Traumatic corneal foreign body injuries account for 8% of primary care eye clinic visits in the US.1 Patients present with a red, painful, watery, photophobic eye with foreign body sensation.1
The foreign body (FB) material and nature of the injury influence the treatment and prognosis.1 Optometrists working in primary care have the necessary expertise and equipment for FB removal.
This article briefly reviews corneal wound healing, discusses the importance of taking a thorough history, and outlines best practices for non-penetrating corneal FB removal and management.
The process of corneal wound healing
The corneal epithelium is replenished every week.2 The process occurs faster during corneal wound repair and consists of four phases: latent, migration, cell proliferation, and attachment.2,3
The time to resolution depends on the patient's age, the depth of the defect, the type of injury, and co-morbidities, like diabetic neuropathy and immunological disease.4 See Figure 1 below for the basic anatomy of a human cornea.
The 4 phases of corneal wound repair
The latent phase begins within an hour of the injury and clears dead cells and debris whilst preparing an extracellular matrix and cellular processes for the migration phase.2,3 Now, basal epithelia migrate centripetally in a linear fashion to form a monolayer that covers the defect.2,3
During this process, they form convex shapes and eventually “Y” shaped contact lines that may be mistaken for dendritic lesions.2,3,5 A whorl-like pattern is often seen around the contact lines where epithelial cells migrate at different rates.2,3,5
In the cellular proliferation phase, limbal stem cells are activated, and the basal epithelia replicate mitotically to restore corneal thickness.2,3 Both migration and cell proliferation phases take place over 24 to 36 hours.2,3
In stromal defects, fibroblast proliferation begins at this stage, replacing the damaged keratocytes in 24 to 72 hours, but complete stromal remodeling occurs within 2 years.2,3 Lastly, during attachment hemidesmosomes and anchoring filaments begin forming when the overlying stratified epithelial layers are established, but they take anywhere from 6 to 8 weeks to a year to fully form.2,3
Endothelial cell damage results in edema, and cells cannot replicate by mitosis, thus increasing in size and shifting to replace the lost cells. This starts 6 hours after the injury and is completed in a week.2,3
Figure 1 highlights a sagittal cross-section of a human cornea.
Figure 1: Courtesy of Jasraj Singh Bhangra BSc, PgCert, MCOptom.
Obtaining a thorough patient history
A thorough patient history should be structured around the “what, when, where, and how” technique of questioning, and patients should be asked about previous ocular injuries, infections or surgery, co-morbidities, and contact lens wear.4,6
What:
What type of FB is it? Organic FBs are more likely to cause bacterial or fungal infections than inorganic FBs.6,7 Ferrous metals react with salts in the tear film, producing rust rings.6 See Table 1 below for examples of common organic and inorganic FBs.4,7
When:
The longer the FBs have been in the cornea, the more likely an inflammatory and infectious response will ensue unless the FB is inert.6 Metallic, ferrous FBs form a rust ring as early as 4 hours after entering the cornea and must be removed promptly to avoid stromal necrosis.8,9,10
Where:
Ask if the patient was injured during work duties or in their personal time and if they were wearing safety eyewear.6 This information is important for compensation and insurance purposes and must be carefully documented in line with company policies.6
How:
High-velocity impact injuries from hammering, grinding, explosions, and the use of power or machine tools are likely to penetrate the globe and, therefore, require careful examination.
This exam can be performed with gonioscopy, a dilated fundus examination, and possibly imaging with computed tomography, anterior segment-optical coherence tomography (AS-OCT), B-scan ultrasonography, X-rays, and magnetic resonance imaging (MRI).1,4,6,7,11 MRI is contraindicated if the FB is metal.6
Table 1 outlines common organic and inorganic foreign bodies. Materials with asterisks are inert FBs.
| Organic | Inorganic |
|---|---|
| Vegetative material | Metals |
| Seeds | Aluminum* |
| Insect parts | Copper |
| Caterpillar hair | Iron |
| Parts of trees | Glass* |
| Wood | Plastic* |
| Fiberglass* | |
| Stone* |
Table 1: Courtesy of Jasraj Singh Bhangra BSc, PgCert, MCOptom.
Examining and removing corneal FBs
6 clinical pearls for examining a patient with a corneal FB:
- Check visual acuity: Measure best-corrected visual acuity. Ensure you note amblyopia or any poor vision in the affected eye prior to FB removal.4,6
- Instill a topical anesthetic to help with the examination if symptoms are severe.4,6
- Slit lamp exam: View the ocular adnexa with white light and diffuse illumination on slit-lamp examination. Note any eyelid edema, conjunctival hyperemia, and hyphema.6 A peaked iris suggests ocular penetration.4,6
- Assess the FB in an exam: Evert the eyelids to look for any FBs or particles.4,6
- Assess the FB with imaging: Use a corneal section, and if possible, AS-OCT to assess the type, location, size, and depth of the corneal FB.4,6
- Check the anterior chamber (AC): Assess the depth and lens of the AC. A shallow AC or lens opacities signify a penetrating injury. Note any cells or flare.4,6
- Perform a Seidel test: Instill Fluorescein 2%, use the cobalt-blue filter, and look for a “dark waterfall’’ appearance, which is a positive Seidel sign (aqueous humor leaking from the AC onto the ocular surface) indicating corneal penetration.
