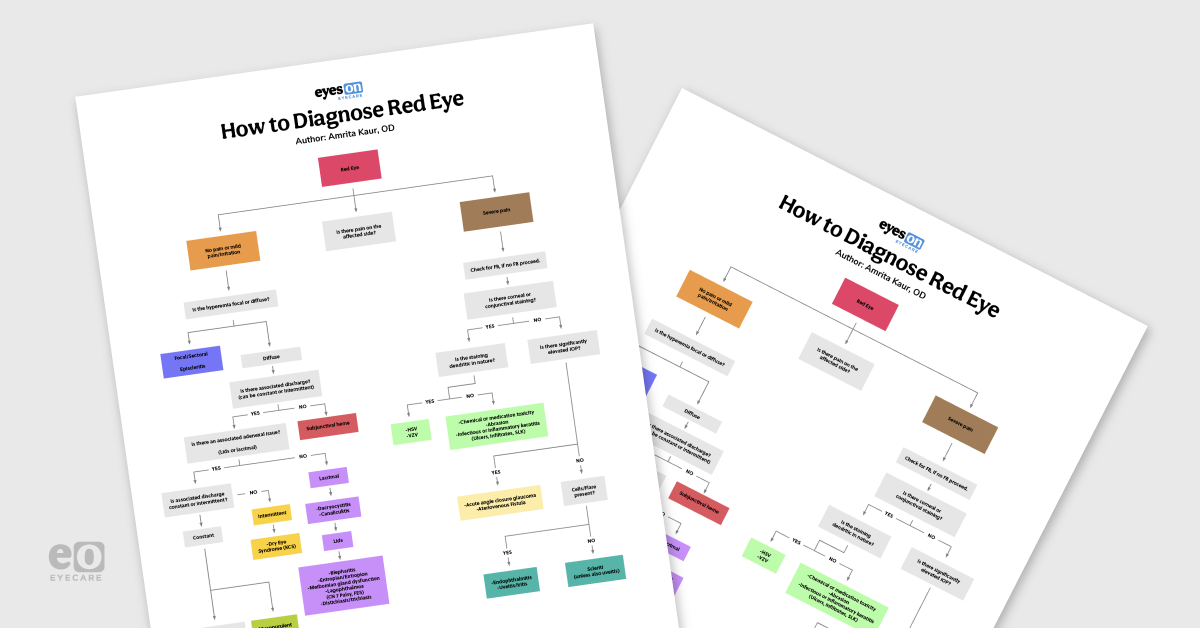
Red eye, or hyperemia as we refer to it in the ophthalmic world, can be the result of what seems like infinite conditions. Although it is one of the most common findings we encounter in practice, deciphering the cause is often difficult. This flowchart and article serve to help narrow differentials for
common causes of red eye. Additionally, the information provided should help guide the practitioner in differentiating a vision-threatening diagnosis from a less severe condition.
1,2First question: Pain or no pain?
In an attempt to diagnose the cause of a patient’s red eye, the first triage question that should be asked is if the affected eye or eyes are in pain.
If there is no pain or only limited pain, we next observe if the hyperemic area is a focal redness or if it is a diffuse hyperemia. If sectoral or focal, this is most likely episcleritis. Episcleritis typically either has no or only minimal pain, compared to the severe pain from scleritis. Aside from the pain factor, a common way to help differentiate the two conditions is to instill a drop of phenylephrine into the affected eye. The hyperemia will typically resolve (blanch) after 10-15 minutes after drop instillation in the case of episcleritis, but not
scleritis.
2Second question: discharge?
If the redness is diffuse but there is no associated discharge, it is likely a subconjunctival hemorrhage. Ask these patients about blood thinners or if they recently performed any strenuous or valsalva inducing activities.2 Checking blood pressure in-office is also crucial in order to rule out latent hypertension in patients with subconjunctival hemorrhages. Episcleritis and subconjunctival hemes both typically self resolve, but if they do not or are recurrent, further workup to assess the underlying cause is required.2
If the diffusely hyperemic eye presents with any form of discharge, determine if there are any associated adnexal issues with the lids or lacrimal system. If there is mucopurulent discharge, medial canthal inflammation, or epiphora on the ipsilateral side of the red eye, consider canaliculitis or dacryocystitis. Canaliculitis often presents with a red and “pouting” punctum and is caused by infection of the canaliculus.3,4 Dacryocystitis is an infection of the lacrimal sac with similar but more pronounced symptoms, such as more significant swelling and pain.
Antibiotics are often used to treat both conditions, but dacryocystitis is the more severe condition and often needs a referral for imaging or a surgical approach for treatment.4-6
The lids are another source of a diffusely hyperemic eye with potential discharge. Upon examination in these patients, explore the possibilities of lagophthalmos, blepharitis, entropion/ectropion,
meibomian gland dysfunction, or distichiasis/trichiasis.
