Corneal foreign body removal1
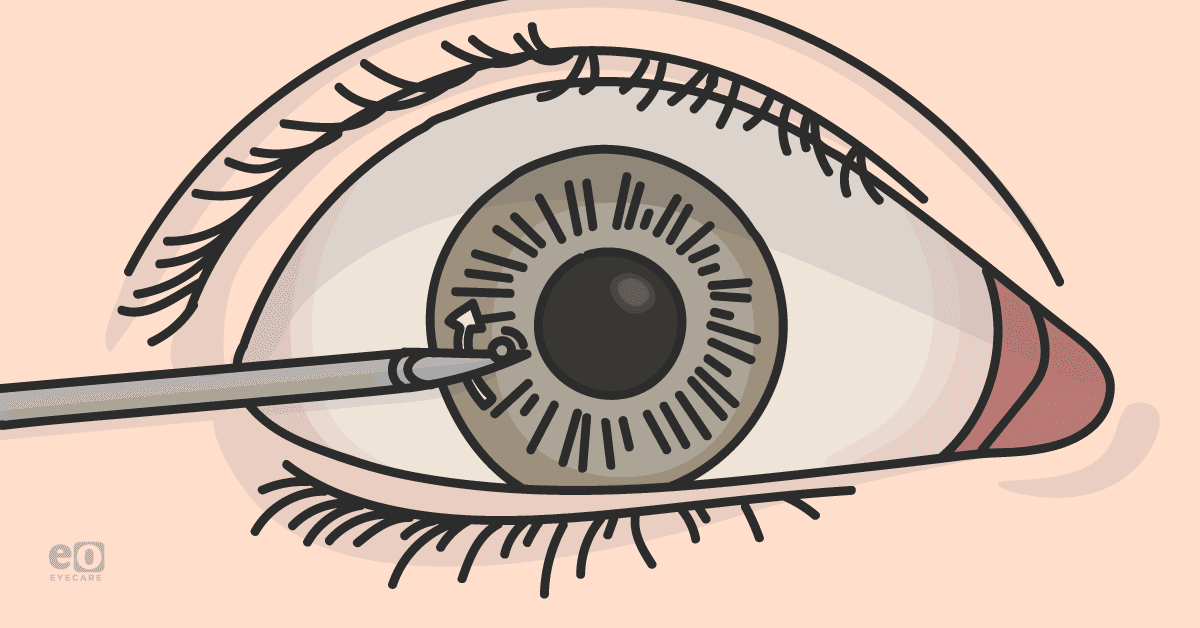
- If it’s determined that the foreign body is superficial, using a moist cotton tip or lavage may be sufficient for removal.
- If embedded, a needle or pair of fine forceps may be used to gently dislodge and lift the foreign body away from the cornea with an upward force.
Download the 5 Procedures Cheat Sheet!
Temporal artery biopsy3,4
After identifying the temporal artery and administering local anesthetics, here are the steps involved in performing a TAB:
- Begin by making a skin incision with a 15-blade scalpel.
- Next, bluntly dissect the fascia layer overlying the temporalis muscle, where the temporal artery will be located immediately deep into this fascia.
- Continue dissecting the fascial plane to expose at least three centimeters of the temporal artery.
- Using a needle driver, pass two silk ties, each beneath the proximal and distal ends of the temporal artery.
- Excise the temporal artery by cutting the proximal and distal ends of the vessel between the two sutures placed on either end. Cauterize the arterial stumps that are left behind.
- Then achieve hemostasis, perform wound closure, and dress the wound.
Canthotomy and cantholysis5,6
To perform lateral canthotomy and cantholysis:
- Begin by locally anesthetizing the area proximal to the lateral canthus and using blunt-tipped scissors to create a full-thickness cut of the canthus. Optionally, hemostats may be clamped for one minute at the lateral canthus before incision to reduce bleeding.
- Once the amount has been made, use large tooth forceps to grasp the eyelid and expose the lateral canthal tendon with gentle anterior traction.
- Cut the tendon to decompress the globe.
The eyelid should move away from the globe once released by the forceps and note rapid decreases in intraocular pressure upon successful cantholysis.
Cataract surgery: phacoemulsification and intraocular lens implantation–“divide and conquer”7,8
“Divide and conquer” technique
- Performing this cataract surgery begins by dilating the pupil with topical drops of choice. Additional mydriatics may be given intraoperatively once access to the anterior chamber has been achieved.
- Administration of local anesthesia, whether via topical drops or through peri- or retrobulbar blocks, will then be performed. Rarely will general anesthesia be administered, though this is typically reserved for pediatric patients or those with a mental state that would prevent a safe surgery.
- Once adequate anesthesia is achieved, create a paracentesis by passing a side port blade through the cornea at the limbus.
- Through the paracentesis, insert a cannula and fill the anterior chamber with dispersive viscoelastic ensuring not to overfill and cause sudden increases in intraocular pressure.
