Ocular oncology is the study of benign and malignant tumors of the eye. Even though metastases are the most common type of intraocular tumor,
uveal melanoma represents the most common primary intraocular tumor in adults, with a prevalence of five per million in the United States.
In this article, we will discuss five pearls and advancements in the field of ocular oncology, emphasizing intraocular and ocular surface tumors.
Overview of intraocular and ocular surface tumors
A substantial percentage of patients with intraocular tumors may be asymptomatic, with the lesion diagnosed on a routine eye exam by their optometrist or comprehensive ophthalmologist. Once a lesion is identified, it can also be difficult to determine if it is benign or malignant.
After diagnosis, patients may ask if there are treatments for this condition. Given the life-threatening nature of these conditions, it is critical for
comprehensive ophthalmologists to be aware of common tumors, when to initiate a referral, and different treatment options.
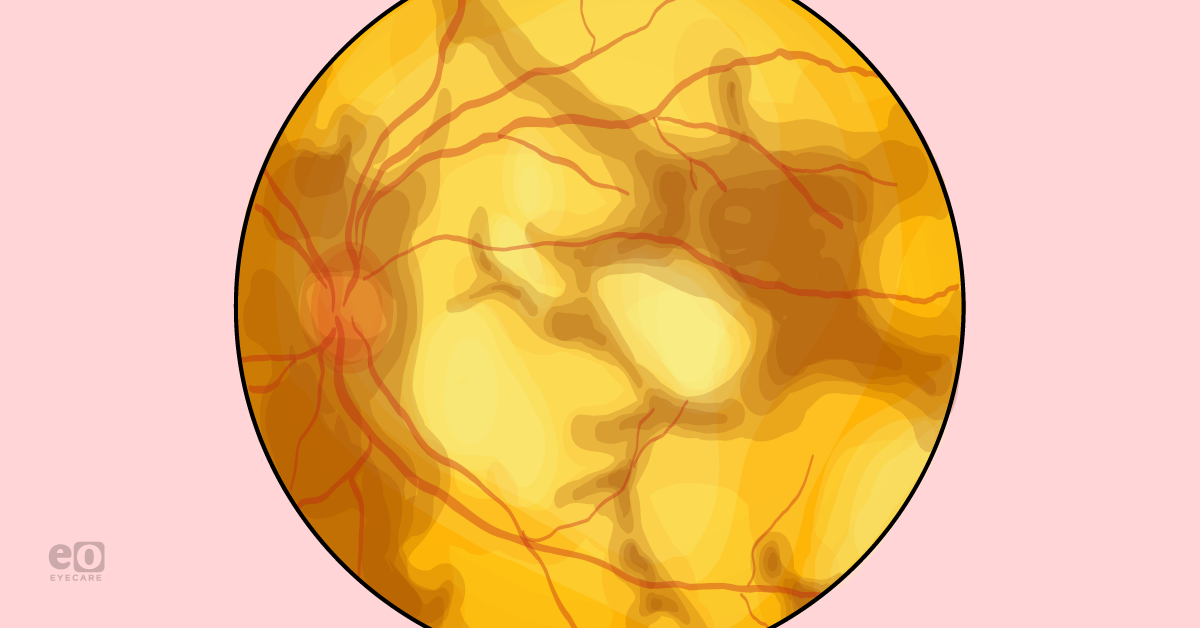
1. Acronyms can help in the decision to refer choroidal nevi
The most important question facing the ophthalmologist for every
choroidal melanocytic lesion is whether it is a choroidal nevus or melanoma. Though most choroidal melanomas occur
de novo, there is a spectrum that exists between the two conditions. It is crucial to identify features that increase the risk of malignant transformation and refer promptly when indicated.
Understanding the acronym TFSOM
Several acronyms have been established to help clinicians perform risk stratification of choroidal melanocytic lesions. One of the most used mnemonics coined by
Shields et al. is "To Find Small Ocular Melanoma" (TFSOM).
1 They later added “Using Helpful Hints Daily,” and most recently, updated it to “Doing IMaging” (TFSOM-DIM, shown below in Table 1).
2,3The mean 5-year estimates of malignant transformation using TFSOM-DIM were 1.1% for patients with no risk factors, 11% for those with one, 22% for those with two, 34% for those with three, 51% for those with four, and 55% for those with five.
2 The latest update of the acronym relies on multimodal imaging, which may be a challenge for those who may not have access to experienced ultrasonographers or
widefield imaging for peripheral lesions.
Table 1 outlines the TFSOM-DIM acronym for stratifying the risk of malignant transformation of nevi.
| Acronym | Corresponding Meaning |
|---|
| To | Thickness >2mm (ultrasonography) |
| Find | Subretinal fluid, initially clinically—now with OCT |
| Small | Symptoms, now vision loss worse than or equal to 20/50 |
| Ocular | Orange pigment, initially clinically—now on autofluorescence |
| Melanoma | Initially margin ≤3mm from optic disc, now melanoma is hollow (ultrasonography) |
| Doing IMaging | Diameter >5mm (fundus photography) |
Table 1: Courtesy of Shields et al.
