Vision plays an essential role at every stage of life but is especially critical during the formative early years, as children begin to shape their perception of the world through sight. When vision is impaired, it affects not only how a child sees the world but also other developmental domains, such as psychosocial and learning.1,2
In the United States, nearly 50% of children with blindness have a retinal disease,3 which is among the leading causes of blindness in most parts of the world.4
Despite the overlap in the clinical workflow of an adult patient, the examination of a pediatric patient with suspected retinal disease requires special considerations, including knowing the age norms and prioritizing the posterior pole assessment and retina evaluation.
Subjective testing and clinical examination for pediatric retinal diseases
Signs and symptoms of pediatric retinal disease can vary significantly by age group. It is important to first benchmark age norms for visual behavior and visual acuities.
Table 1: Visual behavior and acuity expectations for pediatric populations.5,6
| Age | Visual Behavior or Visual Acuity |
|---|---|
| 2 to 4 months | Tracking moving objects |
| 5 to 8 months | Object and face recognition |
| 9 to 12 months | Visually-guided reach |
| 2.5 to 3 years | 20/63 or better |
| 3 to 4 years | 20/50 or better |
| 4 to 5 years | 20/40 or better |
| 5 to 6 years | 20/32 or better |
Table 1: Courtesy of the American Academy of Ophthalmology and Pan et al.
Deviations from these age-appropriate vision milestones, when best corrected or for parental concerns of difficulties seeing in specific lighting conditions (i.e., photophobia or nyctalopia), should prompt suspicion for a retinal condition. Nystagmus, though not pathognomonic, classically presents with congenital retinal disorders and should certainly raise flags for further evaluation.7
Subjective testing for pediatric patients with suspected retinal disease
- Visual acuity
- Color testing
- Visual field
In addition to visual acuity and signs and symptoms, other subjective tests can provide more pieces to the clinical picture. Color vision should be assessed because it is attributable to retinal photoreceptor function. Common pediatric screening tests include Color Vision Testing Made Easy (CVTME) color plates, Waggoner HRR Diagnostic Test color plates, and Ishihara pseudo-isochromatic plates.
Formal visual field testing can be difficult for young children, but the visual field can be estimated via visually evoked saccades or head movements. Early work has explored the options of virtual reality perimetry,8 eye-movement-based perimetry,9 and a dome-shaped pediatric perimeter device for children.10
Clinical evaluation for pediatric patients with suspected retinal disease
- History
- Dilated fundus examination (DFE)
When framed creatively, a clinical test can turn into a fun game or activity. Calling a retinoscope and ophthalmoscope a flashlight can capture glances to accumulate the clinical information needed. While checking refractive error and posterior segment, spot how many gummies are in there, or guess what the child ate for dinner last night.
Looking at the posterior pole is non-negotiable to form a differential diagnosis, so sequence the examination according to the child’s cooperation. When pediatric patients are uncooperative with dilation drops, parents can be given drops to bring home and instructed to instill prior to the next appointment, preferably when the child is just waking up.
