Dry eye disease (DED) is a prevalent ocular condition as well as a common reason for visits to eyecare providers. Currently, more than 16 million American adults have dry eye and many more are thought to have undiagnosed DED.1 The prevalence of dry eye disease varies from 7.4% to 33.7% among studies based on how the investigators define the disease.2
While the definition of dry eye is evolving, the most widely accepted definition is that of Dry Eye Workshop (DEWS) II, which defines dry eye as “a multifactorial disease of the ocular surface characterized by a loss of homeostasis of the tear film, and accompanied by ocular symptoms, in which tear film instability and hyperosmolarity, ocular surface inflammation and damage, and neurosensory abnormalities play etiological roles.”3
DED develops when there is a disruption of tear film homeostasis. In DED, the tear film becomes unstable and the corneal epithelium thins, which leads to inflammation and immune dysregulation of the corneal surface.4
Changes in corneal epithelium, corneal nerves, corneal stroma, and corneal endothelium have all been observed in DED.4 Furthermore, inflammation, one of the main causes of DED, can lead to stromal change and weakening of the corneal tissue.4
The role of ocular surface imaging in DED detection
Ocular surface imaging is used to evaluate the effects of dry eye disease on the cornea and other structures of the ocular surface as well as study the shape and curvature of the cornea. Imaging technologies are critical in diagnosing DED and identifying the exacerbating factors, helping differentiate DED from other ocular surface diseases, and screening for DED in patients.5
Figure 1: Slit lamp image of corneal staining in a 60-year-old patient.
Figure 1: Courtesy of Dev Dhooper.
Using ocular surface imaging to identify DED
Ocular surface imaging that can be used to detect and monitor DED includes:
- Slit lamp photography
- Optical coherence tomography (OCT)
- In vivo confocal laser scanning microscopy
- Infrared meibography
- Noninvasive tear breakup time
- Corneal topography
- Fluorophotometry
Slit lamp photography
Slit lamp photography aids in the evaluation and photo-documentation of the ocular surface for patient education as well as for future comparison. The slit lamp exam should be carried out systematically to ensure a complete and efficient examination.
The patient’s history can help guide a more focused approach, but we must examine all the subtle details of a patient’s ocular surface. Evaluation of tear meniscus height is a diagnostic aspect of aqueous-deficient DED and mixed etiology DED,5 which can also be performed at the slit lamp.
Anterior segment OCT
Anterior segment OCT (AS-OCT) uses interferometry to produce cross-sectional images of the anterior segment.6 By adding an extension lens, it can be used to get detailed images of the cornea and tear film.
In vivo confocal laser scanning microscopy
In vivo confocal laser scanning microscopy can be used to assess the integrity and morphology of the corneal epithelium, nerves, stroma, and endothelium. It can also assess nerve fiber density, nerve reflectivity, and tortuosity, as well as inflammatory cell, goblet cell, stromal keratocyte, and endothelial cell density and morphology.5
Corneal pachymetry
Although corneal pachymetry and epithelial thickness maps are not diagnostic criteria for dry eye disease, studies have shown marked differences in patients with DED as compared to healthy eyes.5
Infrared meibography
Meibography is a diagnostic tool for meibomian gland dysfunction (MGD), which is a root cause of evaporative dry eye disease.5 Infrared meibography uses infrared light to visualize meibomian glands in vivo.7
Meibography helps in identifying gland atrophy, segmentation, and tortuosity as well as aids in documenting gland structure and monitoring for change over time.8 Atrophy is a partial loss of meibomian glands, while dropout is a complete loss from orifice to fornix.8 Gland segmentation is seen as a black line splitting the gland causing a disjointed appearance.8
It is also very helpful in educating the patient about the root cause of dry eye disease. Showing the changes in meibography over time helps the patient understand the progressive nature of the disease and the consequent symptoms.
Figure 2: A 63-year-old male patient with meibomian gland tortuosity and dropout.
Figure 2: Courtesy of Dev Dhooper.
Figure 3: A 33-year-old patient with severe meibomian gland loss.
Figure 3: Courtesy of Dev Dhooper.
Tear breakup time
Traditional and noninvasive tear breakup time (TBUT) are indicators of tear film stability. TBUT is performed by having a patient stare straight ahead without blinking. The TBUT is then determined by noting the time at which the first dry spot or “hole” develops in the tear film.
