Glaucoma is one of the leading causes of blindness in the world. While there are many risk factors for the development of glaucoma, including age, genetics, race, and ethnicity, the only known modifiable risk factor is lowering the intraocular pressure (IOP). Many patients may reach their target IOP through conservative treatments, such as eye drops or in-office laser procedures; however, those with persistently elevated IOP despite maximally tolerated eye drops, or those with certain types of secondary glaucoma, may require incisional surgery.
The vast majority of glaucoma surgeries lower IOP by increasing aqueous outflow, either through decreasing the resistance to outflow through the trabecular meshwork and Schlemm’s canal (e.g., goniotomy, canaloplasty, iStent, Hydrus) or creating a new outflow channel (e.g., trabeculectomy and conventional glaucoma drainage devices). Recent advances have targeted new systems, such as the uveoscleral pathway (i.e., CyPass). Finally, the amount of aqueous produced may be decreased through targeting the ciliary body (e.g., endocyclophotocoagulation).
Throughout this guide, we will review currently available surgical procedures and techniques for glaucoma. It is important to note that there are substantial differences in surgical technique amongst surgeons, and techniques may even vary by the surgeon based upon eye characteristics. Additionally, while some pre- and postoperative management strategies are covered, this guide does not include all nuances of perioperative management.
Glaucoma Filtration Surgery
Trabeculectomy
Trabeculectomy, one of the oldest glaucoma surgeries, remains one of the most effective glaucoma surgeries for lowering IOP, and, despite advances in implantable devices and MIGS, its utility in glaucoma management remains pivotal. During a trabeculectomy, a fistula, or pathway, is created through the angle and sclera to allow aqueous humor to flow from the anterior chamber into the subconjunctival space. The accumulated fluid forms an elevated subconjunctival fluid-filled pocket called a bleb and is taken away by the conjunctival and episcleral vascular and lymphatic systems.
The amount of aqueous humor that egresses can be titrated intraoperatively by adjusting the size of the ostium and the tension of a partial-thickness scleral flap, which covers the ostium and can be adjusted postoperatively through laser suture lysis (LSL) of the flap sutures or with the use of releasable sutures.
As the eye heals, scarring within the bleb typically occurs, leading to an elevation in IOP. The risk of scarring can be reduced during the procedure by utilizing an antimetabolite, such as mitomycin-C (MMC) or 5-fluorouracil (5-FU), and can be managed post-operatively through bleb needling with or without the use of antimetabolites. The nuances of trabeculectomy surgical technique are essential as the immediate and long-term surgical success of trabeculectomies depends on a delicate balance between IOP lowering and hypotony, conjunctival thinning and scarring, and other factors.
There are many things to consider when selecting good trabeculectomy candidates. Trabeculectomies are one of the few glaucoma surgical procedures that, if successful, can allow for IOP in the 5-15mmHg range and are helpful in patients with low IOP targets. Given the relatively higher risk of intra- and postoperative complications compared with other glaucoma surgeries—such as suprachoroidal hemorrhage, hypotony, bleb leakage, and blebitis/endophthalmitis—a trabeculectomy may not be necessary for patients who do not require lower IOP targets.
Patient demographics play an essential role in trabeculectomy consideration, as trabeculectomies are less successful in patients who are younger and are less successful in certain races and ethnicities (mainly in black and Hispanic patients) due to the increased propensity for conjunctival scarring and bleb failure in these patient populations.1 Conjunctival health is important to create a good bleb, and trabeculectomies are often avoided in patients with a history of conjunctival surgery.
While trabeculectomies can be utilized in both open and closed-angle glaucoma types, they should be typically avoided in patients with intraocular inflammation (e.g., uveitic glaucoma) and those with a propensity towards scarring and adhesion formation (e.g., neovascular glaucoma, ICE syndrome).
Surgical technique
1) Setting up
As with most glaucoma surgery, trabeculectomy may be performed with either local anesthesia, moderate sedation, or general anesthesia. For patients not undergoing general anesthesia, a retrobulbar or peribulbar block may be performed, though care must be taken to limit the amount of anesthetic injected so as to not cause posterior pressure on the globe. The eye is surgically prepped, and a partial-thickness superior corneal traction suture is placed.
