In recent years, the
glaucoma treatment paradigm has shifted to focus on earlier interventional treatment. Traditional options for treatment of primary open angle glaucoma (POAG) and/or ocular hypertension (OHTN) include argon laser trabeculoplasty (ALT),
long-term eye drops, and surgical trabeculectomy or tube shunts.
The burden of treatment with eye drops can drive down adherence to treatment and result in progression of the disease process, ultimately leading to permanent vision loss. Topical eye drops carry significant risk for developing ocular surface disease due to drop toxicity
1 and, in severe cases,
neurotrophic keratitis.
2 Therefore, it falls upon optometrists to identify appropriate candidates early or non-drop option treatments to reduce the burden of treatment, and thereby reduce progression of disease and the need for filtering surgery.
With an increasing focus on interventional treatment for glaucoma, we now have non-drop options including Selective Laser Trabeculoplasty (SLT),
Minimally Invasive Glaucoma Surgery (MIGS), with or without cataract extraction, and sustained release implants of varying modalities.
In this article, we will review where SLT fits into the treatment paradigm for POAG and OHTN and whether it is appropriate as a first-line treatment.
Who is a candidate for SLT?
Candidates for SLT include those with:
- Ocular surface disease
- Preservative sensitivities
- Drop intolerance
- Reduced memory or cognitive abilities
- Limited dexterity (i.e., arthritis)
- Patients in transitional housing
- Limited accessibility to medications, such as in cases with lack of insurance or limited funds
- Non-adherence to follow ups and drop regimens
- Patients who are on monotherapy and require adjunctive therapy
- Drop-averse patients who simply do not wish to use drops if their lifestyle does not support it (i.e., patients who travel)
Selective laser trabeculoplasty (SLT) has been shown to be most effective in young patients with ocular hypertension or early POAG and high IOPs3 and open, pigmented angle structures.3,4
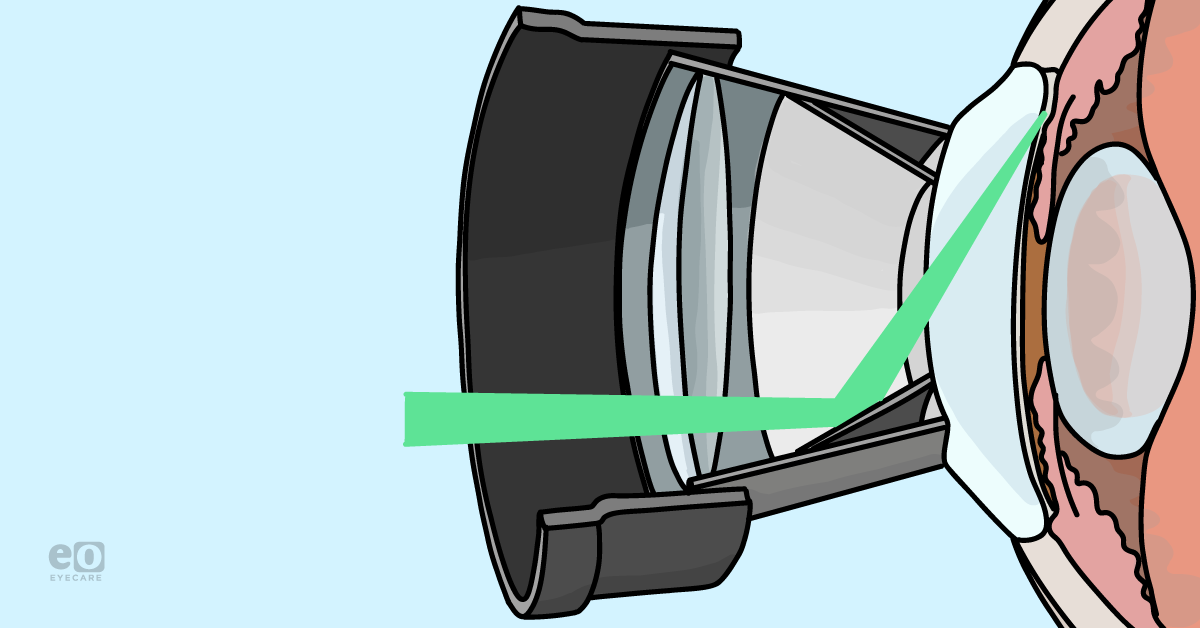
How does SLT work?
The multifactorial mechanism of action of SLT includes a contraction of trabecular meshwork fibers (while avoiding coagulative damage to surrounding tissues),4 stimulation of trabecular meshwork cell proliferation, and extracellular matrix remodeling through the pro-inflammatory pathway.5. It is delivered using a low energy, short pulse laser.
SLT differs from ALT in the laser settings and repeatability. With SLT, the energy is absorbed best by pigmented cells in the trabecular meshwork and does not seem to cause permanent damage to the trabecular meshwork fibers. Therefore, it can be repeated as many times as needed.4
How much IOP lowering should we expect with one round of SLT?
