When you encounter a patient with an eyelid abnormality that causes a functional or cosmetic defect or a growth or lesion that looks a little suspicious, the next best step is to refer to an oculoplastic surgeon. Here’s what to know about
referring patients for an oculoplastics consult.
Who are oculoplastic surgeons?
Oculoplastic surgeons are ophthalmologists who specialize in defects of the eyelid, tear ducts, and eyebrows; it is a
specialty at the intersection of ophthalmology, plastic surgery, and dermatology. Some oculoplastic surgeons (usually those associated with larger academic medical centers) also perform more invasive orbital procedures such as orbital decompressions, enucleations, or eviscerations.
Who refers to oculoplastic specialists?
Referrals to oculoplastic surgeons come from many sources, primarily from other ophthalmologists who do not specialize in oculoplastics, MD/DOs of other specialties including dermatology or endocrinology, and of course,
optometrists—the primary care providers for eyes.
Some general ophthalmologists or optometrists in certain states (Alaska, Kentucky, Louisiana, and Oklahoma) will perform their own minor in-office lid procedures such as
chalazion removal, but for anything more specialized or invasive, most will refer to an oculoplastic specialist.
What conditions should I refer to an oculoplastic surgeon?
As there is a vast array of procedures an oculoplastic surgeon has learned to perform, many choose to focus on a specific subset of this long list. Jenny Temnogorod, MD, the oculoplastic surgeon of
Shoreline Eye Group in Connecticut, says, “This is very individualized, especially as surgeons are becoming more and more specialized and selective regarding what surgeries they want to perform.”
Conditions treated by oculoplastic specialists
1) Ptosis: Note, first, it’s imperative to rule out any sinister causes of ptosis that may be time-sensitive, such as Horner’s Syndrome
2) Dermatochalasis
3) Eyelid lumps and bumps, including chalazia that have not resolved on medical therapy alone and are bothersome to the patient and questionable skin lesions that may warrant a biopsy:1
As a referring doctor, there are things to consider when you see these lesions, including:
a) History and risk factors, including prior skin cancer, fair skin, previous radiation, and immunosuppression
b) Gradual enlargement
c) Clinical Features
- Ulceration
- Induration (hardening)
- Irregular or “pearly” borders
- Disruption of normal eyelid contour
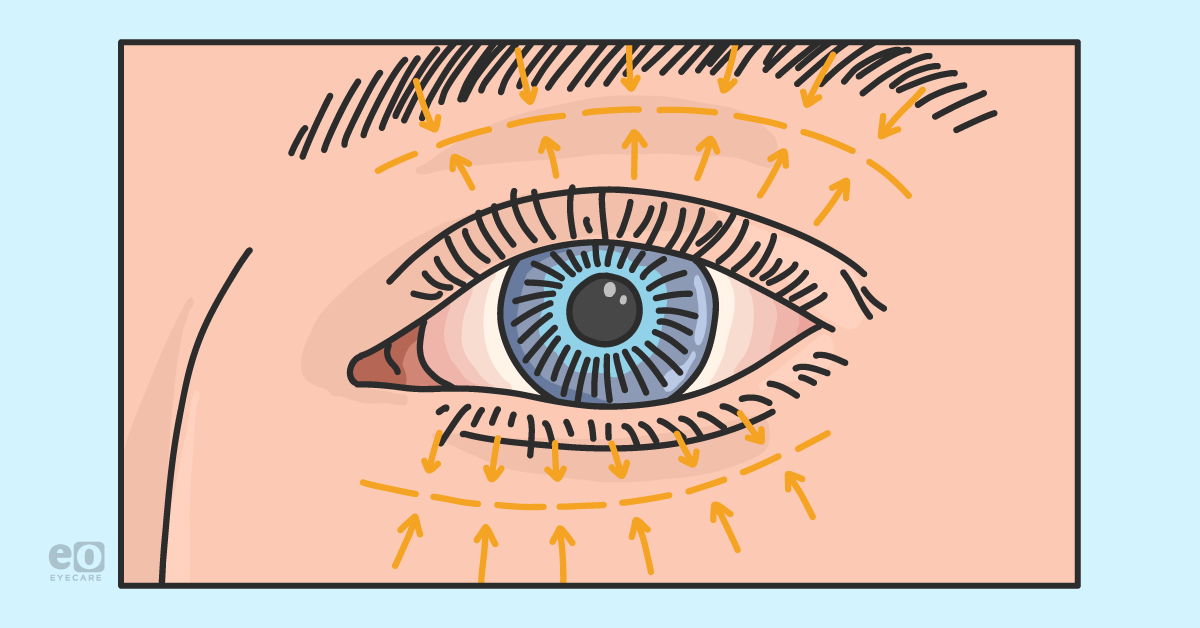
- Madarosis (lash loss, not due to blepharitis, chemotherapy, trauma, or trichotillomania)
- Telangiectasia
- Reduced sensation
4) Rhytids (fine lines in the skin that can be treated with Botox or Dysport injections)
5) Blepharospasm or hemifacial spasm: Note, imaging may need to be done prior to this referral to rule out a sinister cause such as a tumor of the cerebellopontine angle
6) Thyroid eye disease
7) Lagophthalmos
8) Eyelid reconstruction, following Mohs surgery or other event
9) Nasolacrimal duct obstruction
Are there conditions for which I should NOT refer to an oculoplastic specialist?