2) Conjunctival flap creation
The first step consists of opening the superior conjunctiva to allow for access to the sclera. Two types of conjunctival incision techniques may be used, and they are named based upon where the hinge of the conjunctival flap is located (which is opposite the location of the conjunctival incision): a fornix-based flap (i.e., limbal-based incision) and a limbal-based flap (i.e., fornix-based incision).
Typically, a 2-3 clock hour incision, called a peritomy, is created, and through this incision, the conjunctiva is carefully and meticulously dissected off bare sclera to ensure no remaining Tenon’s capsule. The conjunctiva should be handled delicately with appropriate conjunctival forceps (ideally non-toothed, non-serrated) to avoid tearing. A large area is dissected laterally and posteriorly to ensure good bleb formation. Hemostasis should be maintained through cautery.
3) Antimetabolite application
After the conjunctiva and Tenon’s are dissected off the bare sclera, MMC or 5-FU can be applied to the subconjunctival space for a fixed period of time (typically 30 seconds and up to 5 minutes). We prefer using MMC with a concentration of 0.2 to 0.4 mg/mL and applying it for 1 minute. We find creating small pledgets from cut Weck-Cel sponge tips to be useful for this purpose. The pledgets are then removed, and the area is irrigated copiously. Alternatively, the antimetabolite can be applied as an injection prior to conjunctival flap creation. Care should be taken to avoid touching the antimetabolite to the cornea and limbus.
4) Creation of a scleral flap
A partial-thickness scleral flap is then created near the limbus. A variety of scleral flap sizes and shapes (e.g., triangular, rectangular, square, or trapezoidal) can be created depending on surgeon preference. The scleral flap is outlined via a partial-thickness incision (approximately 50% thickness). A flap is created through lamellar dissection. Dissection is continued anteriorly until the bluish-gray zone of the limbus is reached, such that a hinge remains at the limbal edge of the flap. Care should be taken to keep the flap thickness equal throughout.
5) Entry into the anterior chamber and ostium creation
Prior to the creation of a pathway between the scleral flap bed and the anterior chamber, it is crucial to create a paracentesis to ensure good access to the anterior chamber. Remember to create the paracentesis in an area that will be easily accessible at the slit lamp (we prefer placing it temporally) in the event the anterior chamber needs to be reformed during the postoperative period. The anterior chamber is then entered under the flap hinge via an incision parallel to the iris plane, and a piece of scleral and limbal tissue is resected to allow for open communication between the anterior chamber and scleral flap bed. This ostium can be created with a Kelly punch or can be excised manually with a blade.
This is the part of the surgery that gives “trabeculectomy” its name, but it is a misnomer! Most pieces of tissue contain a combination of sclera, limbus, and angle structures (somehow, “keratosclerotrabeculectomy” doesn’t have the same ring to it). After the ostium is created, a peripheral iridectomy may be performed by pulling a small amount of iris tissue through the ostium and excising it with scissors.
6) Scleral flap closure
Once there is open communication with the anterior chamber, the scleral flap must be tied down rather quickly with non-absorbable sutures. If the anterior chamber becomes shallow or flat, it can be reformed by using balanced salt solution (BSS). Because of the need to rapidly suture the flap, some surgeons prefer to pre-place sutures prior to entering the anterior chamber and tying the suture knots afterward. The knots are rotated to avoid erosion through the conjunctiva. The tension of each suture must be carefully considered, as too tight of a flap won’t allow for any fluid egress, and too loose of a suture will lead to over filtration and hypotony. At least two flap sutures are placed; however, more sutures may allow for more control postoperatively.
Some surgeons prefer to tie these sutures with releasable knots; other surgeons prefer to place standard knots and sever the sutures afterward using transconjunctival laser suture lysis. The flow through the scleral flap can be tested by injecting BSS into the anterior chamber and monitoring the amount of fluid leaving the eye, and palpating the tension of the eye once it reaches homeostasis. It is not uncommon to cut and replace the sutures if it is determined they are too tight or loose.
7) Conjunctival closure
Conjunctival closure is an incredibly important step and failing to inadequately close the conjunctiva may lead to bleb leakage which could cause infection or hypotony. The conjunctiva is approximated using absorbable or non-absorbable sutures and partial thickness scleral and/or limbal suture passes. If a fornix-based flap is utilized (meaning a limbal peritomy was performed, enough horizontal tension must be present at the limbus to ensure no bleb leakage. Bleb closure can be tested by indirectly inflating the bleb by injecting the anterior chamber with BSS. The wound may also be tested with fluorescein strips.
