Background
As ophthalmologists, it is easy to focus solely on ocular-based pathology—however, to best care for our patients, a comprehensive diagnosis and treatment approach is necessary. We are well aware that systemic disease can manifest in the eyes—
diabetic retinopathy and hypertensive retinopathy, iritis secondary to
autoimmune disease, HIV retinopathy—however, systemic neoplastic ocular metastasis, though not as common, is an immensely important entity to understand, identify, treat, and refer to the proper subspecialist. The ophthalmologist may be the first to identify a uveal mass, which may indeed signify metastasis.
This article will review the essential diagnosis and treatment of choroidal metastasis and important takeaways to better treat your patients.
Overiew of choroidal metastasis
The uvea is the most common site of metastasis from primary cancer elsewhere in the body, with the choroid being the largest receiving site at 88% (followed by metastasis to the iris (9%) and ciliary body (2%).
1-4 The choroid is thought to be a favored spot due to its rich blood supply.
1-4 Some common primary cancers that can be seen as metastatic to the choroid include lung, gastrointestinal (GI) tract, kidney, and
breast.
1-4 Melanoma is also known to metastasize to the choroid, as well as the prostate, thyroid, and pancreas.
1-4In a study by Shields et al., which reviewed 2,214 uveal metastases from 1,111 patients, the majority of which were Caucasian females, most patients had unilateral metastasis at the time of diagnosis (82%), and the primary tumor site was known prior to ocular diagnosis (67%).1 In this demographic, the most common primary tumor site was the breast (37%), followed by lung (26%), kidney (4%), GI tract (4%), cutaneous melanoma (2%), prostate (2%), lung carcinoid (2%), thyroid (1%), pancreas (1%), other sites (3%), and unknown (16%).1
Mean age at the time of metastasis was between 57-66 years.1 Mean number of metastases per eye was between 1-2.1 In addition; mean survival was poor; the worst survival was found in those with pancreatic metastasis (mean 4.2 months), while the best survival (92% at 5 years) were those patients with lung carcinoid.1
What to look for
Patient history is always an essential part of the ophthalmic exam. Patients who have a history of cancer diagnosis should always undergo complete and comprehensive retinal exams to detect possible signs of metastasis and paraneoplastic disease. These patients may or may not have ocular complaints (though they may present with complaints of blurry vision, flashes, floaters, and pain); therefore it is up to the treating ophthalmologist to identify, as best as they can, any evidence of irregularities that could relate to the patients’ oncological diagnosis.3,4
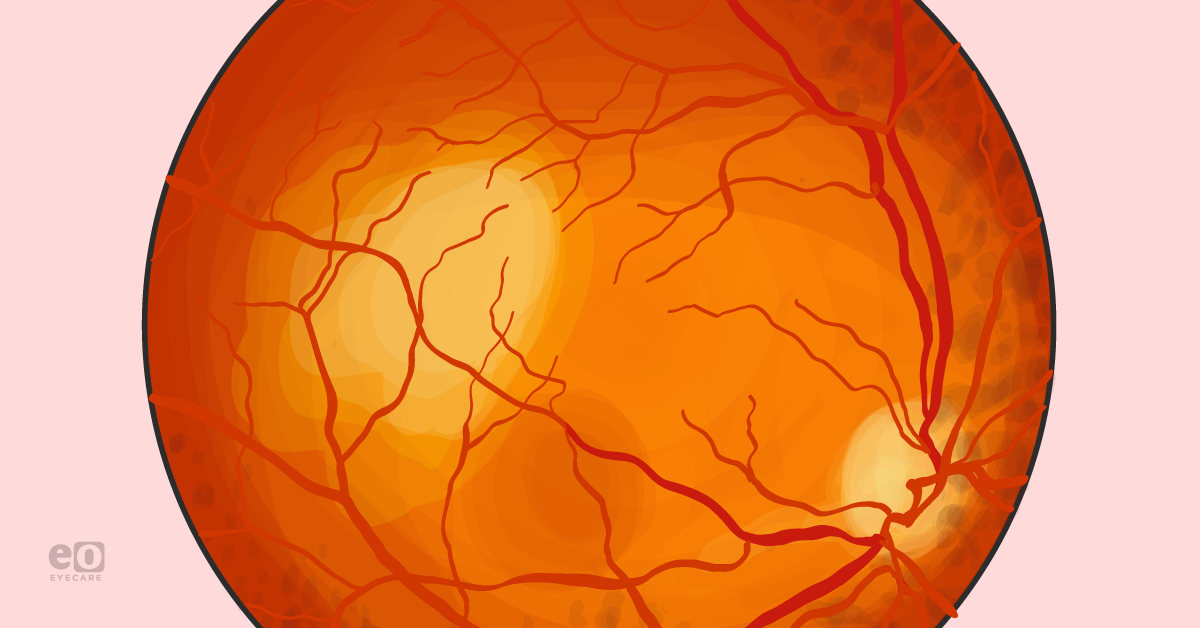
Choroidal metastasis most commonly appears as a solitary yellow mass with associated subretinal fluid.1-4 In addition, tumors arising from the GI tract or kidney may be substantially thicker than those from the breast or cutaneous melanoma (4mm vs. 1-2mm).1-4 It is important to note that choroidal metastasis, though most commonly yellow, may be orange, amelanotic, or darkly pigmented.3,4 Ultrasound may help in diagnosis as the internal reflectivity in choroidal metastatic lesions is variable compared to that of uveal melanoma, which usually has low internal reflectivity.3,4
Diagnostic modalities for choroidal metastasis
Several diagnostic modalities complement a comprehensive retinal exam when diagnosing and assessing choroidal metastatic lesions.
