As technicians, we wear many hats around the office, and our many roles put us in a position to make a significant impact on the care our patients are receiving.
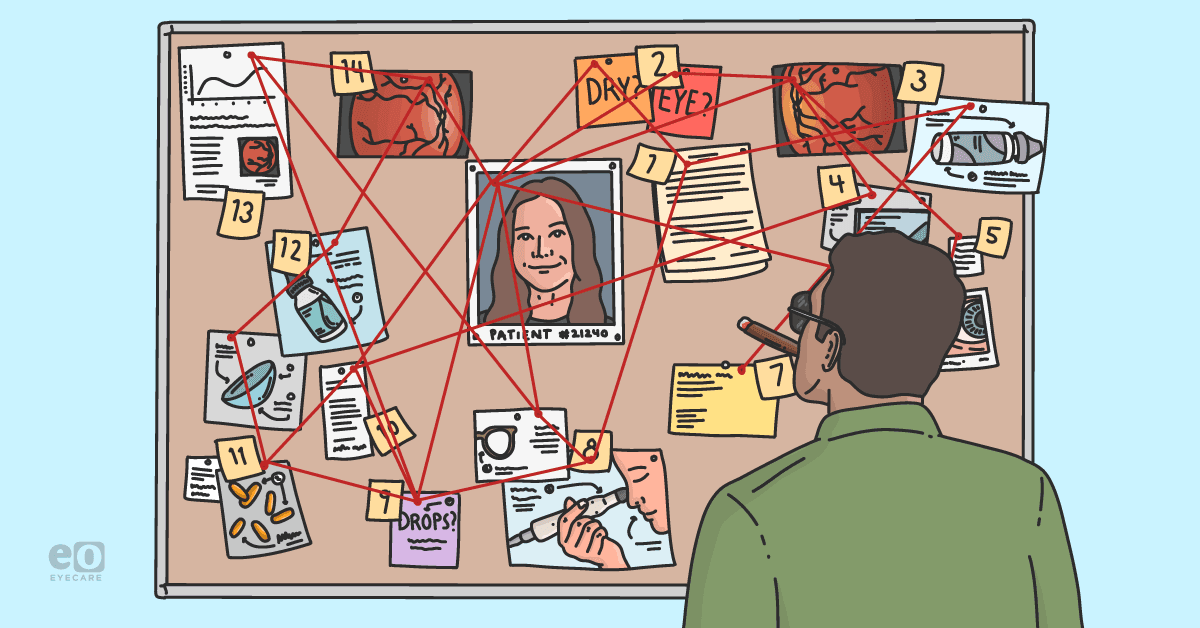
When it comes to dry eye patients, it may feel like we have a mystery on our hands. In some cases, due to low awareness and the variety of signs and symptoms associated with dry eye syndrome, patients may not even know they have it.
In my experience, it’s unfortunately common for dry eye disease (DED) and its symptoms to be overlooked or not even discussed during routine eye exams.
Consequently, as technicians, we can help identify these patients by collecting and piecing together all the information our patients provide during the intake process.
Patients may have limited awareness of DED
A 2016 survey concluded that most adults are not familiar with dry eye symptoms. Of note, 45% of responders didn’t feel DED symptoms were worth bringing up, and 1 in 3 didn’t know DED could cause long-term damage to their eyes.1
DED is a multifactorial condition with a variety of etiologies.2 While an estimated 30 million American adults report symptoms of dry eye, only 16 million have been properly diagnosed, and only 1.5 million have been treated with a prescription.3-6
Although it’s increasingly prevalent, DED can be tricky to catch in the clinic because the signs and symptoms often do not correlate. Dry eye disease affects all patients differently; some patients with severe signs of DED may report mild to moderate symptoms, while some patients with little to no signs may report acute symptoms that severely impact their quality of life and activities of daily living.
Solving the case starts by asking the right questions
Patient intake can be a challenging undertaking. Patients can suffer from “exam chair amnesia” and forget their medical history, neglect to provide pertinent information, or forget to provide the long list of medications they are currently taking.
Not to mention those times when we may run into the occasional patient who seemingly has no complaints and even forgets what brought them in for today’s visit. Building a robust patient history is crucial for accurate and timely diagnosis and treatment of dry eye syndrome and, in some cases, may help determine insurance coverage of some topical treatment options.
