Uveal melanoma is the most common tumor originating inside the eye.
1,2 Uveal melanoma may affect any three parts of the uveal tract (i.e., the iris, ciliary body, or choroid); however, it most commonly affects the choroid.
1,2 As there are only six cases per million, there is limited widespread knowledge regarding the exact etiology of this disease. The early presentation can be nonspecific, and
lesions may even be found on routine screening. Thus knowledge regarding risk factors, high-risk characteristics of lesions, and appropriate workup are critical to preventing the growth and spread of the primary tumor and metastasis.
Risk factors for choroidal melanoma
Age, ethnicity, and iris color are risk factors for developing choroidal melanoma. Fairer-skinned individuals with light-colored irises are more susceptible to choroidal melanoma.3
Although risk increases with age, choroidal melanoma may also occur in children. When occurring in children, the rate of iris melanoma is much higher than other uveal melanomas.
Genetic markers also indicate risk factors, prognosis, and risk of metastasis. Proto-oncogenes, like MAPK and GNAQ activation, are associated with 50% of cases of uveal melanoma, and the incidence of the HLA-B40 haplotype is implicated in uveal melanoma metastasis. The incidence of choroidal melanoma has been further investigated with BAP1 somatic gene mutations and continues to be explored due to its potential as a genetic screening tool for hereditary melanoma.4,5
Symptoms of choroidal melanoma
Symptoms may or may not be present in individuals with early disease. Symptoms that sometimes occur with choroidal melanoma include eye pain, floaters, decreased or blurred vision, and visual field loss.2
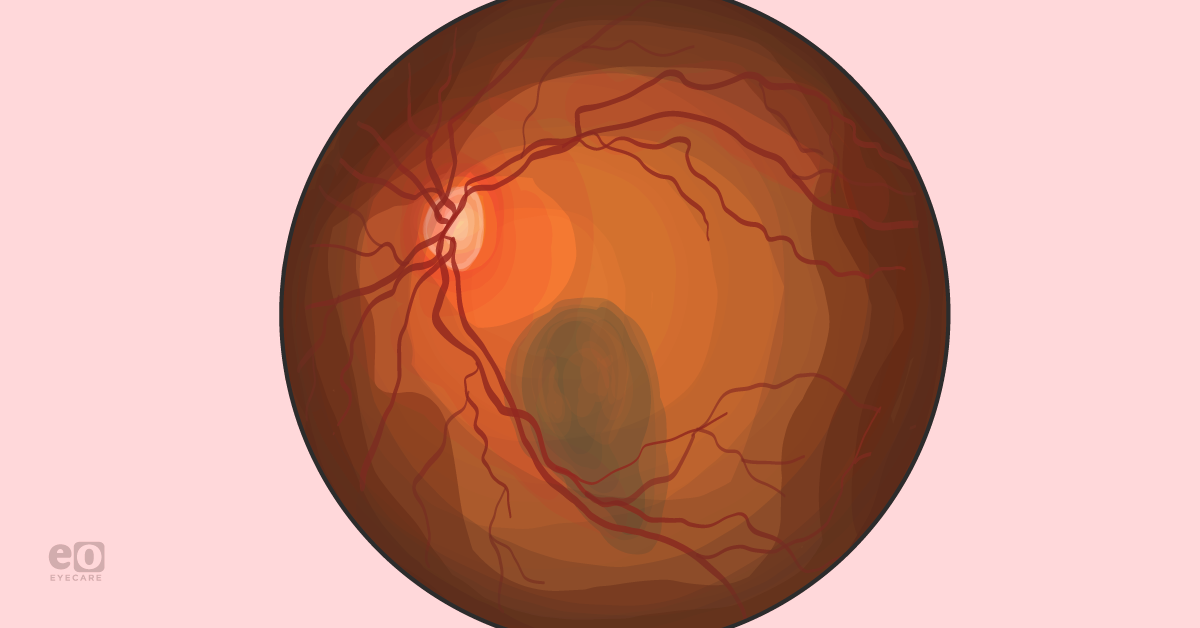
Figure 1 illustrates primary choroidal melanoma.6
Figure 1: Courtesy of Harris Ahmed, DO, MPH
Early diagnosis of choroidal melanoma can prevent metastasis. Metastasis occurs in 16% of patients with melanomas less than 4 mm thick, 32% of patients with 4-8 mm thick melanomas and 53% of patients with more than 8 mm thick melanomas.7 Prognosis depends largely on the grading and staging of the melanoma and whether or not there is metastasis.
