Simple dimple? Cover-me-up . . .
Overview: Corneal dellen . . . what, how, why and who?
Definition: What is corneal dellen?
Pathophysiology: How does corneal dellen form?
Etiology: Why does corneal dellen form?
Typical patient type: Who is likely to experience corneal dellen?
- Patients who have had recent anterior eye surgery (post-operative dellen)3
- The elderly1
- RGP wearers6
- Dry eye patients2
- Patients with incomplete eyelid closure7
Presentation
Differential diagnosis of corneal dellen
- Peripheral corneal thinning, ulceration or degeneration3
- Corneal furrow degeneration (usually bilateral)4,8
- Terrien’s marginal degeneration (usually bilateral)4
Key Clue: Remember the defined dimple/ellipse/oval shape of a dellen and identify a causative area of elevation adjacent to it (unilateral condition).
Treatment and management options for corneal dellen
- Artificial tears and ointment as a baseline treatment3
- apply every two to four hours in the affected eye
- if the etiological cause cannot be eliminated, such as in the case of a filtering bleb, use viscous artificial tear drops four to eight times daily, preferably preservative-free
- Encourage eyelid-cornea surface contact / blinking action2,3
- identifying the etiology
- excision of causative elevated lesion, if dellen persists
- Patching3,6
- eye patching
- bandage contact lens
- Antibiotic ointment, if dellen persists with inflammatory signs3
- four times daily in the affected eye
- [Tear film instability allows the ocular surface to be more susceptible to infection. The normal, healthy tear film contains proteins, antibodies, and phagocytic cells which fight micro-organisms and act as a bactericidal system6]
- Autologous serum tears9
- four to six times daily in the affected eye, tapering as results prove satisfactory
- [These contain growth factors promoting cell proliferation and migration]
- Occlusion of punctum7
- punctal plugs
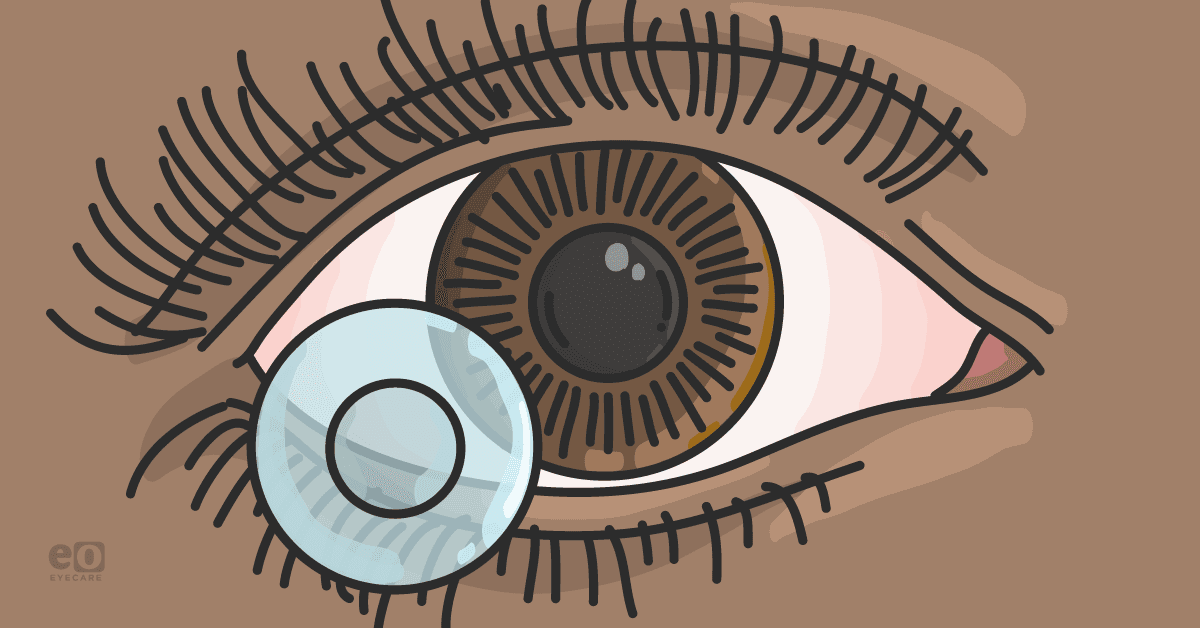
When to use bandage soft contact lenses with corneal dellen
- The contact lens diameter should be big enough to cover over the dellen
- Ensure that there is no contact lens edge mechanical abrasion to worsen the dellen depth
- The contact lens base curve should be compatible with the corneal curvature. Avoid a fit that’s too flat (increased movement upon eyelid blinking) or too steep, (little movement and minimal/no tear exchange beneath the lens).
- Lens material should allow for minimum lens dehydration6
- Hydrogel lenses (with a medium- to low-water content), allow for reduced in-eye dehydration. However, it cannot be used on an extended wear routine. Alternatively, a daily disposable lens can be used for already existing contact lens wearers, who are familiar with the insert, removal, and caring regimen.
- Silicone hydrogel (with a high-water content) are naturally hydrophobic. Although the latest technology advancements allow for increased lens surface hydrophilicity and lubricity. These lenses are more ideal for extended wear in non-contact lens wearers.
- Lens material should be compatible with patient’s tear film, for minimal lens surface deposits and contamination6
Patient script for treatment
- Introduce the treatment plan to the patient
- Ensure the patient knows in which eye to administer their eye drops
- Ensure the patient understands how often eye drop needs to be instilled
- Explain the timeframe of the treatment
- Alert the patient on any side effects and red-flag symptoms
- Schedule the follow-up visit with the known date and time before the patient leaves the consulting rooms and confirm the patient’s contact details.
Follow-up routine
Untreated dellen
ICD-10 coding
- Z09.0 – Follow-up examination after surgery
- H04.1 – Dry eye syndrome
- H18.8 – Erosion (recurrent) of cornea
Conclusion
References
- Grayson, M. Diseases of the cornea. Missouri : The C.V. Mosby Company, 1979. pp. 182, 276. 0-8016-1964-5.
- Chandler, W.C., Sugar, J. and Edelhauser, H.F. External Diseases. Singapore : Mosby, 1994. p. 9.12. Vol. 8. 1-56375-101-1.
- Bagheri, N. and Wajda, B.N. The Wills Eye Manual. 7. s.l. : Wolters Kluwer, 2017. pp. 90,91. 9781496318831.
- Bohigian, G.M. External diseases of the eye. Second. St. Louis : DAC Medical Publishing Assoc., 1982. pp. 43,44. 80-67605.
- 5. Episcleritis: An Everyday Infection. Rubinfeld, R. and Chase, C. 8, August 15, 2001, Review of Optometry, Vol. 138.
- Efron, N. Contact lens complications. Three. s.l. : Elsevier, 2012. pp. 87,90,255,152. 978-0-70-20-4269-0.
- Don’t Act Rash for Rash. Gurwood, A.S. 09, September 29, 2006, Review of Optometry, Vol. 143:09.
- Is Patient's Age a Factor? Gurwood, A.S. October 21, 2009, Review of Optometry.
- When Corneal Wounds Won’t Heal. Bozung, A. and Hammond, P. August 15, 2019, Review of Optometry.
- Anterior Segment OCT Revealed. Miller, J. October 20, 2009, Review of Optometry.
- A visual guide to some of the worst complications of the anterior segment. Sindt, C.W. January 15, 2014, Review of Optometry.
- Corneoscleral Concerns: Trouble at the Border. Mannen, M. April 15, 2021, Review of Optometry.