- Continue injecting the viscoelastic as the cannula is withdrawn from the paracentesis to evacuate air bubbles.
- Following this, create a larger, precise corneal incision that should be large enough to accommodate an intraocular lens (IOL) cartridge. Typically, this second incision is placed about 60 degrees apart from the paracentesis and often in the temporal quadrant, though a superior main incision can also be used.
- The next step is the capsulorhexis, which in most cases is the removal of the anterior lens capsule. In select cases, the posterior lens capsule may also be removed.
Performing capsulorhexis
- With forceps, gently pull the flap with tangential force to reduce the risk of radially developing a tear.
- Once the anterior capsule is removed, perform hydrodissection by placing a hydrodissection cannula beneath the capsulorhexis and injecting a balanced salt solution until the lens moves freely.
- With the cortex exposed, introduce the phaco tip and begin creating a vertical groove through the nucleus.
- Once a track has been carved through the nucleus, submit another instrument through the paracentesis and, using both the second instrument a phaco tip, apply lateral force to crack the nucleus.
- Spin the nucleus 90 degrees perpendicular to the first.
- Crack the nucleus again in this new groove; the result should be four nuclear quadrants.
- With the phaco tip, aspirate the quadrants using ultrasound energy as necessary to break up the nuclear fragments.
- Use the second instrument to guide the fragments to the phaco tip while also protecting the posterior capsule.
- Follow this with removing the epinucleus and stripping the cortex from the capsule in an anterior to posterior fashion.
- Finally polish the posterior capsule to remove any remaining cortical debris. After injecting the anterior chamber and capsular bag with viscoelastic, polish the anterior capsule.
IOL implantation will now be performed.
- Load the IOL into the injector and through the clear corneal incision.
- Place it into the eye and guide it gently into the capsular bag; the IOL will slowly unfurl as it is being placed. The orientation of the IOL haptics should appear to be a backward “S” when appropriately placed. The axis of haptic alignment is especially important when using toric lenses and should align with markers typically made preoperatively.
- Once the IOL is properly positioned, the remaining viscoelastic in the capsular bag and anterior segment should be aspirated.
- Finally, seal the incisions with stromal hydration and refill the eye with a balanced salt solution to ensure normal intraocular pressure.
- Assess for leaks at the incision sites and place a single 10-0 suture or sealant if any concern is.
- Finish by shielding the eye, using a patch if the eye was given more than topical anesthesia.
Open globe repair9,10
Plan B, C, and beyond
Don't forget to download the 5 Procedures for Ophthalmology Residents Cheat Sheet.
References
- Guier CP, Stokkermans TJ. Cornea Foreign Body Removal. 2021 Aug 25. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan–. PMID: 32119365.
- Murchison, AP. Corneal Abrasions and Foreign Bodies.2022 May. [nternet] Merck Manual Professional Version. https://www.merckmanuals.com/professional/injuries-poisoning/eye-trauma/corneal-abrasions-and-foreign-bodies.
- Chase E, Patel BC, Ramsey ML. Temporal Artery Biopsy. 2022 Jan 21. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan–. PMID: 29262071.
- Bowling K, Rait J, Atkinson J, Srinivas G. Temporal artery biopsy in the diagnosis of giant cell arteritis: Does the end justify the means? Ann Med Surg (Lond). 2017 Jun 15;20:1-5. doi: 10.1016/j.amsu.2017.06.020. PMID: 28663795; PMCID: PMC5479941.
- Ballard SR, Enzenauer RW, O'Donnell T, Fleming JC, Risk G, Waite AN. Emergency lateral canthotomy and cantholysis: a simple procedure to preserve vision from sight threatening orbital hemorrhage. J Spec Oper Med. 2009 Summer;9(3):26-32. PMID: 19739474.
- Desai NM, Shah SU. Lateral Orbital Canthotomy. 2021 Oct 27. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan–. PMID: 32491408.
- Carifi G, Miller MH, Pitsas C, Zygoura V, Deshmukh RR, Kopsachilis N, Maurino V. Complications and outcomes of phacoemulsification cataract surgery complicated by anterior capsule tear. Am J Ophthalmol. 2015 Mar;159(3):463-9. doi: 10.1016/j.ajo.2014.11.027. Epub 2014 Nov 26. PMID: 25461300.
- Hausheer, JR. Basic Techniques of Ophthalmic Surgery. 3rd ed. American Academy of Ophthalmology; 2019.
- Blair K, Alhadi SA, Czyz CN. Globe Rupture. 2022 Jan 31. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan–. PMID: 31869101.
- Jordan DR, Dutton J. The Ruptured Globe, Sympathetic Ophthalmia, and the 14-Day Rule. Ophthalmic Plast Reconstr Surg. 2021 Sep 28. doi: 10.1097/IOP.0000000000002068. Epub ahead of print. PMID: 34593714.