4-7Note that lagophthalmos can be due to myriad causes such as floppy eyelid syndrome (FES), facial nerve (CN 7) palsy, neurological disease, or trauma to name a few. These patients struggle with complete lid closure on the affected side, thus may have corneal exposure; the corneal exposure causes the hyperemia secondary to issues such as dry eyes, exposure keratopathy, and even corneal ulcers.7
Blepharitis and meibomian gland dysfunction can be managed with lid hygiene, warm compresses, antibiotics or anti-inflammatory therapy, and intermittent dry eye therapy if needed.4, 5 Several conditions induce ocular redness by causing the lashes to irritate the surface of the eye, such as trichiasis, distichiasis, and entropion. Often underlying blepharitis needs to be treated in these conditions.
Antibiotics and epilation often aid the patient, but occasionally surgical intervention is required for relief.4,6 Ectropion results in corneal exposure and needs to be treated if it causes exposure keratopathy. Many patients with ectropion are intermittently managed with lid taping and combination topical treatment, but ultimately also require surgery for relief.4
If a patient exhibits discharge in the affected red eye but appears to have no adnexal issues, assess the frequency and quality of the discharge. If the discharge is infrequent or the patient complains of epiphora, transient pain, and foreign body sensation but has no signs of allergic conjunctivitis, consider
dry eye syndrome (DES) or keratoconjunctivitis sicca (KCS).
As we know, there are a plethora of causes and treatment for KCS, many of which overlap with conditions already discussed. Do not overlook that DES may stem from underlying lid issues from inflammation or exposure keratitis. If there does not appear to be any associated lid issue to resolve, consider treatment with cyclosporine, omega 3’S,
artificial tears, and humidifiers as a start.
4,6When the discharge in the affected eye presents in a more constant fashion, go on to assess the quality of the discharge. If the discharge is mucopurulent in nature, the red eye or eyes are likely the result of a type of bacterial conjunctivitis. Bacterial conjunctivitis is typically mild in nature, but given that there are so many forms, it has some potential to be hyperacute with severe symptoms (such as the case with gonococcal conjunctivitis). Often patients with bacterial conjunctivitis will complain of a crusting on their eyelids/lashes with their eyes matted shut upon awakening.2,4,8
We are unable to delve into all the forms and causes of bacterial conjunctivitis in this space, but recognize that the most common causes of bacterial conjunctivitis in the adult population are S aureus and H influenza, while the most common causes in children are H influenza and S pneumonia, and the most common cause for neonatal conjunctivitis is chlamydia trachomatis.8 Chlamydial inclusion conjunctivitis is typically sexually transmitted in young adults, and it is infected mothers who can pass it along to neonates. Trachomatous conjunctivitis primarily occurs in developing countries with poor sanitary measures.4
Generally, gonococcal and chlamydial conjunctivitis are treated with systemic antibiotics while bacterial conjunctivitis from the majority of other organisms may be treated with topical antibiotic therapy.8
When the red eye presents with a more serous or watery discharge, consider a viral or allergic conjunctivitis. Allergic conjunctivitis is typically bilateral and associated with other symptoms of allergy, such as sneezing or sinus congestion. The affected eyes often present with a papillary reaction, and the patient will have no inflammation of the preauricular lymph node. This can be treated with an oral or topical antihistamine. Viral conjunctivitis, on the other hand, does often have a positive pre-auricular lymph node inflammation. Generally, viral conjunctivitis is self limiting and mild but on occasion can be painful and severe with the development of subepithelial infiltrates, in which case topical steroid treatment may be required.4
Next question: pressure?
Moving on to diagnoses of red eyes with constant severe pain, first consider checking for a foreign body in the eye if the patient has a history of any kind of recent ocular trauma or foreign body sensation. It is also important to evert the superior lids when checking for an ocular foreign body, especially if tracking marks are seen on the cornea. If there is no foreign body present, we can next assess the cornea and conjunctiva for any fluorescein staining. When no staining or abrasions appear to be present, check the patient’s intraocular pressure.
If the patient has a markedly elevated intraocular pressure (IOP), typically with an evidently narrow or closed anatomical angle, they are likely experiencing an
acute angle closure glaucoma attack. These patients are typically in severe pain, and the globe feels firm when palpated. The pupil may be mid-dilated or poorly reactive to light, and the patient may complain of halos around lights and blurry/hazy vision.