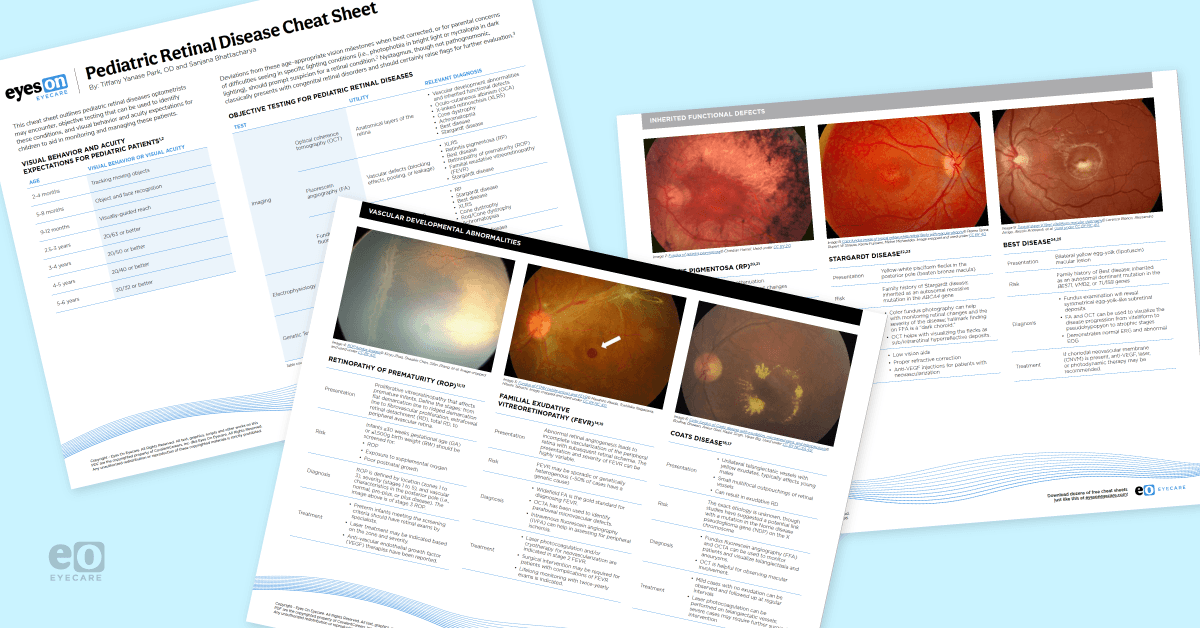
Download the Pediatric Retinal Disease Cheat Sheet here
Download the cheat sheet with 12 clinical images here

Pediatric Retinal Disease Cheat Sheet
Use this cheat sheet with visual behavior/acuity expectations, objective testing recommendations, and fundus photographs of 12 pediatric retinal diseases to review must-know facts about these conditions.

Differential diagnoses for pediatric patients with suspected retinal disease
Forming a list of possible diagnoses that can potentially explain the child’s signs and symptoms is the next critical step.
Common pediatric retinal conditions, categorized by etiology with key signs and symptoms, include:
- Congenital structural defects
- Persistent fetal vasculature (PFV): Cataract with white stalk extending to optic nerve and retina
- Coloboma: White, well-defined defect; often associated with CHARGE syndrome
- Oculo-cutaneous albinism (OCA): Transillumination defects of the iris, foveal hypoplasia, decreased pigment
- Infectious
- Toxoplasmosis: Exposure to cats, pigmented scars +/- vitritis (“headlight in fog”)
- Toxocariasis: Exposure to dog/cat feces, granuloma with vitritis
- Vascular development abnormality
- Retinopathy of prematurity (ROP): Neovascularization associated with gestational age < 30 weeks, birthweight < 1500g, and exposure to supplemental O2
- Familial exudative vitreoretinopathy (FEVR): Genetic disease of avascular peripheral retina with vessel dragging
- Coats disease: Unilateral telangiectatic vessels with yellow exudates, typically affects young males
- Cancer
- Retinoblastoma: White/cream retinal mass presenting as leukocoria, often with proptosis and strabismus
- Inherited functional defects
- Retinitis pigmentosa (RP): Arterior attenuation, bone spicule pigment changes, and waxy disc pallor
- Stargardt disease: Yellow flecks in the posterior pole
- Best disease: Bilateral yellow egg-yolk macular lesion
- X-linked retinoschisis (XLRS): Affects young males, radial spoke-wheel pattern at fovea
- Acquired
- Penetrating trauma: Can present with vitreous hemorrhage, retinal detachment (RD), and/or vitreous prolapse
Figures 1, 2, and 3: Fundus images of FEVR, retinitis pigmentosa, and retinoblastoma, respectively.
