Morgagnian cataracts are an uncommon entity to encounter in the United States, but when they do present, the eyecare provider has both a challenge in surgical management and also a great opportunity to help dramatically improve a patient’s vision and lifestyle.
Morgagnian cataracts (name derived from Giovanni Battista Morgagni) develop as a cortical cataract matures and the lens fibers degenerate and liquefy, leaving the nucleus floating in liquefied cortical material.1,2 It is an accumulation of spherical globules or Morgagnian globules of broken down cortical cell walls that eventually replaces the entire lens cortex with a liquid-like material.3 There is a risk of phacolytic glaucoma in these patients as the liquefied lens proteins can leak through the capsule (even if it appears intact) and obstruct the trabecular meshwork.4
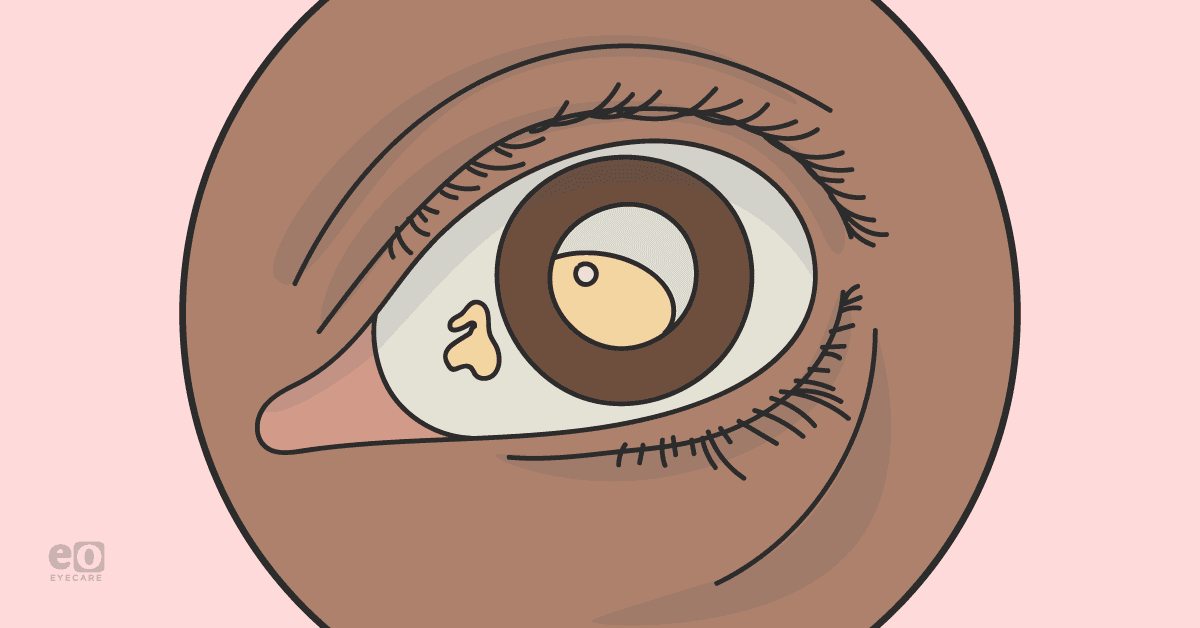
The clinical manifestations of a Morgagnian cataract include a significant decrease in vision (count fingers or hand motion) in addition to a dense brown nucleus floating in liquefied white cortical lens material. The anterior lens capsule may display calcium deposits.
A Morgagnian cataract is a clinical diagnosis made on slit-lamp examination; moreover, the “Triangle sign” has been described which can be seen using a narrow slit beam angled and focused above the nucleus which shows a triangular area bounded by the anterior and posterior capsule with the nucleus as the base.5
Morgagnian cataract case report:
A 62-year-old woman with a past medical history of hypertension presented with progressive decreased Hand Motion (HM) vision in both eyes. Intraocular pressure and extraocular motility were within normal limits; there was no relative afferent pupillary defect. The anterior segment exam was remarkable for a hypermature cataract OU.
