on the patient’s age.12 Children may initially present with watering, blepharospasm, and photophobia. In more severe cases, an enlarged corneal diameter and buphthalmos may be present as observed in congenital glaucoma.12 Elderly patients who have received steroid treatment and then discontinue it may present as having normal-tension glaucoma.12
Studies by Armaly and Becker developed three categories of steroid responders based on the IOP response to topical betamethasone and dexamethasone.13
- High responders developed an IOP greater than 31 mm Hg or a rise of more than 15 mm Hg from baseline.
- Intermediate responders developed an IOP between 25-31 mm Hg or a rise of 6-15 mm Hg from baseline.
- Non-responders or low-responders were found to have an IOP less than 20 mm Hg or a rise of less than 6 mm Hg from baseline.
What are the treatment options for steroid-induced glaucoma?
Discontinuation of the steroid is the first line of management. Steroid-induced hypertension typically normalizes within days of stopping the steroid, and more long-lasting forms can take between one to four weeks.14 If it is difficult to discontinue the steroid completely, consider reducing the dose or prescribing a weaker steroid as an alternative.14
More long-term management options include typical treatments similar to that of POAG:
- Antiglaucoma agents may be used. This includes prostaglandins, beta-blockers, alpha-2 agonists, and carbonic anhydrase inhibitors.
- Laser trabeculoplasty may be considered, especially if patients are experiencing undesirable side effects with the antiglaucoma drugs.15
- Surgical management is indicated in those patients who fail to respond to medical and laser therapies. The most common surgical procedure is trabeculectomy, tube shunt surgeries, or cyclodestructive procedures.15
Steroids are widely prescribed by healthcare workers, and it is essential for the patient’s healthcare team to refer to an eyecare professional who is able to properly monitor for the signs and symptoms of steroid-induced glaucoma. It is also essential to educate patients that are taking steroid medications the importance of following up with their eye care professionals so that the proper identification of risk factors and regular monitoring for ocular hypertension can occur in order to prevent or detect this condition at an early stage.
References:
- Armaly M F. Effect of corticosteroids on intraocular pressure and fluid dynamics. II. The effect of dexamethasone in the glaucomatous eye. Arch Ophthalmol. 1963 Oct; 70:492–499.
- Becker B, Podos SM. Krukenberg’s spindles and primary open angle glaucoma. Arch Ophthalmol. 1966 Nov;76(5):635–639.
- Spaeth GL. Traumatic hyphema, angle recession, dexamethasone hypertension and glaucoma. Arch Ophthalmol. 1967 Dec;78(6):714–721.
- Ohji M, Kinoshita S, Ohmi E, Kuwayama Y. Marked intraocular pressure response to instillation of corticosteroids in children. Am J Ophthalmol. 1991 Oct 15;112(4):450–454.
- Hamilton DR, Manche EE, Rich LF, Maloney RK. Steroid- induced glaucoma after laser in situ keratomileusis associated with interface fluid. Ophthalmology. 2002 Apr;109(4):659–665.
- Lee WB, Jacobs DS, Musch DC, Kaufman SC, Reinhart WJ, Shtein RM. Descemet’s stripping endothelial keratoplasty: safety and outcomes: a report by the American Academy of Ophthalmology. Ophthalmology. 2009 Sep;116(9):1818–1830.
- Podos SM, Becker B, Morton WR. High myopia and primary open-angle glaucoma. Am J Ophthalmol. 1966 Dec;62(6):1038–1043.
- Becker B. Diabetes mellitus and primary open-angle glaucoma. Am J Ophthalmol. 1971; 1–16.
- Gaston H, Absolon MJ, Thurtle OA, Sattar MA. Steroid responsiveness in connective tissue diseases. Br J Ophthalmol. 1983 Jul;67(7):487–490.
- Haas JS, Nootens RH. Glaucoma secondary to benign adrenal adenoma. Am J Ophthalmol. 1974 Sep;78(3):497–500.
- Razeghinejad MR, Katz LJ. Steroid-induced iatrogenic glaucoma. Ophthalmic Res. 2012;47(2):66-80.
- Sihota R, Konkal VL, Dada T, Agarwal HC, Singh R. Prospective, long-term evaluation of steroid-induced glaucoma. Eye (Lond). 2008 Jan;22(1):26-30.
- Armaly MF, Becker B. Intraocular pressure response to topical corticosteroids. Federation proceedings.1965;24:1274–1278.
- Espildora J, Vicuna P, Diaz E. Cortisone-induced glaucoma: a report on 44 affected eyes. J Fr Ophthalmol. 1981;4(6-7):503–508.
- Sihota R, Konkal VL, Dada T, Agarwal HC, Singh R. Prospective, long-term evaluation of steroid-induced glaucoma. Eye (Lond). 2008 Jan;22(1):26-30.