Constant innovations in technology and pharmacology mean ophthalmologists must consistently educate themselves on the latest offerings. Biosimilars are becoming a part of the treatment landscape.
Therefore, it is important to understand exactly what biosimilars are, how they are being labeled for use, safety considerations, and what the future may hold.
First, let’s look at biologics
Biologics therapies have begun to revolutionize the treatment of diseases across various medical fields and are now beginning to enter the field of ophthalmology. As such, it is important to obtain a new level of knowledge on the impact they could have on the ever-changing landscape of ophthalmology.
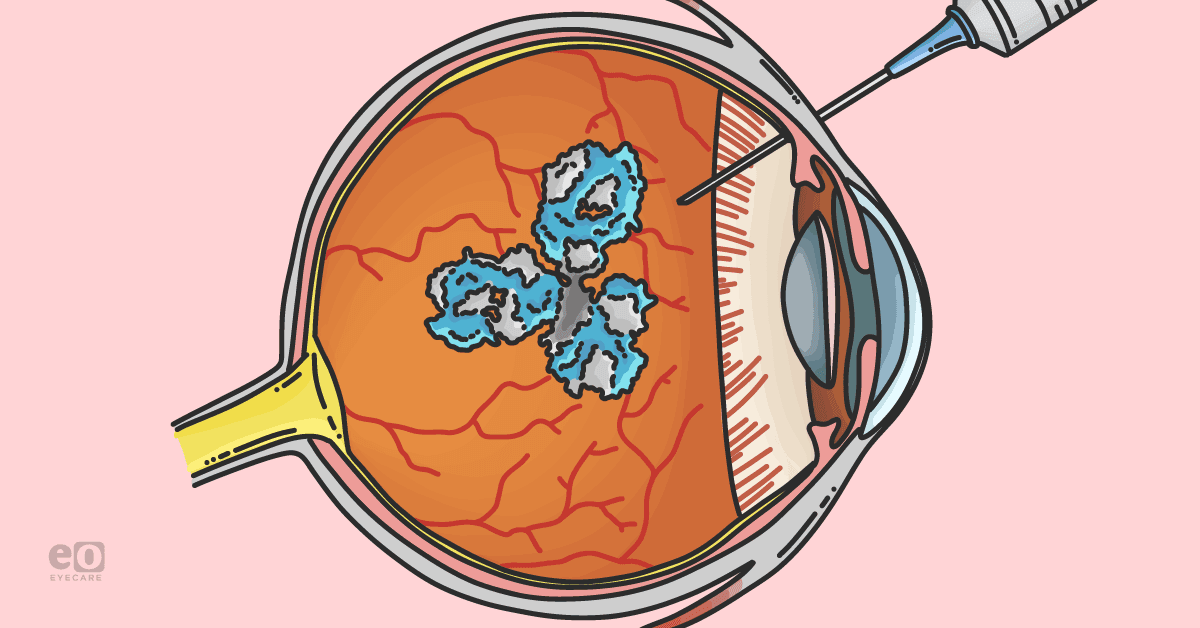
Biologics have been in the pharmaceutical industry for years, first beginning with the use of recombinant insulin. A biologic is a complex molecule created to be structurally and functionally similar to molecules produced by our bodies (shown in Figure 1).1
These companies were then able to patent the product, which resulted in increased costs for patients. Once the patent expires, biosimilars can be formulated from their innovator biologic.
Figure 1 illustrates how biosimilar products differ from reference products.
Figure 1: Courtesy of the American Academy of Ophthalmology.
What exactly are biosimilars?
Biosimilars can be compared to generic drugs; however, their production is much more costly and time-consuming. In the production of biosimilars, every batch must be molecularly tested to be structurally and functionally equivalent to the biotherapeutic.2 This production is less costly than its preexisting biologic counterpart but still provides the same safety and efficacy.