- Corneal defects from small penetrating FBs can self-seal and thus will show a negative Seidel sign.4,6
5 steps for safe corneal foreign body removal:
- Anesthetic: Instill a topical anesthetic in the affected eye.4,6
- Irrigation: Irrigate the eye with saline to remove a superficial corneal FB and particles. If unsuccessful, see the third bullet.4,6
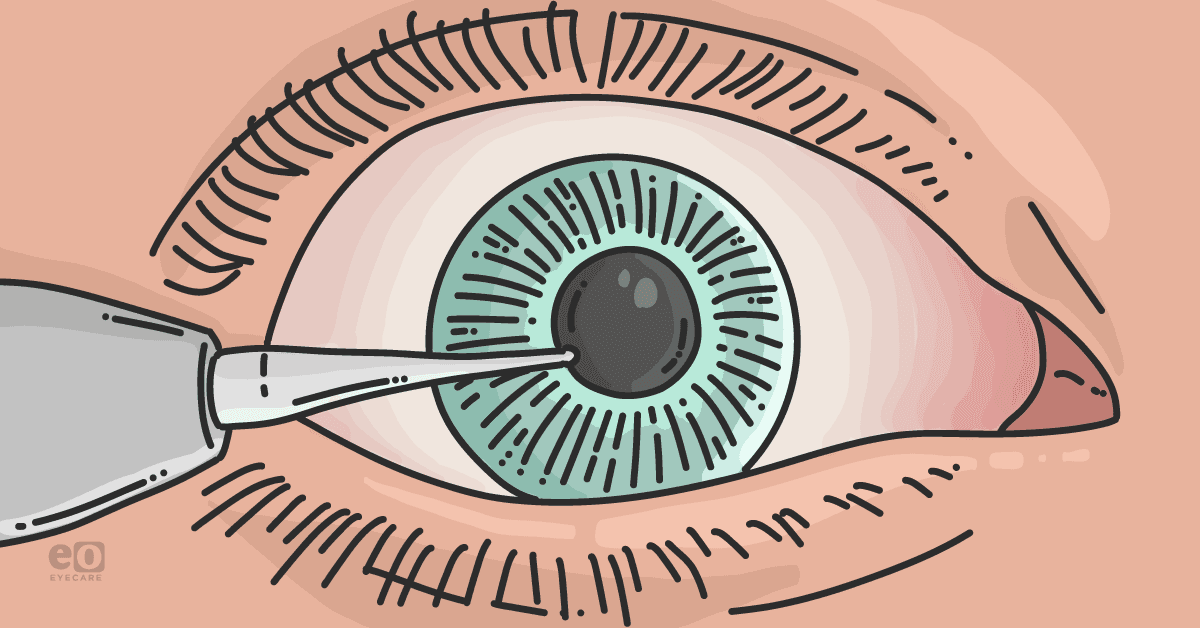
- Select a tool to remove the FB: Take a 23- to 25-gauge needle attached to a disposable syringe or a FB spud (magnetic ones are effective for removing metal FBs without disrupting surrounding tissues) and hold it between your index finger and thumb, resting your hand on the slit lamp bar.4,6,10
- Cotton-tipped applicators can be used for swiping the very superficial FB on the conjunctiva, but are not advised for removing corneal FBs, especially deeper FBs, as it will likely push them further back.4,6 Protruding FBs can be removed with jeweler’s forceps.4,6 See Figure 2.
- Remove the FB: Approach the cornea with the bevel of the needle facing you and at a tangent to the ocular surface.4,6,12 The tip of the needle can be bent using a sterile needle driver or the needle cap, so that it is approximately perpendicular to the shaft of the needle.4,6,12 See Figure 2.
- This technique reduces the likelihood of you perforating the cornea, thus allowing you to dislodge the FB easily by placing the tip just behind the FB and lifting it off.4,6,12
- Managing metal FBs: Use an alger brush to remove as much of the rust ring as possible from ferrous metal FBs. This electric dental burr automatically stops when it meets Bowman’s layer, so you are unlikely to scar the cornea, especially if the rust ring covers the visual axis.4,6,10
- However, for anterior stromal or slightly deeper FBs, it should be used very carefully, as the automatic stop will not work.4,6,10 Alternatively, you can scrape the rust out with a needle or FB spud in this case.4,6,10
Commonly used tools for removing corneal FBs
Figures 2 to 6 below show tools frequently utilized by eyecare practitioners to remove corneal foreign bodies.
Figure 2 demonstrates the tip and bevel of a 23-gauge needle.
Figure 2: Courtesy of Jasraj Singh Bhangra, BSc, PgCert, MCOptom.