TBUT has been shown to be decreased in keratoconjunctivitis sicca, mucin deficiency, and meibomian gland disease.5 The typical cutoff for a normal TBUT value is 10 seconds, with anything below that being considered abnormal.5
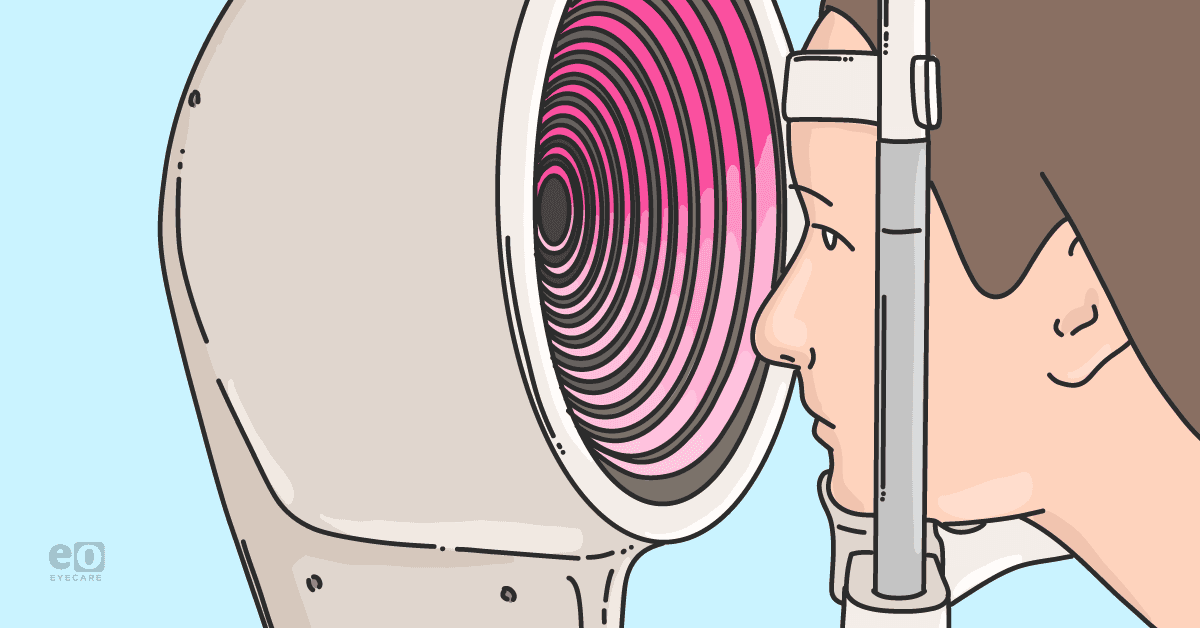
Corneal topography
Corneal topography (demonstrated in Figure 4) is very useful for examining characteristics of the cornea, such as shape, curvature, power, and thickness. It is also helpful in identifying ocular surface disease and its impact on the patient’s vision.
Corneal topography is useful for refractive surgery evaluation, keratoconus diagnosis and management, and assessment of the ocular surface. Furthermore, corneal topography helps in the diagnosis of pterygium, Salzmann nodules, and corneal scarring.
Figure 4: Image of corneal topography with the Keratograph 5M (Oculus).
Figure 4: Courtesy of Dev Dhooper.
Fluorophotometry
Fluorophotometry (as seen in Figure 5) is a noninvasive technique that objectively detects clinical and subclinical changes in corneal epithelium by quantitatively measuring the barrier function or permeability of the cornea.9 Fluorophotometry devices record the concentration of fluorescein in different parts of the eye, such as the cornea and vitreous.9
A drop of fluorescein is applied to the eye’s surface and the fluorophotometer measures how quickly it penetrates the cornea. The amount of fluorescein that collects in the cornea stroma and clears from tears can indicate damage to the epithelium or increased corneal permeability.9
Increased corneal uptake of fluorescein indicates damage to the corneal epithelial cells, which could help diagnose and monitor dry eye disease. Patients with dry eye disease have demonstrated increased corneal permeability. Currently, fluorophotometry is used as an end-point analysis in various clinical trials.9
Figure 5: Image of fluorophotometry with the Keratograph 5M.
Figure 5: Courtesy of Dev Dhooper.