Identifying choroidal melanoma
Often, lesions may be discovered on routine screening or follow-up for unrelated eye problems. In these scenarios, it is essential to risk stratify the lesions based on specific criteria. Studies by Shields et al. at the Ocular Oncology Service at Wills Eye Hospital have established such criteria.
Risk factors for choroidal lesions that are suspicious for melanoma include thickness greater than 2 mm, orange color pigment, subretinal fluid, the presence of symptoms, and the margin of the lesion is 3 mm or less from the disc. Additional risk factors include acoustic hollowness, surrounding halo, and absence of drusen.
Figure 2 demonstrates high-risk choroidal melanoma, classified by MOLES criteria.6
Figure 2: Courtesy of Harris Ahmed, DO, MPH
Shields et al. showed that lesion thickness is both a
risk factor and an indicator of metastasis. The thickness of the lesion by one-millimeter increments in melanoma can increase the risk for metastatic disease by 5%. If two risk factors are present, then the chance of tumor growth can be 45-50% compared to 36-38% with one risk factor (TABLE 1).
7,8Progression of high risk or diffuse choroidal melanoma can also be evaluated with MOLES criteria:
- Mushroom shape
- Orange pigment
- Large size
- Enlarging
- Subretinal fluid
Increase in risk factors increases the relative risk and tumor growth7,8
| Risk Factors | Relative Risk for Tumor Growth | Percentage of patients (1287) with small choroidal melanocytic tumors |
|---|
| None | 0 | 4% |
| Tumor thickness greater than 2 mm | 1.9 | 36-38% |
| Tumor thickness greater than 2 mm, posterior tumor margin touching the disc | 3.8 | 45-50% |
| Tumor thickness greater than 2 mm, posterior tumor margin touching the disc, visual symptoms | 7.4 | 50% |
| Tumor thickness greater than 2 mm, posterior tumor margin touching the disc, visual symptoms, orange pigment | 14.1 | 51% |
| Tumor thickness greater than 2 mm, Posterior tumor margin touching the disc, visual symptoms, orange pigment, subretinal fluid | 27.1 | 56% |
Screening for choroidal melanoma
Screening for choroidal melanoma with a dilated fundus exam is a recommended mainstay of preventive care for patients. Even before symptoms are present, routine comprehensive eye exams are responsible for recognizing one-third of choroidal melanoma cases. One dilemma with uveal melanoma is that choroidal lesions that progress to
melanoma can sometimes be confused for benign nevi.
Figure 3 represents benign choroidal nevus.
Figure 3
Suspicious pre-cancerous lesions in the choroid can sometimes be distinguished from choroidal nevi by lesion thickness greater than 2 mm, as mentioned by B-scan ultrasound. Choroidal lesions that do not have those risk factors for melanoma discussed above are most likely choroidal nevi. The potential for progression to choroidal melanoma occurs in 1 in 8,000 cases of choroidal nevi. It should be monitored with imaging modalities such as B scan ultrasound,
optical coherence tomography (OCT), and widefield fundus photography.
Managing choroidal melanoma
If a choroidal lesion is confirmed melanoma, disease management may include radiation (plaque or proton beam radiation) or enucleation when end-stage disease. Plaque radiotherapy is the standard treatment available for choroidal melanoma, which involves high dose radiation to the lesion. It is most successful for small to medium choroidal lesions with a 3% recurrence rate in 97% of patients at five years,9 and visual acuity was preserved in 50% of patients at 20/50 at ten-year follow-up.10
Due to the radiation injury risk from plaque radiotherapy in thicker and larger choroidal lesions. An investigational treatment drug called light-activated AU-0,10 developed by Aura Biosciences is in phase 1 clinical trial. It uses viral nanoparticle conjugates alongside an ophthalmic laser treatment for eliminating cancer cells in ocular melanoma patients.11
Figure 4 illustrates malignant choroidal melanoma.12
Figure 4
Genetics play a role in presenting choroidal melanoma; subsequently, anti-PD-1 monoclonal antibodies such as pembrolizumab against MAPK and GNAQ have been explored, but with little benefit in minority populations. The continuation of yearly dilated exams as well as management of any arising complications should be followed for health maintenance.