Trabeculectomy variations
Several devices have been developed to limit the risk of hypotony by inserting an implant with a fixed ostium size. These devices may also cut down on procedure time and variability by modifying the crucial step where a block of scleral tissue is resected and the flap is sutured. EX-PRESS Glaucoma Filtration Device (Alcon Laboratories, Inc., Texas, USA) and XEN gel stent (Allergan, Inc., Dublin, Ireland) are two FDA-approved implants. The EX-PRESS device is a stainless-steel implant that is inserted into the anterior chamber through the scleral at the limbal edge. Due to the risk of erosion through the conjunctiva, surgeons may prefer to create a scleral flap to cover the device.
XEN gel stent may be implanted either via an ab interno (meaning the device is injected from the anterior chamber into the subconjunctival space, avoiding the need to open the conjunctiva) or ab externo approach. Since the stent may kink or encapsulate on Tenon’s capsule, requiring postoperative needling, some surgeons have begun to prefer an ab externo approach, where a conjunctiva peritomy is performed, and the conjunctiva is dissected off of bare sclera prior to the stent being injected from the sclera into the anterior chamber.2 Similar devices may be available in the US soon, including InnFocus MicroShunt (Santen, Osaka, Japan).
Conventional glaucoma drainage devices
Glaucoma drainage device procedures entail implanting a tube with a fixed lumen size into the eye, either via anterior chamber, sulcus, or pars plana, to allow the aqueous to drain into a subconjunctival reservoir. The tubes may be valved, designed to reduce the risk of postoperative hypotony, or non-valved. Currently available FDA-approved valved-devices include Ahmed Glaucoma Valve; non-valved devices include Molteno implant (Molteno Ophthalmic Limited, Dunedin, New Zealand), Baerveldt Glaucoma Implant (Johnson & Johnson Vision, California, USA), and Ahmed ClearPath (New World Medical, Inc., California, USA).
Non-valved tubes require modifications to prevent hypotony until a fibrous capsule forms around the external reservoir, which typically takes about 4-6 weeks. Compared with trabeculectomies, surgical success is less dependent on the presence of conjunctival scarring, and the devices may be placed in eyes with prior conjunctival surgery (including prior trabeculectomy), and they can be placed inferiorly. Multiple tubes may be placed within a single eye. Most commonly, the primary tube is placed superotemporally, and secondary tubes are typically placed either superonasal or inferonasal—the inferotemporal quadrant is usually avoided as it has the most exposure, resulting in a higher risk of tube erosion due to more lid movement over the subconjunctival portion of the tube3 and poor cosmetic results.
Surgical technique
1) Setting up
Local, conscious sedation, or general anesthesia may be performed, with or without a peri- or retrobulbar block. A partial-thickness corneal traction suture is placed at the limbus on whichever quadrant the device is to be implanted.
2) Conjunctival peritomy
A limbal peritomy is performed for approximately three clock hours, and the conjunctiva is dissected posteriorly to the bare sclera. Be careful to avoid the eye muscles, particularly the superior oblique if superonasal and the inferior oblique if inferonasal. Radial relaxing incisions are created cutting the conjunctival from the limbus posteriorly at the edges of the quadrant to allow more visualization and access. Hemostasis is maintained with cautery (we prefer 18-gauge eraser tip bipolar cautery). Surgeons may consider lightly blanching the tentative sclerotomy site.
3) Plate placement
The patency of the implant is confirmed by gently flushing the tube with BSS. The external reservoir, or plate, is then placed posteriorly underneath the conjunctiva. Most are placed such that the anterior edge of the plate is 8-10 mm posterior to the limbus. Larger devices, such as Baerveldt implants, may require placement under the recti muscles by hooking and isolating the muscle and sliding the plate underneath the muscle belly. Two-plate devices require the implantation of one plate per quadrant.
Once the plate is in a good position, it is sutured to the sclera via partial-thickness scleral bites with a non-absorbable suture, and the suture knots are rotated to avoid erosion through the conjunctiva.
4) Sclerostomy and tube insertion
Prior to entering the anterior chamber, it is important to create a paracentesis. The tube is then trimmed to an appropriate length (typically such that it has a length of 2.5 to 3mm in the anterior chamber) at approximately a 45-degree angle such that the bevel faces away from the iris (i.e., facing anteriorly for anterior chamber tubes, and posterior for sulcus-based tubes).