Fluorescein corneography
Fluorescein corneography (FCG) is repurposed OCT-FA (OCT fluorescein angiography) to evaluate corneal staining. It offers high-contrast visualization and higher sensitivity than slit lamp images. Further, FCG was found to be effective at detecting corneal erosions and punctate epithelial erosions and repeatable at different centers.10
Fluorescein staining of the cornea is a mainstay for assessment of the health of the epithelium. Currently, there is a lack of agreement for extracting, grading, and quantifying this biomarker.10
A concise overview of ocular surface imaging modalities
Table 1 lists the indications, advantages, and limitations of different ocular surface imaging modalities.8,9,11-17
| Name of Modality | Indicators/Use | Advantages | Limitations |
|---|---|---|---|
| Slit lamp biomicroscopy | Three-dimensional examination of the anterior segment of the eye and adnexa. | Standard piece of equipment in most clinics. Helps examine the ocular surface. | Constant sanitation after use and close proximity between provider and patient can expose parties to spread of viruses or diseases. |
| OCT | Used for cross-sectional images of the anterior segment, including the cornea and tear film. | Scan speed (around 6 seconds for each volumetric scan). Is a noninvasive technology that provides three-dimensional visualizations based on scans. | High acquisition costs. SD-OCT requires an extension lens for imaging cornea and tear film. |
| In-vivo confocal laser scanning microscopy | Helps identify ocular surface diseases, including dry eye disease, keratitis, corneal ectatic disorders, dystrophies, degenerations, and iridocorneal endothelial syndrome (ICE) syndromes. | Can image through moderately-opaque tissues, such as scarring and edema of the cornea. Helps observe dynamic processes of the cornea (inflammatory reactions or infectious keratitis). Enables study of epithelial cells, keratocytes, endothelial cells, nerves, and immune cells. | Availability typically limited to research institutions. |
| Infrared meibography | Noninvasive form of meibography using infrared filters to capture images of the meibomian glands. | Provides improved image quality. Helpful for patient education. Becoming more affordable for clinicians. | Still relatively expensive. Relatively low resolution. Most systems provide a two-dimensional image, making it hard to judge depth, although some three-dimensional imaging systems are available. |
| Noninvasive tear breakup time | Noninvasive way to measure TBUT. Can be a marker of homeostasis of the tear film. | Simple, practical, and noninvasive method that has better diagnostic performance compared to standard tear breakup time for detecting dry eye disease. | Instruments may not be readily available to all clinicians. |
| Corneal topography | Defines shape, curvature, power, and thickness of the cornea. Helps identify scarring, growths (pterygium), astigmatism, and keratoconus. Also helps with surgical planning and contact lens fitting. | Noninvasive and painless. | Topography maps can be altered by tear film abnormalities and contact lens wear. Proper patient placement is needed for accurate results. Comparisons cannot be made between different devices. |
| Fluorophotometry | A drop of fluorescein is applied to the eye’s surface and the fluorophotometer measures how quickly it penetrates the cornea. The amount of fluorescein that collects in the cornea stroma and clears from tears can indicate damage to the epithelium or increased corneal permeability. | Noninvasive and objectively measures the permeability of corneal epithelial cells. | Limited availability to clinicians. |
Table 1: Compiled by Dev Dhooper.
Patient education through ocular surface imaging
Ocular surface imaging aids with photo-documentation, diagnosis of DED, and can guide treatment. Most importantly, imaging helps the patient understand their problem and buy into their treatments. Dry eye disease is complex and difficult for patients to understand and imaging helps doctors better educate their patients.
Since DED is multifactorial, showing the patient images of their eyelids, meibomian glands, and corneal staining can help the doctor explain the problem to patients. Patients typically accept images, videos, and scans more readily than verbal explanations alone.
Images and videos help make the problem real to the patients. Showing a patient a video demonstrating their blinking patterns and tendency toward partial blinking can prove a very powerful tool to motivate them to change their visual habits. Most dry eye patients need interventions in two or more areas, including inflammation, bacterial overgrowth, lid function issues, and/or abnormal blinking patterns.
Consequently, without the patient understanding the reasoning behind at-home or in-office therapy, the treatment plan, which can sometimes be relatively time-consuming, is very unlikely to be successful. However, once the patient understands the problem, they are more likely to comply with their treatment.
There is increasing evidence that MGD is common in the pediatric population as well, and gland atrophy has been linked to 2 hours daily of screen time.8 In our increasingly digital world, we owe it to our patients to take a proactive approach in assessing meibomian gland health during every eye exam. Fortunately, imaging such as meibography is becoming more affordable as well as easy to implement in routine eye exams.
Conclusion
With different imaging techniques, we can show patients images, videos, and scans to establish a baseline and show progression to the patient.
In my experience, showing images solidifies the issue in the patient’s mind and they tend to comply better with treatments. Patients also understand that they need to change their visual behaviors with blinking exercises and breaks and maintain their eye health with home therapy.