Fluorescein Angiography (FA): This test can permit differentiation from choroidal metastases and choroidal melanoma. Here,
fluorescein angiography may show a hypofluorescent pattern in early arterial phases, with hypofluorescence of later venous phases. Choroidal metastatic lesions may also have dilated retinal capillaries with leakage of the tumor border.
1-4 Indocynine green angiography (ICG): This modality is similar to FA in the procedure; however, it is more specific to the choroid and, therefore, may highlight choroidal lesions better. Here, a metastatic lesion may show a blockage of background staining with patchy staining of the tumor surface.1-4
Optical Coherence Tomography (OCT): This imaging modality can demonstrate preretinal, intraretinal, and subretinal disturbances as well as fluid collections in the posterior segment. In addition, a pattern of hyperintense irregular spots in the photoreceptor layer and retinal pigment epithelium (RPE).
3,4 The choroidal surface may appear ‘bumpy’ and show compression of the choriocapillaris.
3,4 OCT may also be used to follow the progression of lesion size and also intraretinal and subretinal fluid accumulations.
Fundus Autofluorescence (FAF): FAF is a noninvasive imaging technique that allows assessment of intrinsic autofluorescence of ocular tissues secondary to lipofuscin.
3,4 On exam, choroidal metastasis may have overlying subretinal fluid and lipofuscin, lending to a hypofluorescence of the tumor on
fundus autofluorescence.
3,4 However, there is contrasting hyperfluorescence of the associated lipofuscin, and subretinal fluid—these features may help delineate tumor margins and allow for assessment of progression.
3,4 A-scan ultrasound: Ophthalmic ultrasound (A-Scan and B-Scan) can determine tumor size, echogenicity, and even differentiation of choroidal metastasis from other lesions.3,4 A-Scan can demonstrate moderate to high internal reflectivity of the metastatic lesion vs. a melanoma, which typically displays low-medium internal reflectivity.3,4
B-scan ultrasound: B-Scan ultrasound can identify a choroidal mass, as well as secondary retinal detachment and subretinal fluid accumulation.3,4 Color flow mapping, if available, may show hypervascularity with a peripheral blood flow pattern.3,4
MRI: In some cases, MRI may help delineate the extent of tumor metastasis. Here, a well-delineated choroidal mass may appear isointense in T1-weighted images and hypointense in T2 images.3,4
Fine needle aspiration biopsy (FNAB): In cases of an unknown primary tumor or indeterminate diagnosis, FNAB can provide a pathological/cytology-based diagnosis.3-5 This procedure is best done by an ocular oncologist with extensive training in this procedure to avoid accidental retinal injury or injury to other intraocular structures.3-5
Treatments
Control of uveal metastasis may be managed via local and systemic therapies (alone or in combination). This is where a team-based approach is best; communication between the treating ophthalmologist, primary care doctor, and medical/radiation oncologist is essential to best treat these patients.
Below is an overview of local ophthalmic treatment modalities.
Please bear in mind, the best treatment, depending on tumor type, may be systemic chemotherapy and hormonal therapy. PET CT Scan may be warranted to highlight and document the extent of metastatic disease, which may also influence therapy.