When examining the lens in the right eye, there was an obvious white cataract, with a dense brown crescent floating inferiorly (nucleus). The left lens was a mature white lens. There was no view of the posterior segment. A B-scan was obtained which did not reveal any abnormalities of the fundus.
After a detailed discussion with the patient about the risks and benefits of cataract surgery, including an increased risk of anterior capsular tear, dropped nucleus, and need for further surgical procedures, the patient was taken to surgery one week after her clinic visit.
In the operating suite, after prep and draping, the surgery began with the creation of a standard side port and main incision. Next, Trypan blue was used to stain the anterior capsule. This is a crucial step for adequate visualization of the lens capsule for the ensuing capsulorrhexis.
I place an air bubble prior to Trypan injection to aid in the staining. Viscoelastic was then injected to displace and remove the Trypan and air bubble. Following this, as with all white/intumescent cataracts, I used a 27G needle on a 3cc syringe ½ filled with BSS to puncture the capsule centrally and attempt to remove cortical material and the pressure.
Interested in other complex cataract case reports? Check out the reports on White Cataracts and the Dense Cataract with Malyugin Ring and miLOOP!
This step is an effort to reduce the risk of an Argentinian flag during rhexis creation. I then use a bent cystotome to begin the capsulorrhexis. At this point, large amounts of liquefied cortex began to escape into the anterior chamber obscuring my view of the capsule.
One could choose to displace this with more viscoelastic or aspirate it out—I chose the latter given the amount and density of this white, thick material. Next, I used Utrata forceps to complete the rhexis. While creating the rhexis more lens material was pouring from the capsular bag, further obscuring the view.
After this was completed successfully, it was time for nucleus removal. There is no need for hydrodissection or delineation. Given the fact that there is no solid cortical material to hold the nucleus in place, a groove technique is difficult. I prefer a vertical chop technique and dividing the nucleus into six sections.
After this was completed, I moved to polish the lens capsule and insert the intraocular lens (IOL) in the capsular bag.
Photo 1 represents the view at the start of the case.
Photo 1
Photo 2 illustrates instillation of Trypan Blue under air bubble.
Photo 2
Photo 3 shows the escape of liquefied lens material during capsulorrhexis.
Photo 3
Photo 4 demonstrates capsulorrhexis with Utrata forceps.
Photo 4
Photo 5 illustrates lens disassembly.
Photo 5
On post-operative day 1, the patient was now 20/25 sc and fairly happy with the improvement in the vision. She had her second eye cataract surgery 2 weeks later with similar results.
Discussion
Encountering a Morgagnian cataract in clinic is an unusual opportunity to dramatically improve a patient's vision. Pearls include the possibility of phacolytic glaucoma and need for a proper view of the fundus using echography.
Surgical removal is dependent on good capsular visualization (e.g., Trypan). Additionally, the unique challenge with a Morgagnian cataract is the escape of liquefied cortical material that obscures your view during capsulorrhexis creation.
As discussed, this can be managed by aspirating carefully as the liquid escapes. Finally, during nuclear disassembly, keep in mind a chop technique is preferred, since there is no cortical material to hold the nucleus in place for a groove or divide and conquer technique.
References
- Albert D, Miller J, Azar D, Blodi B. Cataractogenesisi in the Adult. Albert & Jakobiec's Principles and Practice of Ophthalmology. Philadelphia: Saunders Elsevier Inc, 2008
- Rozenbaum I. The Faces Behind the Eponyms. Arch Ophthalmol. 2008;126(6):846. doi:10.1001/archophthalmol.2007.63
- Roger F. Steinert. Cataract surgery 3rd edition. Chapter 1, The pathology of cataracts. CA, USA: Elsevier Inc.; 2010
- Epstein DL, Jedziniak JA, Grant WM. Identification of heavy-molecular-weight soluble protein in aqueous humor in human phacolytic glaucoma. Invest Ophthalmol Vis Sci. 1978;17(5):398-402.
- Deshmukh S, Bhattacharjee H, Gupta K. “Triangle sign”in Morgagnian cataract. Indian J Ophthalmol 2019;67:137