The US Food and Drug Administration (FDA) approval process for biosimilars states, “A biosimilar is highly similar to, and has no clinically meaningful differences in, safety, purity, and potency (safety and effectiveness) from an existing FDA-approved reference product. The goal of a biosimilar development program is to demonstrate the similarity between the proposed biosimilar product and the reference product, not to establish the safety and effectiveness of the proposed product independently.”3
The first biosimilar approved in the US was filgrastim in 2016.3 Since then, over 30 biosimilars have been approved by the FDA.4
Tables 1 and 2 highlight retinal biosimilars that have been approved and are in development, respectively.5
| FDA-Approved | |
|---|---|
| Name | Company |
| Byooviz (ranibizumab biosimilar) | Samsung/Bioepis |
| Cimerli (ranibizumab biosimilar) | Coherus |
Table 1: Courtesy of Jennifer Lim, MD, FARVO, FASRS.
| In development | |
|---|---|
| Name | Company |
| Ranibizumab biosimilars | |
| Xlucane | Xbrane, Sweden; Phase III |
| R-TPR-024 | Reliance Life Sciences, India; Phase III |
| SJP-0133 | Senju Pharmaceuticals, Japan: Phase III |
| LUBT010 | Lupin, India; Phase III |
| CKD-701 | Chong Kun Dang Pharmaceutical, South Korea; Phase III |
| Aflibercept biosimilars | |
| SB15 | Samsung Bioepis |
| MYL1701 | Momenta Pharma and Viatris |
| ABP-938 | Amgen, United States |
| FYB203 | Formyon AG/Bioeq. Germany; Phase III nAMD |
| S0K583A19 | Sandoz, Switzerland; Phase III nAMD |
| CT-P42 | Celltrion, South Korea; Phase III nAMD |
| ALT-L9 | Alteogen, South Korea; Phase I AMD |
| 0T-702 | Ocumension Therapeutics/Shandong Boan Biological Technology, China; Phase III |
| Bevacizumab biosimilar | |
| Bevacizumab-vikg (Lytenava) | 0NS-5010, Outlook Therapeutics, Phase III |
Table 2: Courtesy of Jennifer Lim, MD, FARVO, FASRS.
Biosimilars' emerging role in the treatment of retinal disease
Biosimilars' role in the treatment of neovascular retinal disease has vastly grown throughout the years. Anti-vascular endothelial growth factor (VEGF) biosimilars have broken onto the scene as a possible alternative agent to other treatments, such as laser ablation therapy and photodynamic therapy. The most common drugs used today are ranibizumab and bevacizumab, approved in 2022; however, bevacizumab is being used as an off-label product for neovascular retinal disease.6
Biosimilars have been explored as treatment agents for retinal diseases, such as wet macular degeneration and diabetic macular edema, due to their effects on vascular endothelial growth factors. VEGF plays an important role in these two diseases as it is the potent factor causing neoangiogenesis.7
Studies performed in 1994 showed that retinal hypoxia caused elevated levels of VEGF mRNA, leading to indications of its role in neovascularization. The following studies showed increased levels of VEGF in the ocular fluid of individuals with neovascular ocular disease as opposed to those without new vessel growth. These studies were crucial in indicating the role of VEGF in neovascularization and providing a target for treatments.8 Neovascularization in wet age-related macular degeneration (AMD) provided a therapeutic role for biologics.
In wet AMD, the increased formation of new blood vessels on the retinal pigment epithelium leads to central vision loss. VEGF plays a major role in driving the formation of new blood vessels forming below or through, via breaks in Bunch Membrane, the retinal pigment epithelium. Therefore, the role of anti-VEGF biologics results in decreased progression of neovascularization, helping to preserve vision.7
Significant studies on biosimilars in neovascular disease
Two pivot studies, MARINA and ANCHOR, allowed for the FDA approval of ranibizumab for wet AMD treatment. Both studies found improvements in vision loss and mean visual acuity through 2 years and demonstrated minimal adverse events.9,10
In a more recent retrospective study performed in 2020, Sharma et al. found similar results, such as improved visual acuity, decreased central subfield thickness, and reductions in intraretinal and subretinal fluid. They also concluded no new safety concerns with the injection of ranibizumab as intraocular pressure increases were minimal from baseline to 48 weeks.11
Further, in the CESAR study from 2021, researchers tested the safety and efficacy of ranibizumab in India and similar results to previous studies. They saw similar efficacy and safety to the original biologic drug. For the safety profile, out of 126 participants, they had 12 complaints (12.7%) of an adverse effect, most involving ocular complaints of increased intraocular pressure.12
Additionally, they had complaints of iridocyclitis, corneal edema, ocular hyperemia, and dry eye comparable to the innovator biologic ranibizumab of less than 1% of patients. Immunogenicity was also tested, showing 7.94% patients before treatment and 7.14% patients after biosimilar ranibizumab treatment, comparable to the innovator drug, indicating no increase in anti-ranibizumab antibodies suggesting immunogenicity. The overall study concluded the biosimilar was just as effective and safe as its innovatory biologic drug.12
How are biosimilars reviewed and regulated?