If the tube is non-valved, the tube is ligated with an absorbable or non-absorbable suture; tube fenestrations may also be created on the side closest to the anterior chamber to allow for early IOP lowering. Alternatively, a ligature suture may be inserted into the lumen of the tube—this can be later pulled at the slit lamp. Some surgeons prefer two-stage procedures for non-valved tubes in high-risk eyes. The plate is placed during the first surgery, and the tube is inserted into the anterior chamber several weeks later once a capsule has formed.
The eye is then rotated away from the quadrant being worked on with the help of the corneal traction suture. For anterior chamber placement, we prefer to create a partial thickness scleral tunnel with a 22 or 23-gauge needle starting approximately 3 mm posterior to the limbus. Advance the needle towards the limbus, and once approximately 0.5 posterior to the limbal border, redirect the needle into the anterior chamber such that it is anterior and parallel to the iris plane. The non-dominant hand can pull the eye back into primary position to help redirect the needle and improve visualization.
The tube is then inserted into this scleral tract. The scleral tunnel can be easily lost, and it is helpful to maintain good visualization of the proximal opening of the tract. Fine toothed forceps may help open the anterior lip of the tract, and the tunnel can also be accessed and dilated with the use of viscoelastic on a cannula.
Tubes may also be placed more posteriorly to reduce the risk of corneal decompensation:
a) Sulcus tube placement: If the eye is pseudophakic or aphakic with an intact capsule (or vitrectomized), the tube may be inserted posterior to the iris. The tract is started approximately 1 mm more posteriorly (that is, 4-5 mm posterior to the limbus), and the needle is directed into the sulcus space about 2 mm posterior to the limbus.
As the sulcus space can be challenging to access, it is advantageous to delineate the sulcus space with viscoelastic. Some surgeons may find it easier to create the sclerotomy from an ab interno approach by entering the eye via a paracentesis with a long needle 180-degrees away from sclerotomy site, accessing the sulcus space, and then externalizing the needle through the sclera. We prefer to leave the tubes just long enough to be visualized while dilated, and for this reason, it may be helpful to dilate patients prior to surgery.
b) Pars plana placement: This is reserved for pseudophakic or aphakic eyes that have been vitrectomized. Care must be taken by the vitreoretinal surgeon to shave close to the vitreous base in the area of tube placement and to perform a thorough vitrectomy (as vitreous can easily clog the tube!). The sclerotomy is created 3.5 – 4 mm posterior to the limbus, and minimal scleral tract is needed. Due to the more abrupt angulation, a pars plana clip or elbow may be required.
This is often always performed in conjunction with a vitreoretinal surgeon at the time of pars plana vitrectomy, and it is useful to be able to visualize the tube and confirm appropriate placement.
5) Patch graft placement
The tube may be secured to the underlying sclera using partial thickness suture passes. The tube is then covered with a patch graft to help reduce the risk of tube erosion through the conjunctiva. Most physicians use either a portion of donor corneal tissue (usually tissue deemed unfit for corneal transplantation) or processed tissue, such as processed sclera, pericardium, dura, or fascia lata. The patch graft is secured to the underlying sclera using partial thickness suture passes and typically an absorbable suture. Alternatively, a partial thickness scleral flap may be constructed.
6) Conjunctival closure
The conjunctiva is then closed in a fashion similar to trabeculectomies. Care should be taken to ensure tight closure at the limbus. The radial conjunctival incisions are approximated together using interrupted or running sutures.
Angle-based procedures
In glaucoma management, conjunctival real estate is highly prized. Many glaucoma surgeons prefer a conjunctival-sparing approach; this is particularly useful as a primary surgery as surgeons may want to save conjunctival procedures for later. It may also be of use in patients with unhealthy conjunctival tissue or those who are poor trabeculectomy or tube shunt candidates.
There has also been a push to develop procedures with a lower side-effect profile than trabeculectomy or conventional glaucoma drainage devices. Therefore, a new class of glaucoma surgeries, called Minimally Invasive Glaucoma Surgery (MIGS), has been recently developed. These procedures are characterized by a high safety profile, minimal disruption to normal anatomy, ab interno approach, meaningful IOP-reducing efficacy, and ease of use.4
These procedures target angle structures and can be broken down into those that bypass the trabecular meshwork tissue and access Schlemm’s canal and the collector channel systems (such as Schlemm’s canal devices, goniotomy, and canaloplasty) and suprachoroidal devices that access the uveoscleral pathway.
