Non-clearing vitreous hemorrhage (NCVH) cases can present in various ways with different levels of severity. In some cases, you may know the underlying diagnosis, and the surgery can be fairly straightforward. Other times you may not know what caused the bleeding, and the surgery can be more of a mystery case. No matter the situation, following certain surgical principles can help ensure a good surgical outcome and minimize the risk of a complication.
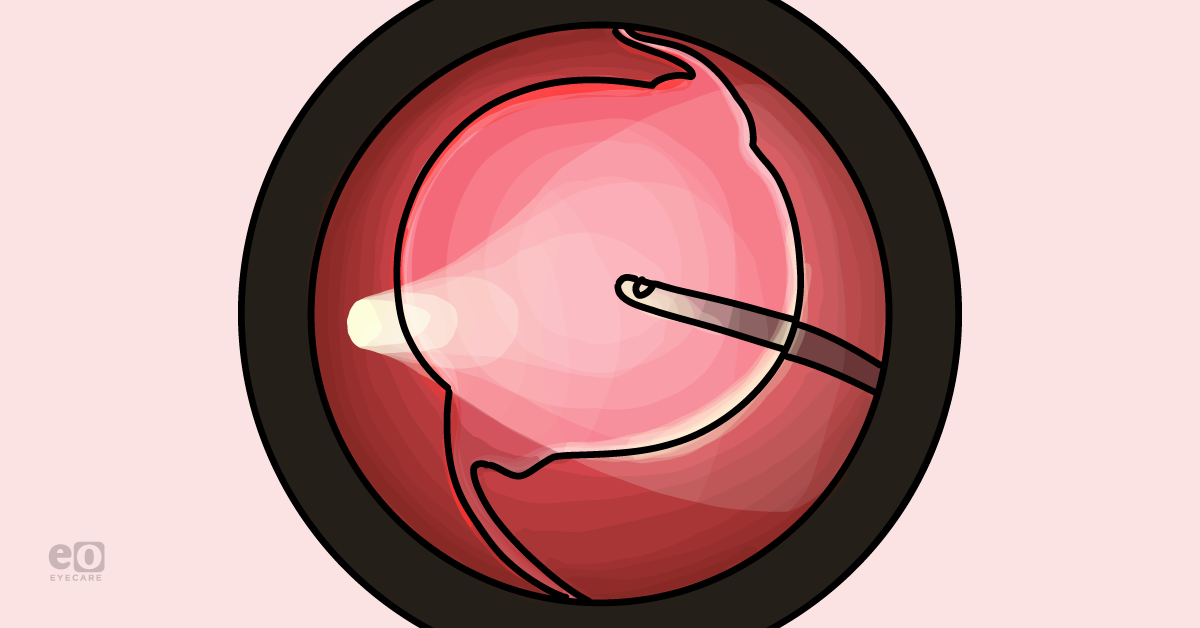
This article will review tips for surgical procedures addressing NCVH and provide videos of anterior and posterior pars plana vitrectomies.
Surgical pearls for NCVH from a branch retinal vein occlusion
Michael Ammar, MD
- Prior to surgery: Be prepared for whatever may be hidden beneath the vitreous hemorrhage. Use all the preoperative information, exams, and imaging available to form an adaptable surgical plan. Try to have everything you may need available in the operating room.
- Vitrectomy: Vitrectomize only in areas of clear visualization. Depending on the degree of blood, visualization can be very poor. Stay where the cutter is illuminated and well-visualized and keep the cutter mouth pointed up towards you. As areas begin to clear, move towards them cautiously. It’s easy to get overzealous and chase the vitreous right into healthy retinal tissue or other structures and cause iatrogenic damage.
- Infusion: Watch the infusion; if the hemorrhage is dense enough, the cannula may not be visible and can be occludable. Also, watch the structural integrity of the globe, and if there is any concern that the infusion is poor or compromised, assess the line and increase the IOP to 60 if needed temporarily. Once the area around the cannula has been vitrectomized, this is typically no longer an issue.
- Shaving: Be very cautious with shaving. It is tempting and natural to want to remove as much blood as possible, but the closer you shave the vitreous base, the higher the risk of an iatrogenic break. A break in this setting can be obscured by blood and may lead to an iatrogenic detachment. This can significantly alter the postoperative course for the patient and potentially require a long-acting tamponade. There is nothing wrong with leaving some of the vitreous skirt behind, as patients will do great. Shave cautiously, and don’t get too aggressive.
- Reassess: When necessary, take a moment to pause and reassess. This is an important rule for any surgery, and it applies to NCVH cases as well. As the view clears, sometimes we see the underlying pathology for the first time. It’s important to take a moment and formulate the best plan for the patient now that new information has revealed itself.
Video of NCVH from a branch retinal vein occlusion
📚
Watch a video of the surgical procedure!
These videos are step-by-step breakdowns of surgeries performed to address NCVH.
Surgical pearls for a pars plana vitrectomy
Eric K. Chin, MD, David RP Almeida, MD, MBA, PhD, Harris Ahmed, DO, MPH
Preoperatively, I always remind patients that
cataract surgery is an expectation and not a complication. Living in an area with mountains and high altitudes, I always bring up the possibility of needing a gas or oil tamponade, even if it is unlikely, based on B-scan ultrasound prior to surgery.
Intravitreal anti-VEGF therapy—while waiting for medical clearance—is a helpful adjunct that can regress culprit abnormal neovascular vessels. Sometimes medical clearance can linger for months, and once in a while, the vitreous hemorrhage will clear with injections.
During the pars plana vitrectomy
Intraoperatively, I have a low threshold for using diluted triamcinolone (50%) after a core vitrectomy is performed to ensure that a complete posterior vitreous detachment (PVD) is present and the hyaloid has been lifted and/or removed with the cutter. This will also aid in shaving the vitreous base.
Ensure that the panretinal photocoagulation (PRP) laser is complete— I like to surround the nerve and macula and extend the PRP laser to the ora with the aid of scleral depression.
Hemostasis from oozing neovascular vessels can be controlled by temporarily elevating the IOP or using an endo-diathermy probe to cauterize abnormal vessels.
After the pars plana vitrectomy
Post-operatively, it is not uncommon to have mild residual red blood cells lingering in the vitreous cavity. This can sometimes take a few weeks to resolve and reabsorb in a fluid-filled vitrectomized eye.
In cases where residual or recurrent vitreous hemorrhage lingers, I have a low threshold to reinject with monthly
anti-VEGF therapy. Sometimes oozing can arise from neovascularization at the disc after the peeling of membranes, and there’s no better way to stop additional bleeding than with anti-VEGF therapy, in my opinion.
Vitrectomy tips for diabetic NCVH
The following video represents a straightforward case of pars plana vitrectomy for a non-clearing diabetic vitreous hemorrhage. When the vitreous hemorrhage is diffuse with poor vision, I often offer and discuss the option of surgery/vitrectomy to accelerate the potential improvement in vision. With the improved safety and efficiency of vitrectomy surgery, it is a valuable and viable option for many patients with baseline poor vision or chronic vision loss.
Video of pars plana vitrectomy
📚
Watch a video of the surgical procedure!
These videos are step-by-step breakdowns of surgeries performed to address NCVH.