While oculoplastic specialists are ophthalmologists, most do not perform
cataract surgery or other anterior segment surgery. For example, a pterygium that is causing significant discomfort and/or impacting visual function should be referred to a general ophthalmologist or
cornea specialist. Additionally, most oculoplastic specialists outside of large academic medical centers (unless otherwise specified) do not perform more invasive orbital procedures such as decompression, enucleation, or evisceration.
Finally, traumatic orbital pathology, severe infection, orbital fractures, and other urgent matters should be sent to an
emergency department, ideally at an academic facility.
What information is most helpful to include in an oculoplastics referral?
Oculoplastics referral checklist
According to Dr. Temnogorod, the following clinical information is helpful to include:
- The last, or last few, exam notes, including exam findings and past ocular/medical history.
- A specific description of the problem to be addressed, especially for eyelid lesions (e.g., whether the lesion is located near the punctum and/or on the lid margin), as this can assist in planning whether a procedure could potentially be performed on the day of the consultation or will likely need to be scheduled for surgery in the operating room.
- Humphrey Visual Field Superior 36 performed with lids taped and untaped; most insurance companies require >30% of a superior visual field defect that improves when the lids are taped (i.e., is not caused by another pathology such as glaucoma). Even if the fields do not meet this criteria but eyelid droop appears to be clinically significant and/or the patient reports it is affecting their vision, send the referral anyway; often, patients in this category have habituated to raising their eyebrows while taking these tests and will meet insurance criteria when retested with careful coaching.
Additionally, the following are helpful for documentation, but oculoplastic specialists will likely repeat these tests themselves:
- MRD 1, 2, 3: Margin-to-reflex distance measurements—here’s a refresher on MRD’s
- Exophthalmometry
- Anterior photos
What does a referring doctor need to know about insurance, billing, and coding?
As there are many eyelid/periorbital abnormalities, there are many
ICD-10 and CPT codes that go along with them. A referring doctor should know (and should set expectations for the patients they refer. Explain that if an eyelid abnormality is deemed cosmetic (i.e., it does not meet certain criteria for its
functional impact on the patient’s vision), it does not have features causing concern for malignancy, and/or it is not causing discomfort, it will not be covered by medical insurance.
Out-of-pocket fees may vary drastically—a benign, simple eyelid bump removal may be $100, while a cosmetic blepharoplasty will cost thousands. It is best to discuss fees with the specific specialist(s) to whom you refer.
The bottom line
The bottom line:
Communication is essential to any good referral relationship, so it is a good practice to establish a relationship with your local oculoplastic specialist(s) sooner rather than later. Dr. Temnogorod says “It is important to have a conversation with the individual oculoplastic surgeon to whom you refer to or are considering referring to and ask what kinds of conditions they specialize in evaluating and which surgeries they do or don’t perform.” Knowing this will save time and resources for the referring doctor, the patient, and the specialist.
And when in doubt? Ask questions and discuss cases with your specialist. As Dr. Temnogorod, who also goes by “Dr. Jenny” offers, “I’m always available by phone if a referring doctor would like to discuss any case.”