4,5Treatment depends on the etiology of the angle closure. These patients may ultimately need a surgical referral but, in office, we should attempt to lower the IOP with topical or oral therapy ASAP.4
Although a less commonly found cause of elevated IOP with red eye, an arteriovenous fistula cannot be a forgotten cause. These patients may present with a pulsatile proptosis, have a “corkscrew” appearance to the conjunctival vessels and even retinal venous congestion. If suspected, these patients need prompt referral for imaging and treatment.4
If the hypermic eye is inducing severe pain but has a normal IOP, check for cells and flare in the anterior chamber. If there is no anterior chamber reaction present, consider scleritis (although sometimes uveitis is associated with scleritis). Scleritis presents with severe pain that can radiate to the orbital area and may present with pain on eye movement and decreased vision. These patients are initially managed with NSAID and steroid therapy. However, once symptoms are treated, these patients need a workup for systemic disease and treated for any positive findings for long-term management.4, 9
When cells and flare are present in a painful hypermic eye, consider uveitis or endophthalmitis. As we know, there are seemingly infinite causes of both uveitis and endophthalmitis from systemic inflammatory disease to iatrogenic causes. At times, these conditions may be difficult to discern from each other. In these cases, a thorough history, complete workup, extensive ancillary testing, and often referral are required for appropriate management.4,10 It is also important to perform a thorough dilated ocular health assessment for any patient with iritis/uveitis.
Should fluorescein staining be present in the red eye, we want to appraise the cornea for any kind of dendritic appearance. If the cornea appears to have true dendritic ulcers, the cause is Herpes Simplex Virus (HSV). These dendrites have terminal end bulbs and are typically bilateral in presentation, as opposed to pseudodendrites from the Varicella Zoster Virus (VZV). Psuedodendrites will always be unilateral, and do not present with terminal end bulbs. VZV resides latently in the dermatomes of one side of the body; if pseudodendrites are present, it has been reactivated in the ophthalmic division of the trigeminal nerve. Both conditions may have associated skin vesicles and are treated with antiviral therapy.11,12
Fluorescein staining in the red eye that is not consistent with a dendritic appearance may be from a plethora of causes. Common causes include infectious or inflammatory keratitis (including contact lens related pathology such as ulcers), abrasions of the cornea or conjunctiva, chemical burns, inflamed pinguecula, and topical ophthalmic drug toxicity.
4 Remember key distinctions
Despite the plethora of causes for red eye(s) that present for evaluation, hopefully this guide will facilitate clinical thinking when attempting to diagnose and treat these patients. By remembering a few key distinctions between the etiologies of red eye, clinicians can quickly arrive at a diagnosis and treatment plan for their patient.
Download the flowchart now!
Download the Red Eye Flowchart!
This colorful and comprehensive flowchart is 100% free!
Citations
- Vaishnavi Menon, Varshini Manoharan. Decoding the Red Eye. Eye News. Feb 2021.
- Gilani c, et al. Differentiating Urgent and Emergent Causes of Acute Red Eye for the Emergency Physician. West J Emerg Med. 2017 Apr; 18(3): 509–517. Published online 2017 Mar 3. doi: 10.5811/westjem.2016.12.31798.
- Freedman JR, Markert MS, Cohen AJ. Primary and secondary lacrimal canaliculitis: a review of literature. Surv Ophthalmol. 2011 Jul-Aug;56(4):336-47. doi: 10.1016/j.survophthal.2010.12.001. Epub 2011 May 28. PMID: 21620429.
- Gerstenblith AT, Rabinowitz MP. The Wills Eye Manual. 6th ed. Philadelphia, PA; Lippincott Williams and Wilkins; 2012: 4; 59-60;110-125;139-146; 213-217; 358-393.
- CRONAU H, et al. Diagnosis of Red Eye and Management in Primary Care. Am Fam Physician. 2010 Jan 15;81(2):137-144.
- Santhakumaran, S. Approach to Red Eye. 2021 Mar: 1McGill University, Montreal, QC, Canada. DOI: 10.26443/mjm.v19i1.196.
- Fu L, Patel BC. Lagophthalmos. [Updated 2021 Jul 30]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-.
- Tarabishy AB, Jeng BH. Bacterial conjunctivitis: a review for internists. Cleve Clin J Med. 2008 Jul;75(7):507-12. doi: 10.3949/ccjm.75.7.507. PMID: 18646586.
- Sainz de la Maza M, Foster CS, Jabbur NS. Scleritis-associated uveitis. Ophthalmology. 1997 Jan;104(1):58-63. doi: 10.1016/s0161-6420(97)30361-3. PMID: 9022105.
- Davis JL. Diagnostic dilemmas in retinitis and endophthalmitis.Eye (Lond). 2012;26(2):194-201. doi:10.1038/eye.2011.299.
- Shaikh S, Ta CN. Evaluation and management of herpes zoster ophthalmicus. Am Fam Physician. 2002 Nov 1;66(9):1723-30. PMID: 12449270.
- Azher TN, Yin XT, Tajfirouz D, Huang AJ, Stuart PM. Herpes simplex keratitis: challenges in diagnosis and clinical management. Clin Ophthalmol. 2017;11:185-191. Published 2017 Jan 19. doi:10.2147/OPTH.S80475.