We can expect a 26-29% drop in IOP after one 360 degree SLT treatment, which is comparable to the standard first-line topical treatment with a prostaglandin analog.3
Laser as first line of therapy
The Glaucoma Laser Trial (GLT) first demonstrated the efficacy of laser directly applied to the trabecular meshwork with ALT as compared with topical timolol 0.5% in treatment naïve eyes newly diagnosed with POAG. ALT was shown to be efficacious for 2 years in maintaining a lower IOP, requiring less than 2 drop therapies for IOP control and demonstrating less
visual field loss. After 2 years, the hypotensive effects diminished and patients needed drop therapy. The limitation with ALT is that it cannot be repeated, thereby limiting its application as a first-line therapy.
6,7A major landmark study known as the LiGHT trial was published in 2019, showing benefit to a very large cohort of 718 POAG and OHTN subjects who received SLT as a first line of therapy for OHTN or mild/moderate POAG. Primary and secondary outcomes included
health-related quality of life (HRQL), clinical effectiveness, safety, and cost compared to topical medications.
While HRQL remained comparable between both groups, IOP was better controlled over a 3 year period with SLT as first-line therapy as compared to eye drop therapy and the cost burden was less. After 12 months of receiving one SLT treatment, 75% were drop free; 58% after 3 years, which is still over half. This data demonstrates that even for a patient who is non-compliant with follow ups for 3 years, one out of two of these patients will still be drop free and at IOP goal after one SLT.
When SLT is repeatable, the probability of being drop free at 3 months jumps to 74%. The interval during which SLT is effective after the second treatment is at least equivalent to the interval between the initial and second rounds of SLT.3
In a nutshell, SLT is effective for an overwhelming majority of patients, and although temporary, repeat SLT can achieve effective IOP control over a 3-year period.
How does SLT address disease progression?
We learned early that IOP fluctuations are a
risk factor for glaucoma progression,
8,9 and SLT may provide better diurnal IOP control compared to drops, where IOP control is dependent on patient compliance. Therefore, we might conclude that due to the reduction in episodic IOP fluctuation with SLT, zero patients in the LiGHT study went on to need surgery in the laser group; as compared to 11 in the eye drop group.
3Into the future...
What is the role of the optometrist in managing patients who receive SLT?
I would recommend that optometrists seek OD-friendly ophthalmology colleagues in their local area and discuss their advanced level of practicing
glaucoma. Once the relationship is established, refer patients for the procedure and
co-manage post-op care, eventually resuming glaucoma care of your patient until further non-drop options are needed.
Post-operatively, patients typically start a topical NSAID and continue their IOP-lowering drops in the first month. Patients should return within 1 week for an IOP check, and 1 month for IOP and
gonioscopy. If sufficient IOP lowering is established, the optometrist may choose to reduce one drop therapy and monitor closely.
Resources
- Anwar Z, Wellik SR, Galor A. Glaucoma therapy and ocular surface disease: current literature and recommendations. Curr Opin Ophthalmol. 2013 Mar;24(2):136-43.
- Sacchetti, M., & Lambiase, A. (2014). Diagnosis and management of neurotrophic keratitis. Clinical ophthalmology (Auckland, N.Z.), 8, 571–579.
- Garg A, Vickerstaff V, Nathwani N, Garway-Heath D, Konstantakopoulou E, Ambler G, Bunce C, Wormald R, Barton K, Gazzard G; Laser in Glaucoma and Ocular Hypertension Trial Study Group. Primary Selective Laser Trabeculoplasty for Open-Angle Glaucoma and Ocular Hypertension: Clinical Outcomes, Predictors of Success, and Safety from the Laser in Glaucoma and Ocular Hypertension Trial. Ophthalmology. 2019 Sep;126(9):1238-1248.
- Kramer TR, Noecker RJ. Comparison of the morphologic changes after selective laser trabeculoplasty and argon laser trabeculoplasty in human eye bank eyes. Ophthalmology. 2001;108:773-779.
- Kennedy JB, SooHoo JR, Kahook MY, Seibold LK. Selective Laser Trabeculoplasty: An Update. Asia Pac J Ophthalmol (Phila). 2016 Jan-Feb;5(1):63-9.
- The Glaucoma Laser Trial (GLT). 2. Results of argon laser trabeculoplasty versus topical medicines. The Glaucoma Laser Trial Research Group. Ophthalmology. 1990 Nov;97(11):1403-13.
- The Glaucoma Laser Trial (GLT): 6. Treatment group differences in visual field changes. Glaucoma Laser Trial Research Group. Am J Ophthalmol. 1995 Jul;120(1):10-22.
- Caprioli J, Coleman AL. Intraocular pressure fluctuation a risk factor for visual field progression at low intraocular pressures in the advanced glaucoma intervention study. Ophthalmology. 2008 Jul;115(7):1123-1129.
- Nouri-Mahdavi K, Hoffman D, Coleman AL, Liu G, Li G, Gaasterland D, Caprioli J; Advanced Glaucoma Intervention Study. Predictive factors for glaucomatous visual field progression in the Advanced Glaucoma Intervention Study. Ophthalmology. 2004 Sep;111(9):1627-35.