Breaking down the acronym MOLES
Another acronym developed for non-ocular oncologists is MOLES, designed to assess risk factors based on ophthalmoscopy (see Table 1). The system assigns zero to two points each for mushroom shape, orange pigment, large tumor size, enlarging tumor, and subretinal fluid. It then categorizes a lesion as a common nevus (zero points), low-risk nevus (one point), high-risk nevus (two points), and probable melanoma (three or more points) according to the sum of scores.
Any lesion with a score of zero can be monitored every 1 to 2 years; those scoring one to two are recommended to undergo multimodal imaging with B-scan ultrasonography, optical coherence tomography (OCT), and
fundus autofluorescence; those scoring three or more are recommended to be urgently referred to an ocular oncologist. A retrospective analysis using MOLES found that it was a highly sensitive (99.8%) tool in guiding the need for referral to an ocular oncologist.
4Table 2 summarizes the MOLES acronym for clinical stratification of nevi (scores zero to two) and identification of probable melanomas (score greater than or equal to three).
| Feature | Identification |
|---|
| Mushroom Shape | Absent (0), Unsure/early growth (1), Present (2) |
| Orange Pigment | Absent (0), Unsure/trace clumps (1), Present (2) |
| Large Size | Thickness <1mm (flat) and diameter <3DD (0), Thickness 1 to 2mm ("subtle dome") or diameter 3 to 4DD (1) |
| Enlarging Tumor | None or lesion not documented or mentioned previously (0), Unsure/poor image quality (1), Definite confirmed by subsequent imaging (2) |
| Subretinal Fluid | Absent (0), Trace/minimal and detected only with OCT (1), Definite/seen clinically (2) |
Table 2: Courtesy of Roelofs et al.
Most specialists argue that enlarging tumor size is highly concerning regardless of other features and requires prompt referral. Hence, it is strongly recommended that baseline and annual color fundus photographs are taken to monitor lesions objectively. Baseline OCT through the lesion is also helpful in detecting subtle subretinal fluid and allows for future comparison. When in doubt, referral to an ocular oncologist is never wrong and may save a life.
2. A promising therapy is on the horizon for primary uveal melanoma
Primary treatments for uveal melanoma are irradiation and enucleation. These are highly effective for controlling intraocular tumors. Irradiation with
plaque brachytherapy or proton beam is the treatment of choice for small- and medium-sized tumors, as well as some large tumors. Sequelae of radiation can significantly impair vision; however, this results most commonly from radiation retinopathy or optic neuropathy.
A new globe-sparing treatment that does not involve irradiation has been under exploration.
AU-011 (Belzupacap sarotalocan, Aura Biosciences) is a virus-like drug conjugate that selectively destroys tumor cells upon activation of a near-infrared laser while promoting immune-mediated tumor cell death. Initial studies looking at intravitreal delivery of this agent in indeterminate choroidal melanocytic lesions and small choroidal melanomas have been promising.
In the phase 1b/2 trial results presented in EURETINA 2022, 71 to 86% of patients preserved their visual acuity, and 64 to 70% had local tumor control at 12 months.
Suprachoroidal administration has been shown to achieve higher intratumoral concentration and demonstrated 89 to 100% tumor control and a similarly favorable visual acuity profile at an average of 9 months follow-up in the phase 2 trial presented in Macula Society 2023.
If these findings are corroborated in a larger phase 3 trial and other studies, AU-011 may be the first relatively vision-preserving treatment for patients with indeterminate lesions or small choroidal melanomas.
3. We have an FDA-approved treatment for metastatic uveal melanoma
It is well-documented that approximately 50% of patients with
uveal melanoma develop clinically detectable metastatic disease when the life expectancy drops significantly. Uveal melanoma is distinct from cutaneous melanoma in demonstrating low response rates to immune checkpoint inhibition.
It also has variable response rates to traditional chemotherapeutic agents. These properties were, and continue to be, significant roadblocks to treatment, and there is a large need for new therapies in metastatic disease.
tebentafusp-tebn
In 2021,
tebentafusp-tebn (Kimmtrak, Immunocore Limited) became the first drug to receive Food and Drug Administration (FDA) approval for the treatment of unresectable or metastatic uveal melanoma. It is a bispecific protein that can redirect T-cells to target glycoprotein 100-positive cells in the tumor. In a multicenter, randomized, phase 3 trial, tebentafusp was compared with the investigator’s choice treatment (pembrolizumab, ipilimumab, or dacarbazine) in patients with previously untreated metastatic uveal melanoma.
The study, published in the
New England Journal of Medicine (NEJM), showed that 1-year survival of tebentafusp was significantly higher at 73% compared to the control group at 59%.
5 As expected, treatment-related adverse events were more prevalent in the tebentafusp group, with Grade 3 or 4 severe events occurring in 44% of patients on tebentafusp compared to 17% in the control group.