Angle-based procedures require good visualization of the angle structures and an open angle—therefore, the cornea must be clear enough to perform intraoperative gonioscopy, and the angle structures cannot be covered by peripheral anterior synechiae (PAS). This does not entirely mean that angle-based procedures cannot be performed on patients with narrow angles, mainly if PAS is absent. If the procedure is combined with cataract extraction, the anterior chamber and angle will likely deepen once the phakic lens is removed.
Schlemm’s canal devices
Several implant-based angle procedures have been developed to bypass resistance to outflow and target the collector channel system, including iStent, iStent inject, and iStent inject W (Glaukos Corp., California, USA) and Hydrus Microstent (Ivantis, Inc., California, USA). iStent was initially developed as a single micro-stent that was implanted into the posterior, pigmented trabecular meshwork. Since the first generation’s release in 2012, there have been several changes to the stent design and injector system. The current model, iStent Inject W, allows for the implantation of two micro-stents. Hydrus Microstent is a longer, scaffold-like implant that spans 90 degrees of the trabecular meshwork and opens Schlemm’s canal to enhance trabecular outflow.
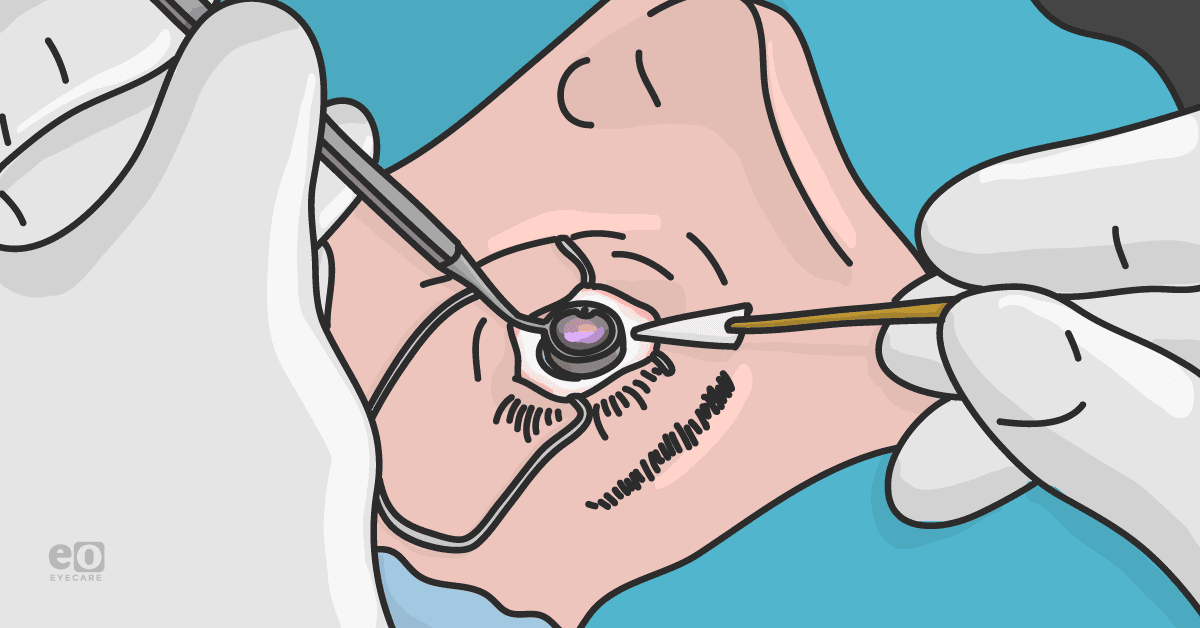
Procedure basics
After cataract extraction and implantation of the intraocular lens, the anterior chamber and particularly the nasal angle is inflated with viscoelastic (we prefer a cohesive viscoelastic and find benefit with high molecular weight viscoelastic). The head of the patient is rotated away from the surgeon, and the microscope is tilted and rotated towards the surgeon. The cornea is coated with a coupling agent (we prefer a cohesive viscoelastic), and the nasal angle is visualized with the use of an appropriate sterile direct gonioscopy lens. The injector system is placed into the anterior chamber through the main surgical wound, and two stents are placed in the superonasal and inferonasal pigmented trabecular meshwork.