Even with studies providing evidence for safety, there are still some significant concerns about whether the safety is truly equivalent to biologics. As the production and approval process is significantly shorter, there are growing concerns over the regulation and quality of products.
Additionally, there are no set guidelines worldwide for the approval process, making many feel unsure of whether they are doing the best for their patients. As previously discussed, biologics require large efficacy studies; however, the regulations on what studies biologics require are more fluid in nature and performed in an abbreviated fashion.
The FDA is open to looking at different target data when reviewing biosimilars. They want to answer the question, “Are there clinically meaningful differences between the products?—and look across the spectrum of different scientific studies, whether in the analytical space, looking at functional data or pharmacodynamic endpoints, versus those traditional clinical endpoints.”13
With continued pushes towards biosimilars without hard-set guidelines on the approval process, many ophthalmologists are wary of the safety and efficacy profiles of these drugs.
Ranibizumab for diabetic retinopathy and diabetic macular edema
VEGF’s role in diabetic retinopathy and diabetic macular edema (DME) has additionally made biosimilars an attractive therapy for these patients. DME pathophysiology makes the effect of anti-VEGF unclear. Two forms of edema occur in this process, one being extracellular with inflammatory cytokines resulting in vasogenic edema and the expression of VEGF. Additionally, edema on the intracellular side resulting from arterial occlusion leads to another form without the effects of VEGF.14
This is one of the reasons that studies have found conflicting results with the use of biosimilars for a full treatment of DME. A 2-year study performed in 2012, found that after 6 months, there was a significant improvement in vision in the biosimilar group compared to the biosimilar plus steroid group and the macular laser photocoagulation group. However, at the end of 24 months, there was no significant difference seen, thus indicating that the benefit of the biosimilar does not sustain its effectiveness long-term.15
Findings from the RESTORE study on biosimilars and DME
Further studies have demonstrated that biosimilars are effective in treating DME. The RESTORE study performed in 2010 separated participants as those treated with ranibizumab monotherapy, ranibizumab plus sham laser, ranibizumab plus laser, or sham injections plus laser.
The results found that ranibizumab monotherapy and laser combination had a significant increase in visual acuity as compared to those with just laser (seen in Figure 2). This indicated that even if VEGF is not the sole factor in diabetic macular edema, using biosimilars helps improve visual acuity in patients.16
Figure 2 highlights the RESTORE study results comparing ranibizumab monotherapy and laser combination to treat diabetic macular edema.
Figure 2: Courtesy of Mitchell et al.
Further studies on biosimilars in the treatment of DME
An additional study known as RESOLVE showed similar efficacy with the use of ranibizumab, reporting a mean difference in central retinal thickness of 194.2 ± 135.1μm with ranibizumab compared to 48.4 ± 53.4μm with the control (P < 0.0001). Findings resulted in a significant improvement in best-corrected visual acuity.17
As mentioned earlier, in the CESAR study, they looked at the safety and clinical efficacy of ranibizumab. Their findings indicated visual acuity improved as early as the first month and maintained through 3 months and showed no incidence of increased intraocular pressure greater than 20 after injections. They additionally also found a reduction in the central fovea thickness from baseline after both 1 and 3 months.12 These findings further demonstrated the safety and effectiveness of biosimilars in the treatment of DME found in both the RESTORE and RESOLVE clinical trials.
The aforementioned LUMINOUS study found that in the US, when patients had a co-pay, it decreased the odds of a patient receiving anti-VEGF shots by 40% and also decreased follow-up appointments by 37%. These socioeconomic factors are still major factors regarding patients having access to biosimilars. The price will significantly be reduced for patients, but they may still struggle with access to care and their health insurance coverage.6,19
Conclusions
The use of biosimilars raises concerns regarding their effectiveness and safety, which must be addressed before their expanded use in various fields of medicine. While biosimilars may offer more affordable treatment options for patients, there are uncertainties surrounding their use.
Further education is necessary to understand the potential risks and benefits of these drugs and their approval process. More evidence is required to determine the safety and efficacy of biosimilars before their role in ophthalmology can be clearly defined. It is important to approach biosimilars with caution and a comprehensive understanding of their potential impact on patients.