As glycoprotein 100 is presented by HLA-A*0201, which is highly expressed on uveal melanoma cells, the mechanism relies on HLA-A*02 expression in patients. It is only approved in adults positive for the HLA-A*02:01 allele by blood testing. The FDA has granted
de novo classification to the
SeCore CDx HLA Sequencing System (Thermo Fisher Scientific) used as a companion diagnostic with the medication so that patients can obtain a testing for eligibility assessment.
Figure 1 features a research summary of the phase 3 tebentafusp clinical trial showing an overall survival benefit. Full research summary available and open access in NEJM.
Figure 1: Courtesy of Nathan et al.
IOA-244
More recently, the FDA granted orphan drug designation to
IOA-244 (iOnctura) for treating metastatic uveal melanoma. This is a regulatory T-cell blocking agent that reprograms the immune response to target tumor cells and is administered orally. Interim phase 1 data presented at the American Society for Clinical Oncology 2022 showed that the medication was safe, and the 1-year overall survival rate was 66.7% for the patients in the safety assessment group (9 uveal melanoma patients).
6An additional seven patients were enrolled in the second group of the study, and the 6-month overall survival rate was 100%. Even though studies with a larger patient population and follow-up are necessary, these findings are promising and offer another potential treatment for patients with advanced disease.
4. Topical medications can be used as first-line agents for ocular surface squamous neoplasia
Ocular surface squamous neoplasia (OSSN) is a clinical term that encompasses a spectrum of abnormal conjunctival squamous cell growth, from intraepithelial neoplasia to squamous cell carcinoma. These tumors used to be treated exclusively via surgical excision with wide margins using the “no-touch” technique. However, topical medications are an effective alternative for primary treatment for patients who can demonstrate strong adherence and follow-up.
The three topical agents used for treatment include interferon alpha-2b (IFN), 5-fluorouracil (5-FU), and mitomycin C (MMC). IFN and 5-FU are considered first-line therapies due to their excellent treatment response and favorable side effect profiles.
7 IFN does not require a pause after treatment since it is generally very well-tolerated. Unfortunately, Merck decided to
discontinue its production as of January 2022, and they were the sole supplier of IFN in the United States.
The use of IFN has been limited to inventory availability, and many specialists have been using 5-FU. MMC is a poorly-tolerated medication due to its effects on the ocular surface, from keratoconjunctivitis and corneal epithelial erosions to limbal stem cell deficiency. As such, it requires pauses in treatment and is used as a second-line medication.
It is important to remember that both 5-FU and MMC can be difficult to obtain insurance approval for, so surgical excision may be the most feasible treatment. You can find more information on the medical treatment of OSSN in a recently published
comprehensive review.
75. Consider intraocular lymphoma in the differential diagnosis of anterior uveitis
Intraocular lymphoma compromise rare forms of non-Hodgkin lymphoma that may be primary or secondary. A key subtype of intraocular lymphoma is vitreoretinal lymphoma, which is typically diagnosed in patients after age 50 and is strongly related to central nervous system lymphoma.8 It commonly presents as chronic vitritis that shows an initial response to corticosteroids, followed by rebound inflammation with tapering. Immune status can play a role in the age of presentation, with immunocompromised patients presenting as early as ages 30 to 40.
The diagnosis of
vitreoretinal lymphoma can be challenging, as it is often misdiagnosed as idiopathic uveitis and treated with prolonged courses of corticosteroids. The average time between symptom onset and confirmed diagnosis is approximately 13.9 months.
9 Patients with vitreoretinal lymphoma are typically referred to a retina or uveitis specialist when there is posterior involvement. Still, it is important to note that it can also present as an isolated anterior uveitis. Findings may include keratic precipitates in a floral pattern, a hypopyon, or rarely posterior synechiae.
10 Intraocular lymphoma secondary to a systemic lymphoma may also have similar anterior segment findings.
Patients may present first to their comprehensive ophthalmologist, who may perform the infectious/inflammatory workup and, if it is an
anterior uveitis, may decide to manage them depending on local resources initially. In a patient with uveitis above 50 (or younger if immunocompromised) with a negative infectious and inflammatory workup, lymphoma should be on the differential diagnosis. Prompt referral to a uveitis specialist or ocular oncologist can potentially uncover another systemic lymphoma, and treatment may be lifesaving.
In conclusion
Diagnosis and discussion of ocular cancer are challenging for the patient and the ophthalmologist. Knowledge of the spectrum of disease presentation and risk can help ophthalmologists
identify lesions of concern, guide referral, and better support patients with a new diagnosis. Though treatment is tailored to each patient and should be discussed in detail by the subspecialist, awareness of new treatments helps the ophthalmologist answer preliminary patient questions.
Overall, it is important for comprehensive ophthalmologists to be aware of the broad range of clinical features and potential treatments of ocular tumors and to facilitate evaluation to a subspecialist if there is clinical suspicion.
Prompt diagnosis and referral in these cases do not only save vision and eyes—they can save lives.