- Figure 1: Fundus of FTMH (white arrow) and FEVR© Masahiro Akada, Toshihiko Nagasawa, Hitoshi Tabuchi. Image cropped and used under CC BY-NC 4.0.
- Figure 2: Fundus of retinitis pigmentosa© Christian Hamel. Used under CC BY 2.0.
- Figure 3: Ocular fundus aspect of retinoblastoma© Isabelle Aerts, Livia Lumbroso-Le Rouic, Marion Gauthier-Villars, et al. Used under CC BY 2.0.
To see more fundus images of pediatric retinal diseases, download the cheat sheet!
Objective testing to confirm the diagnosis
Confirmatory testing can be completed by objective testing:
- Imaging
- Optical coherence tomography (OCT)
- Fluorescein angiography (FA)
- Fundus autofluorescence (FAF)
- Electrophysiological testing
- Electroretinography (ERG)
- Electro-oculography (EOG)
- Visual evoked potentials (VEP)
- Genetic testing
Selecting which tests to perform is dependent on the leading differential diagnosis.
Table 2: Ancillary testing that can be used to confirm a diagnosis with their respective utility and relevant differential diagnoses.
| Testing | Test Type | Utility | Relevant Diagnoses |
|---|---|---|---|
| Imaging | OCT | Anatomical layers of the retina | Vascular development abnormalities and inherited functional defects, OCA, XLRS, cone dystrophy, achromatopsia, Best disease, Stargardt disease |
| FA | Vascular defects (blocking effects, pooling, or leakage) | XLRS, RP, Best disease, ROP, FFEVR, Stargardt disease | |
| FAF | Abnormal lipofuscin | RP, Stargardt disease, Best disease, XLRS, cone dystrophy, rod/cone dystrophy, achromatopsia | |
| Electrophysiology | ERG | Function of photoreceptor and inner retina | Stargardt disease, XLRS |
| EOG | Function of photoreceptor-retinal pigment epithelium (RPE) complex | Best disease | |
| Genetic testing | Confirm diagnosis with causative gene mutation, establish risk to family, and determine eligibility for clinical trials and treatments | Stargardt disease, Best disease, RP, XLRS, OCA, FEVR, cone dystrophy and variants |
Table 2: Courtesy of Tiffany Yanase Park, OD, and Julie Rodman, OD, MS, FAAO.
Management of pediatric retinal diseases
For pediatric patients, prompt treatment followed by early referral for low vision services is integral to preserving visual function and quality of life.
Therefore, the management of pediatric retinal diseases entails:
- Treatment: Medical or/and surgical
- Low vision services
Determining treatment options for a child with retinal conditions is complex and multifactorial. The general goals of treatment are to slow or stop the progression of the disease as well as preserve, improve, or restore vision.
This may be accomplished with pharmaceutical medicines administered topically or intravitreally as well as with surgery. Though diagnosis may not occur until the child has experienced significant vision loss, initiating the appropriate treatment early can result in more favorable visual outcomes.
The importance of low vision services
Managing pediatric patients with retinal diseases also involves partnering with them and their families as they navigate the next steps following a diagnosis. Children with visual impairment can benefit from resources to support their development, but often need a point in the right direction.
The role of patient advocate by optometrists and ophthalmologists should increasingly be recognized, as they play a crucial part in a child’s interdisciplinary team. Low vision rehabilitation can effectively address the current vision of the child with tools and devices to improve functional vision.11
These services are often in tandem with individual family service plans (IFSP) or individual education plans (IEP). Care coordination is offered by local or regional centers as well as private sector agencies to detangle a network of resources to address the child’s specific needs. Counseling and support groups can also decrease the psychological impact of visual impairment.
Final thought
There are certainly many challenges that come with visual impairment; however, optometrists and ophthalmologists can empower these children and their families with a thorough clinical workup and diagnosis, as well as with education and resources.
Eyecare practitioners must understand the resources and specialists in their area where they can direct their pediatric patients with suspected retinal disease.