Figure 3 illustrates a 23-gauge needle needle with a bent tip and bevel.
Figure 3: Courtesy of Jasraj Singh Bhangra, BSc, PgCert, MCOptom
Figure 4 highlights a cotton-tipped applicator.
Figure 4: Courtesy of Yevhen Borysov.
Figure 5 shows a 23-gauge needle with a cap and disposable syringe.
Figure 5: Courtesy of Jasraj Singh Bhangra, BSc, PgCert, MCOptom.
Figure 6 demonstrates jeweler’s forceps.
Figure 6: Courtesy of Jasraj Singh Bhangra, BSc, PgCert, MCOptom.
Strategies for managing corneal foreign bodies
An epithelial defect that covers less than 60% of the corneal surface recovers in 1 to 4 days whilst larger or deeper defects take up to a week to resolve.1,13 After corneal FB removal, the mainstay of management is to prescribe a broad-spectrum topical antibiotic to use four times daily for prophylaxis until re-epithelialization of the defect, and it must cover against pseudomonas infection in contact lens wearers.1,4,6,9
Medical therapies
Topical fluoroquinolones are the preferred drug of choice, but aminoglycosides and macrolides are occasionally used. Initiating treatment within 18 hours of the injury may reduce the likelihood of microbial keratitis.1,9,14,15
Ointments are preferred to eye drops as they allow for increased contact time on the ocular surface, reduced friction between the eyelids and the cornea—facilitating faster healing of the corneal epithelium, increased comfort, and can soften corneal rust so it is easier to remove after 24 hours.1,13 The patient should be asked about any allergies to medication they have before prescribing.
Topical non-steroidal anti-inflammatories and anesthetics reduce pain, but may hinder corneal wound healing; therefore, a mydriatic like cyclopentolate 1%, can be prescribed for 3 to 5 days to reduce ciliary spasm and oral analgesia taken as required.1,4,6,13,16,17
Bandage contact lenses
Bandage contact lenses (BCLs) offer a protective barrier by covering the defect and reducing friction between the eyelids and cornea, allowing better adhesion between the basal epithelia, their basement membrane, and the anterior stroma.6,18,19
This reduces the likelihood of recurrent corneal erosions (RCE).20 BCLs are used for larger defects that are not caused by organic FBs; they must be replaced monthly and are used with topical fluoroquinolones.6
Patients should be counseled not to get water into the affected eye due to the risk of acanthamoeba keratitis.20 Corneal wounds covered by BCLs heal faster than with pressure patching (PP), and PP causes more pain in the first 24 hours of treatment.18,19,21,22
Topical steroids may be used to treat an infiltrative keratopathy with active ulceration 48 hours after starting a topical antibiotic as long as the epithelial defect is healing or, to reduce inflammation and scarring in defects penetrating Bowman’s layer, only once the affected cornea has re-epithelialised.6,7,9,13,23 They are contraindicated in defects caused by organic FBs as it increases the risk of a severe fungal infection.6,7
Amniotic membranes
Amniotic membranes (AMs) are indicated in RCEs or persistent epithelial defects (PED) in conditions like herpetic, neurotrophic, bullous, or immunological keratopathy for their pro-epithelialization, anti-inflammatory, and antimicrobial properties.24,25,26 They are derived from fetal tissue and consist of an epithelial monolayer with a basement membrane and an avascular stroma.24,25,26
Amniotic membranes can be applied in three ways:
- Inlays: A corneal surgeon integrates it into the corneal stromal, epithelial side up, to replace lost tissue.24,27
- Outlays: Placed epithelial side down over the defect to encourage healing and limit scarring.24 They are removed or dissolve after a few weeks.24 Optometrists are likely to take this approach using sutureless grafts.27
- Sandwich transplant: A combination of an Inlay and Outlay to increase chances of recovery.24
Depending on the etiology and depth of the corneal ulcers treated with AMs, they tend to heal within 3 days to 4 weeks, but it can take up to 3 months for complete re-epithelialsation.24,26,27
However, in the rare instance that AMs fail to heal defects such as PEDs or neurotrophic ulcers; autologous platelet-rich plasma derived from the patient’s blood is an alternative therapy that contains growth factors and antimicrobial products that stimulate regeneration of the corneal epithelium.28
Epithelial defects that are central, large, deep, associated with contact lens wear, or needing rust removal require a follow-up in 24 to 48 hours; then, extend as needed until resolution.1,4,6,14,29 Otherwise, they can be reviewed in 2 to 3 days or even discharged without follow-up if they are symptom-free 1 to 2 days after treatment.1,6,14
Inert FBs embedded in the peripheral cornea in an asymptomatic patient do not require removal.9,29 Suspected penetrating injuries must be referred immediately to the hospital emergency department.6
In closing
Optometrists should manage corneal FB removal within the scope of their practice, as set out by state law and within the limits of their competence.
A detailed history and examination, including necessary imaging, careful technique, judicious use of medication, and strict follow-up, can ensure good outcomes. Protective eyewear must be advised for future prevention.