Entropion can be defined as the inward movement of the eyelid margin; this most often occurs from eyelid laxity.
When the eyelid turns inward, the lashes, lid, and eyelid margin rub against the ocular surface, causing ocular irritation.
Overview of entropion
Presenting symptoms of entropion include foreign body sensation, tearing, red eye, and irritation.1 Other symptoms that may also be present include photophobia, blurry vision, and burning eye sensation.2
Progressive age-related changes can lead to loss of adequate tone and laxity, which are structural changes characteristic of entropion. Its prevalence increases with age and is more common in women.2,3 Unilateral occurrence of entropion is less likely than bilateral presentation.2,3
Associated findings and conditions include increased lateral or medial canthal tendon laxity, overriding preseptal orbicularis, dry eye, enophthalmos, chronic blepharitis, superficial punctate keratopathy, and chronic conjunctivitis.3,4
Figure 1 illustrates entropion of the lower eyelid.
Figure 1: Courtesy of Leonid Skorin, Jr., DO, OD, MS.
Differential diagnoses for entropion
The development of entropion can occur from involutional, cicatricial, spastic, or congenital etiologies. Differential diagnoses like epiblepharon, ectropion, distichiasis, and trichiasis must be ruled out before entropion can be confirmed.1 The eyelashes face the globe in epiblepharon due to an additional horizontal skin fold that overrides the lower lid margin.1,2,5
The appearance and symptoms of epiblepharon are very similar to entropion, but there is no actual in-turning of the eyelid margin.5 If the lid margin is pulled downward and eyelashes revert to usual positioning, epiblepharon can be ruled out.1,2
“Ectropion can be distinguished by its outward eyelid movement, despite similar symptoms to entropion.”
Distichiasis occurs when there is inappropriate lash growth from the meibomian glands.2,6 With trichiasis, the lashes originate from their normal position but grow posteriorly and make contact with the conjunctiva and cornea.6 Symptoms like foreign body sensation, redness, and irritation are present with the aforementioned differential diagnoses, but physical examination is necessary to diagnose entropion.
Types of entropion
There are four primary types of entropion: involutional, spastic, congenital, and cicatricial.
Involutional entropion
Involutional entropion is the most common form of entropion and appears in advancing age, especially in patients who are 60 years and older.4 It exists in 2.1% of the elderly population.1
Age-related changes most commonly leading to the development of involutional entropion include horizontal lower eyelid laxity, disinsertion or attenuation of the eyelid retractor muscles and capsulopalpebral fascia, and vertical eyelid instability resulting from overriding of the preseptal orbicularis muscle.4
Spastic entropion can occur secondary to a chronically occurring involutional entropion.
Figure 2 shows entropion of the lower eyelid with overriding of the preseptal orbicularis muscle.
Figure 2: Courtesy of Leonid Skorin, Jr., DO, OD, MS.
Spastic entropion
Spastic entropion development involves the orbicularis oculi muscle. The Riolan muscle, part of the orbicularis oculi muscle, acts as an eyelid retractor and keeps the eyelid and globe firmly juxtaposed.1
Trauma, inflammation, chronic irritation, or surgery to the eye can lead to eyelid edema.5 The presence of edema can cause the Riolan muscle to spasm. When this muscle spasms, the development of spastic entropion can occur.
Figure 3 is a clinical image of a patient with spastic entropion of the lower eyelid.
Figure 3: Courtesy of Leonid Skorin, Jr., DO, OD, MS.
Congenital entropion
Congenital entropion is caused by abnormal eyelid development. It is a condition that appears prior to 6 months of life. With less than 50 cases reported worldwide, congenital entropion is rare.1 Short posterior lamella, eyelid retractor dysgenesis, or defects in tarsal plate structure influence the development of congenital entropion.1,5
Cicatricial entropion
Cicatricial entropion can develop secondary to a history or presence of infections, such as trachoma, inflammatory diseases such as Stevens-Johnson syndrome, chemical and thermal burn, autoimmune diseases such as ocular cicatricial pemphigoid, and other eye conditions.1,4
Additionally, long-term use of glaucoma medications such as miotics has been known to cause cicatricial entropion.4,5 The posterior lamella vertically contracts from eyelid scarring, which leads to cicatricial development.4
How to evaluate patients for entropion
Entropion can be identified on external and biomicroscopy evaluation. When the eyelid is chronically turned inward, visualization of entropion is apparent. With mild or intermittent entropion, the eyelid may not appear affected on casual observation.