With the current injector model, the stents are placed by clicking the injector button. Bias of the injector needle, strong dimpling of the trabecular meshwork tissue, and improper tissue placement may cause the stent, not the implant; however, stent implantation can be reattempted (there are a total of four clicks with the current model). Care should be taken to avoid the 3 and 9 o’clock positions to avoid the long ciliary nerve.
For Hydrus implantation, the anterior chamber is again filled with viscoelastic, and the patient head and microscope are positioned to allow for visualization of the nasal angle. Unlike iStent inject and iStent inject W, which is implanted perpendicular to the trabecular tissue, Hydrus is inserted parallel to the tissue and follows the curve of the angle.
Goniotomy
While indeed not a new concept, goniotomy procedures have recently had a resurgence thanks to new surgical tools. During a goniotomy, a surgeon opens or excises a piece of trabecular meshwork tissue under gonioscopic visualization. Goniotomy may be performed as a stand-alone procedure (meaning without cataract surgery). Some newer surgical devices may also allow for canaloplasty at the time of goniotomy. Goniotomy devices include Kahook Dual Blade (New World Medical, California, USA), Trabectome (Neomedix, California, USA), and Trab 360/OMNI (Sight Sciences, California, USA).
Procedure basics
A partial goniotomy may be performed with the utilization of an appropriate blade or device, such as Kahook Dual Blade or Trabectome. If performing the goniotomy at the time of cataract surgery, the lens is first removed, and the intraocular lens is implanted. If performing as a stand alone procedure, a paracentesis and main temporal wound (we prefer at least a 2.0mm wound) are created, and topical anesthesia is injected into the anterior chamber. The anterior chamber and nasal angle are inflated with viscoelastic and the patient and scope are positioned as previously described.
The nasal angle is visualized under direct gonioscopic view, and the goniotomy blade is introduced into the eye via the primary surgical wound. Three to four clock hours of trabecular meshwork tissue are excised; an incision going the opposite direction may need to be performed to entirely excise the tag of tissue. Trabectome utilizes electrocautery and provides irrigation and aspiration, which aid in clearing of debris.
A more extensive goniotomy may be performed. Gonioscopy-assisted transluminal trabeculotomy (GATT) is a procedure in which a nasal goniotomy is performed, and through this incision, a suture or catheter (e.g., iTrack [Ellex iScience, California, USA]) is inserted and advanced circumferentially 360 degrees. The suture or catheter is then pulled out of the eye to shear the trabecular meshwork tissue. A similar procedure may be performed with TRAB 360/OMNI, where a microcatheter is advanced 180 degrees with the use of an injector after the nasal trabecular meshwork tissue is nicked. The procedure can then be repeated with the opposite 180 degrees for a full, 360-degree goniotomy.
Canaloplasty
Similar to GATT and TRAB 360/OMNI, Schlemm’s canal can be accessed with use of a catheter and then dilated with use of viscoelastic. This can dilate both Schlemm’s canal and the distal outflow systems to help reduce the resistance to outflow. Two devices are currently approved: VISCO360/OMNI (Sight Sciences, California, USA) and Ab interno canaloplasty (Ellex iScience, California, USA).
The OMNI system is a single-use injector system that allows for canaloplasty and goniotomy during the same procedure. Once the catheter is advanced for 180 degrees, viscodilation is performed by injecting a predetermined amount of viscoelastic as the catheter is pulled out through the goniotomy incision; the catheter is then reintroduced, and a goniotomy is performed.
Ab interno canaloplasty (ABiC) is performed using the iTrack system, which includes a blinking light at the distal tip of the catheter. The catheter is advanced 360 degrees into Schlemm’s canal, and the catheter is then slowly withdrawn while performing viscodilation. As previously mentioned, this device may also be used to perform a 360-degree goniotomy.
Suprachoroidal Devices
Suprachoroidal devices target and take advantage of the uveoscleral outflow pathway. As of the time this article was written, there are no devices currently approved by the FDA. The only device to have received FDA approval is the CyPass Micro-Stent (Alcon Laboratories, Inc., Texas, USA); however it was withdrawn from the market in 2018 due to concerns of endothelial cell loss related to mispositioned stents. Potential future devices include iStent SUPRA (Glaukos Corp., California, USA), SOLX gold shunt (SOLX, Inc., Massachusetts, USA), MINIject (iStar Medical, Wavre, Belgium), and STARflo (iStar Medical, Wavre, Belgium).