Systemic therapy: Chemotherapy, immunotherapy or hormone therapy may be preferred in patients with multifocal and bilateral choroidal metastases. The choice of therapy depends on the primary tumor and is best designated by the treating oncologist. The fenestrated endothelium permits efficacy of systemic chemotherapy in the eye in the choriocapillaris, which allows entry of medications into the choroidal lesions for effective tumor control.3,5
Plaque radiotherapy: This treatment is usually reserved for solitary metastatic lesions; it offers precise and controlled radiation dosage to the eye.1,3,4,6 In addition, it may only require 3-4 days of treatment compared to external beam therapy (EBRT), which may require 3-4 weeks.3,4,6 Creation of a treatment plan for plaque-based therapy is usually based on metastatic lesion size and thickness and the distance from the lesion to the optic nerve and macula.3,4,6 Plaque therapy, though very precise, can cause adverse effects such as radiation retinopathy, radiation optic neuropathy, and cataract formation.3,4,6
Transpupillary Thermotherapy (TTT): TTT uses a diode laser to administer heat to the choroid and RPE through a dilated pupil. TTT can induce tumor necrosis.3,4
External beam radiation: This modality is useful for multifocal disease and has been shown to decrease the subretinal fluid/exudative retinal detachment that may be associated with metastatic choroidal disease.3,4,6 The typical dosage is 40-60 Gy.3,4,6
Gamma Knife Radiosurgery (GKR): GKR has been used to treat choroidal metastases. Here, multiple gamma rays with an average dosage of 30 Gy are focused on the lesion over a period of 10 days.3,4
Proton Beam Radiotherapy (PBT): In comparison to GKR, PBT allows for more focused radiation.3,4 Typical dosage is 28 Gy over two treatments.3,4 Possible complications of PBT include eyelid burns, iris neovascularization and neovascular glaucoma, radiation maculopathy and optic neuropathy, cataract, and madarosis.3,4
Photodynamic Therapy (PDT): PDT produces reactive oxygen species and intravascular thrombosis and tumor infarction through verteporfin.3,4 PDT can treat small metastatic lesions and may also improve vision in those eyes with associated subretinal fluid.3,4
Intravitreal antivascular endothelial growth factor (Anti-VEGF) injection: These injections help treat choroidal metastases based on their ability to cause regression of neovascularization.3,4 As tumors are dependent on neovascularization for growth, use if anti-VEGF injections such as bevacizumab and ranibizumab can be effective treatments for these lesions.3,4 Injections are typically given every 1-3 months, depending on tumor response.3,4 Duration of treatment may depend on patient response and tolerance.
Enucleation: In the very worst-case scenario, where all other treatment modalities have been trialed without success, and it has been determined that the eye cannot be salvaged or is blind and painful, the patient and treating ophthalmologist may consider enucleation.3,4
Conclusions
Unfortunately, the eyes are not immune from systemic cancer metastasis. Once an irregular mass has been detected on exam, it is imperative to investigate further and determine its malignant potential and systemic impact. OCT,
angiography, and fundus photography are necessary diagnostic technologies that can help confirm the diagnosis and help follow therapeutic response.
It is always best to refer to a
retina specialist for these diagnostics if unfamiliar or uncomfortable with their interpretation. Ultimately, the patient may need to see an ocular oncologist for treatment and follow-up.
In addition, a team-based approach, with clear communication between the patient, oncologist, and primary care doctor, is an invaluable part of the treatment plan.
References
- Shields CL, Shields JA, et al. Uveal Metastasis: Clinical Features and Survival Outcome of 2214 Tumors in 1111 Patients Based on Primary Tumor Origin. Middle East Afri J Ophthalmol. 2018; 25(2): 81-90
- Shields CL, Shields JA, Gross N, Schwartz G, Lally S. Survey of 520 eyes with uveal metastases. Ophthalmology. 1997;104: 1265-1276
- BCSC Section 4: Ophthalmic Pathology and Intraocular Tumors. Chapter 20. 2010-2011
- Arepalli S, Kaliki S, Shields CL. Choroidal Metastases: Origin, features and therapy. Indian J Ophthalmol. 2015; 63(2): 122-127
- Shields JA, Shields CL, Ehya H, Eagle RC, De Potter P. Fine-needle aspiration biopsy of suspected intraocular tumors. The 1992 Urwick Lecture. Ophthalmology. 1993;100(11): 1677-1684
- De Potter P, Shields CL, Shields JA, Cater JR, Brady LW. Plaque radiotherapy for juxtapapillary choroidal melanoma. Visual acuity and survival outcome. Arch Ophthalmol. 1996; 114(11): 1357-1365