In addition to the standard History of Present Illness (HPI) questions, such as onset, location, duration, frequency, associated factors, relief, timing, severity, etc., history-taking can also be an opportunity to ask questions relating to each patient’s quality of life, environment, and self-medication.
Crucially, symptoms associated with activities of daily living and the use of artificial tears and other over-the-counter (OTC) treatments may uncover some DED “red flags.”
Other potential DED red flags include:
- A history of ophthalmic surgery
- Prescriptions for ophthalmic medications, particularly for chronic illnesses such as glaucoma
Exhibit A: Patient questionnaires
Patient questionnaires may reveal hidden clues and help start the dry eye disease conversation. These can be integrated into our existing electronic medical records (EMRs), patient intake forms, or provided to patients we suspect may be dry eye sufferers. These questionnaires can also be sent to patients prior to examinations, helping to facilitate the examination and save chair time.
In addition to helping us identify patients who may be suffering from dry eye symptoms, they can help us quantify a patient’s subjective level of discomfort. This can help us better relate to what our patients are experiencing and can also aid in tracking the improvement of symptoms over time after therapies or treatments have been initiated.
Two common dry eye disease questionnaires used in practice today are the SPEED, or Standard Patient Evaluation of Eye Dryness, and the OSDI, or Ocular Surface Disease Index. These questionnaires can provide us with a quantifiable score that can put a number on the patient’s level of complaint and can be tracked over time.
Follow the trail: Lifestyle and environment
A quick overview of a patient's lifestyle can reveal important dry eye syndrome clues and risk factors:
- Overuse of OTC artificial tears
- Topical ophthalmic medications such as:
- Medications for glaucoma linked with DED
- Medications such as Restasis that would indicate a DED diagnosis even if the patient does not remember why they have it
- History of ophthalmic surgery
- Environmental factors
- Occupation and workplace
- Digital device use
- Contact lens habits
- Fluctuating vision
- Dig into this one—is it fluctuating vision for seconds or minutes? Does their vision fluctuate from morning to afternoon or evening? These are important clues!
For a dry eye detective, it wouldn't take much to identify some of these behaviors or symptoms as red flags or risk factors for dry eye disease. Connecting the dots can lead to more pertinent questions that can help us paint a full picture and build a robust patient history for the doctor during the exam.
A patient who relies on OTC artificial tears and uses them multiple times daily or has been using them for several months or even years may be self-medicating to ease the symptoms of dry eye.
At the same time, a patient who notices fluctuating vision throughout the day or while performing visually tasking activities, such as driving, working on the computer, or binging the latest true crime documentary, may also be suffering from undiagnosed dry eye disease or another ocular condition.
Identifying the dry eye suspect:
- Reason for Visit: Intraocular pressure (IOP) check
- Demographics: 39 years old, male
- Occupation: IT worker (8+ hours of computer work, air-conditioned office)
- Current Ophthalmic Medications: Latanoprost nightly, OTC tears 4 times daily
- Contact Lenses: Wears daily disposable contact lenses
- Complaints: Fluctuating, blurry vision, grittiness upon waking, and watery eyes
Dry eye disease symptoms can have a significant impact on patients’ lives, including causing difficulties with everyday activities such as driving, reading, work-related tasks, and time spent on digital devices.7
Understanding the burden of dry eye on patients
The impact of dry eye can also be psychological. Specifically, depression or depressive symptoms have been associated with dry eye disease.8 In a survey of over 500 office workers, approximately 7 out of 10 reported some inhibition of daily activities due to dry eye symptoms.9 Only 30% of responders had been diagnosed with dry eye disease.
This study also found that a majority of symptomatic workers were not being treated by an eye care provider for their dry eye symptoms, instead choosing to self-medicate with artificial tears and other OTC therapies.9
With the prevalence of dry eye disease increasing daily, our constant dependence on digital devices, and the variety of factors that may contribute to dry eye disease, there is a possibility these patients are already in our practices for routine exams, contact lens fittings, ocular surgery, or management of other, more significant ophthalmic conditions (e.g., glaucoma, macular degeneration, diabetic retinopathy).
Asking the questions, collecting the evidence, and documenting and reporting the information to our doctors can help them piece together the puzzle, solve the case, and identify patients who may be suffering from dry eye disease, getting them one step closer to the appropriate diagnosis and treatment.
Conclusion
Dry eye disease doesn’t have to be a mystery that goes unsolved. Break out your best detecting skills and assume every patient holds a key piece of information that can make or break our case!