Ciliary body-targeting procedures
Unlike the previously mentioned procedures, which increase aqueous outflow, procedures that target the ciliary body aim to lower IOP by decreasing the rate of aqueous production. They may be broken down into endocyclophotocoagulation (BVI, New Jersey, USA) which is an intraocular surgery, and transscleral or incisionless procedures, which include cyclophotocoagulation and MicroPulse Transscleral Laser Therapy (Iridex, Inc., California, USA). These procedures utilize a laser that is delivered at a fixed wavelength (typically 810nm) which is absorbed by the pigmented epithelium of the ciliary body.
Historically, procedures that targeted ciliary body tissue were reserved for end-stage glaucoma, as these procedures were cyclodestructive in nature, meaning that the ciliary body tissue was irreversibly destroyed. More recently, particularly with the development of endocyclophotocoagulation (ECP) and MicroPulse Transscleral Laser Therapy (MicroPulse TLT), these procedures can be safely performed on earlier disease given the lower side effect profile and reduced risk of hypotony and phthisis.
Endocyclophotocoagluation
Endocyclophotocoagulation (ECP) is a procedure unique to the field of glaucoma as it involves an intracameral endoscopic visualization. The procedure may be performed at the time of cataract surgery or as a stand-alone procedure. The surgeon introduces an endoscopic probe, which contains a light source and camera, through a clear corneal incision; through a second corneal incision, the laser probe is introduced. The anterior portion of the ciliary body is visualized on an external video source, and the ciliary processes are lasered until they blanch and contract.
Transscleral Laser Procedures
Transscleral incisionless laser procedures have been developed to target the ciliary body tissue. Traditional or continuous-wave transscleral cyclophotocoagulation (CPC) is a cyclodestructive procedure that delivers laser energy at fixed energy and duration. The CPC probe is used to deliver laser energy at several spots at the pars plicata; typically, 270-degrees of treatment is given, with sparing of the superotemporal quadrant to reduce the risk of hypotony.
MicroPulse TLT delivers laser energy in small bursts, where “on cycles” are interrupted by “off cycles” to reduce the risk of coagulative damage and tissue necrosis. While the exact mechanism of action has yet to be elucidated, it appears to cause changes in the conformational structure of the ciliary body that may increase outflow through traditional pathways rather than reduce the risk of aqueous production.5 Unlike CPC, where the laser is delivered continuously at discrete spots, MicroPulse TLT is delivered by sweeping the probe back and forth along the pars plicata.
In Closing
While IOP may be the only modifiable risk factor, there are now numerous treatment modalities for glaucoma management. Less invasive and lower-risk procedures, such as MIGS and MicroPulse TLT, have revolutionized surgical paradigms. Even still, traditional procedures, like trabeculectomy and glaucoma drainage device implantation, remain pivotal in the treatment of glaucoma.
Citations
- Broadway DC, Chang LP. Trabeculectomy, risk factors for failure and the preoperative state of the conjunctiva. J Glaucoma. 2001;10(3) 237-249. doi: 10.1097/00061198-200106000-00017. PMID: 11442190.
- Panarelli JF, Yan DB, Francis B, Craven ER. XEN gel stent open conjunctiva technique: a practical approach paper. Adv Ther. 2020;37(5):2538-2549. doi:10.1007/s12325-020-01278-1. PMID: 32200534.
- Pakravan M, Yazdani S, Shahabi C, et al. Superior versus inferior Ahmed glaucoma valve implantation. Ophthalmology. 2009;116(2):208-13. doi: 10.1016/j.ophtha.2008.09.003. PMID: 19062098.
- Saheb H and Ahmed I. Micro-invasive glaucoma surgery: current perspectives and future directions. Current Opinions Ophthalmol. 2012;23(2) 96-104. doi: 10.1097/ICU.0b013e32834ff1e7. PMID: 22249233.
- Moussa K, Feinstein M, Pekmezci M, et al. Histologic changes following continuous wave and MicroPulse transscleral cyclophotocoagulation: a randomized comparative study. Transl Vis Sci Technol. 2020;9(5):22. doi: 10.1167/tvst.9.5.22. PMID: 32821494.