Choroidal melanoma sequelae include macular edema,
retinal detachment, neovascularization, and recurrence and are managed in follow-up after appropriate diagnosis and treatment.
Conclusions and differential diagnosis for choroidal melanoma
Although preventative measures like screening and treatment modalities are available, choroidal melanoma continues to have a high mortality rate of 62% with metastasis and 9% without metastasis.13 Disease related mortality also showed that patients with one site or more of metastasis showed 54% survival at the 7.4 year mark.13
Differential diagnosis between benign choroidal nevi and melanoma should be established early and risk factors evaluated to decrease the risk of growth and potential metastasis. Genetic targets, multimodal therapies, and investigational drugs continue to be a new source of possible treatments and disease management.
References
- Van, Poppelen NM,, et al. “Genetics of Ocular Melanoma: Insights into Genetics, Inheritance and Testing.” Int. J. Mol. Sci., no. 22, 2021, p. 336.
- B Quinn, Nicola, et al. “Prevalence and characteristics of peripheral retinal lesions in an aging population.” Invest. Ophthalmol. Vis. Sci, vol. 15, no. 8, 2017, p. 1497.
- Moss, Cathy. “New Clinical Trial for Early-Stage Eye Melanoma.” Wills Eye Hospital, 24 April 2017, https://www.willseye.org/new-clinical-trial-early-stage-eye-melanoma/. Accessed 10 April 2022.
- Luo H,, Ma C. “Identification of prognostic genes in uveal melanoma microenvironment.” PLOS ONE, vol. 20, no. 11, 2020.
- Helgadottir H, Höiom V. “The genetics of uveal melanoma: current insights.” Appl Clin Genet, vol. 9, 2016, pp. 147-155.
- Ahmed, Harris, et al. “Differential Diagnosis for a Pigmented Fundus Lesion with Downloadable Cheat Sheet.” Eyes On Eyecare, 26 January 2022, https://eyesoneyecare.com/resources/differential-diagnosis-for-a-pigmented-fundus-lesion-with-downloadable-cheat-sheet/. Accessed 10 April 2022.
- Shields, Carol L., and Hakan Demirci. “Clinical factors in the identification of small choroidal melanoma.” PubMed, June 2004, https://pubmed.ncbi.nlm.nih.gov/15327099/. Accessed 10 April 2022.
- Shields, Carol L., et al. “Combination of clinical factors predictive of growth of small choroidal melanocytic tumors.” Arch Ophthalmol ., vol. 118, no. 3, 2000, pp. 360-364.
- Shields CL, Cater J, Shields JA, et al. Combined plaque radiotherapy and transpupillary thermotherapy for choroidal melanoma: tumor control and treatment complications in 270 consecutive patients. Arch Ophthalmol 2002;120:933–940.
- Say, E. T., et al. “Plaque Radiotherapy for Management of Small Choroidal Melanoma: A Series of 1251 Cases.” Investigative Ophthalmology and Visual Sciences, vol. Volume 51, no. Issue 13, 2010.
- Moss, Cathy. “New Clinical Trial for Early-Stage Eye Melanoma.” Wills Eye Hospital, 24 April 2017, https://www.willseye.org/new-clinical-trial-early-stage-eye-melanoma/. Accessed 10 April 2022.
- Ko, Paula. “Ocular Tumors: Choroidal Nevus Vs. Choroidal Melanoma.” The Women's Journal, 1 October 2017, https://thewomensjournal.com/ocular-tumors-choroidal-nevus-vs-choroidal-melanoma/. Accessed 10 April 2022.
- The Collaborative Ocular Melanoma Study Group. Assessment of Metastatic Disease Status at Death in 435 Patients With Large Choroidal Melanoma in the Collaborative Ocular Melanoma Study (COMS): COMS Report No. 15. Arch Ophthalmol. 2001;119(5):670–676. doi:10.1001/archopht.119.5.670.