Physical examinations to assess inverted eyelid margins include:
- Snap-back test
- Eyelid distraction test
- Digital eversion test
- Orbicularis override test
In order to evaluate horizontal eyelid laxity in entropion, the patient is asked to look up slightly, and the lower eyelid is pulled inferiorly and then released (snap-back test). If the eyelid does not return to its position apposed to the globe in 1 to 2 seconds, there is pathological laxity.1 If blinking causes the eyelid to return to the globe after an initial delay, moderate entropion is present. When blinking does not return the eyelid to its normal position against the globe, there is severe entropion.7
Eyelid laxity can also be assessed by the eyelid dislocation or distraction test. The lower eyelid is moved anteriorly so that the lower lid margin to globe distance can be measured. There is no pathological laxity when the distance is 2 to 3mm, but as the distance increases, 10mm or greater, severe laxity and entropion is present (Figure 4).1
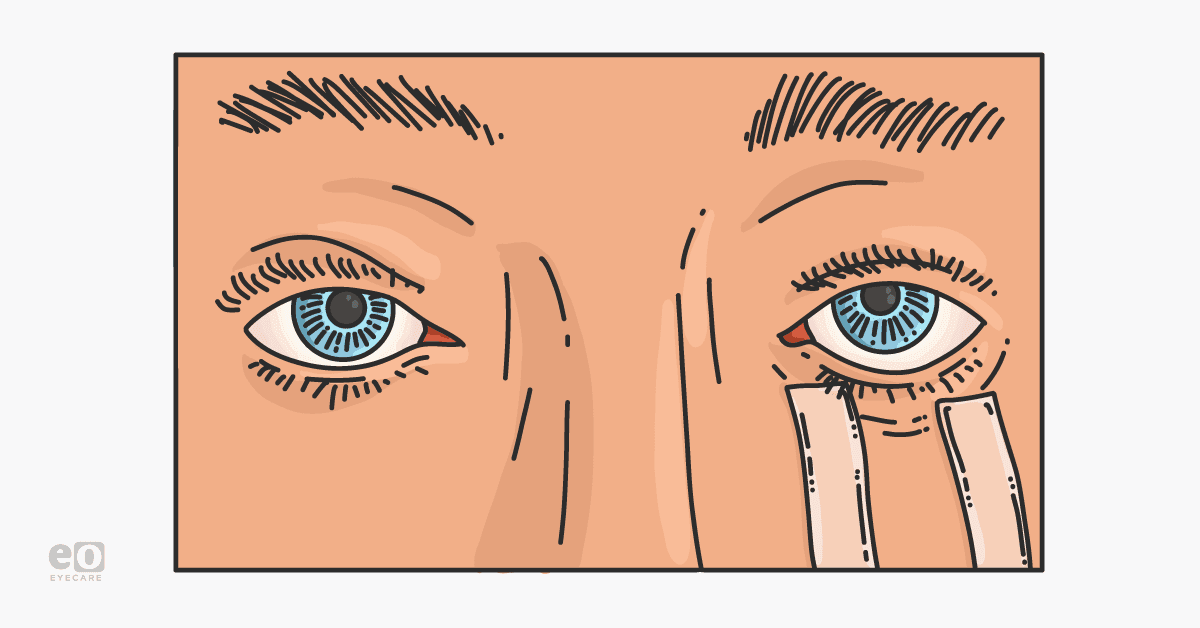
Figure 4 demonstrates the distraction test, which involves measuring the amount of displacement of lower eyelid from the globe with a millimeter ruler.
Figure 4: Courtesy of Leonid Skorin, Jr., DO, OD, MS.
The digital eversion test can differentiate the presence of either involutional or cicatricial entropion.8 The lower eyelid is pulled downward in the absence of blinking. A vertical reorientation of the lid margin against the globe is indicative of involutional entropion.1 If the eyelid remains inverted, this indicates an underlying cicatricial component.8
Another physical exam to determine entropion is the orbicularis override test. Upon squeezing the eyes shut and blinking, any misalignment or unusual motion of the preseptal orbicularis muscle can cause the lid to rotate inward.1,4 A positive finding in this test suggests severe entropion.
Surgical and non-surgical treatments for entropion
Prompt management of entropion can prevent corneal damage and help to reduce vision loss. Treatment includes non-surgical and surgical management. When a patient is not a candidate for surgery, or needs symptom relief, non-surgical treatment can provide immediate effects.
Non-surgical management of entropion
Topical lubricating gels and ointments with or without bandage contact lenses can ease irritation and pain by limiting lid margin contact against the eye. Another technique is epilation, where epilating forceps are used to remove any in-turned lashes that are in contact with the corneal surface.1
“Taping can also be used to position the lid margin so that eyelashes are not in contact with the cornea.”
Botulinum toxin (i.e., Botox, Abbvie) injections into the orbicularis oculi muscle will temporarily inhibit acetylcholine release at the neuromuscular junction. This weakens the protractor action of the orbicularis oculi muscle, preventing the inversion of the eyelid.5 Maximum effect occurs after 1 week and can provide 3 to 4 months of relief.1
Entropion will reoccur as the medication wears off; therefore, repeat injections are needed. Surgical repair is the only treatment that offers long-term results. With 50 to 80% success rates, entropion surgery is an effective and more definitive therapy.1
Surgical management of entropion
Surgery includes the reattachment of the inferior eyelid retractors or capsulopalpebral fascia to the tarsal plate (seen in Figure 5).8 Once reattachment is complete, a lateral canthal strengthening procedure is performed to resolve any horizontal lid laxity.
There are other surgical methods for treating entropion, including the placement of everting or "temporizing" sutures.3,8 These sutures can be placed in an outpatient/in-office procedure room, potentially avoiding a trip to the operating room.
Figure 5 illustrates localizing the inferior eyelid retractors or capsulopalpebral fascia prior to reattachment to the inferior edge of the tarsal plate.
Figure 5: Courtesy of Leonid Skorin, Jr., DO, OD, MS.
Ultimately, surgery offers a better chance for long-term treatment of entropion. For elderly patients and those with complex medical issues, medical management should be considered prior to surgical intervention.