Herpes zoster (HZ) is the reactivation of the varicella-zoster virus. This is the virus that causes the highly contagious chickenpox.
In the United States, 99.5% of adults over the age of 40 have been
infected with varicella.
1 After the acute infection, the virus remains dormant in the dorsal root ganglia (illustrated below).
Overview of herpes zoster
Varicella zoster can reactivate later in life, causing a rash that can be painful in various areas of the body. This is herpes zoster, also known as
Shingles. Only people who were previously infected with varicella or have had the varicella vaccine, can develop shingles.
Each year, there are approximately one million new cases of herpes zoster in the United States.1 A person's risk for herpes zoster increases after the age of 50. Those who experience herpes zoster typically only have one episode in their life. However, multiple episodes are possible, especially in patients who are immunocompromised.
Figure 1 shows how the varicella virus remains dormant in the dorsal root ganglion.
Figure 1: Courtesy of Evan Canellos, OD, FAAO.
How does the herpes zoster virus reactivate?
As a person ages, their immune system functions less efficiently. Additionally, medical conditions and medications: human immunodeficiency (HIV),
chemotherapy, malignancies, and immunosuppressive therapy can all contribute to an immunosuppressed state.
Finally, psychological/emotional stress can affect immune function and increase susceptibility to infection.
Is herpes zoster contagious?
People who have not had varicella or never received the varicella vaccine can get infected with the varicella-zoster virus from someone with active herpes zoster. The virus is spread by direct contact, and the lesions are no longer contagious once they have become crusted and dry.
Clinical manifestations of herpes zoster
HZ manifests as a painful vesicular dermatitis localized to a dermatome supplied by a spinal or cranial sensory ganglion. It is typically unilateral and respects the body’s midline. The most common dermatomes are: T3-L3 and V (trigeminal). Although uncommon, severe pain without a vesicular eruption, known as
zoster sine herpete, can occur.
2 There are three phases of clinical manifestations: pre-eruptive, acute eruptive, and post-herpetic neuralgia.
Table 1 outlines the key features of each phase of clinical manifestation of herpes zoster.
| Phase 1: Pre-eruptive | Phase 2: Acute Eruptive | Phase 3: Post-Herpetic Neuralgia |
|---|
| Sensory phenomena involving 1 or more dermatomes. | Patchy erythema. Blister-like vesicles which rupture and eventually become dry and crusty. Regional lymphadenopathy. | Persistent pain lasting 30 or more days after lesions have crusted. |
| Duration: 1 to 10 days (avg. 48 hours). Symptoms: Burning, throbbing pain, itching, pins and needles, tingling, or numbness. Malaise, photophobia, headache. Possible fever. | Healing can take 10 to 14 days, complete resolution may take up to a month. Skin scarring is not typical, but possible. | Pain typically confined to the area of original dermatome. Pain can be mild and short-term to severe, debilitating and long-term. |
Potential systemic complications of a herpes zoster infection
Herpes zoster infections can potentially spread to other nerve ganglions or through the bloodstream, which can cause various systemic complications.
Systemic complications associated with herpes zoster infections include:
- Aseptic meningitis
- Encephalitis
- Bacterial superinfection
- Bell’s Palsy
- Hearing impairment
- Motor neuropathies
- Ramsay Hunt Syndrome
- Transverse myelitis
- Vasculopathy/vasculitis and stroke
- Genitourinary complications
Herpes zoster ophthalmicus (HZO)
Herpes zoster ophthalmicus (HZO) occurs along the dermatome of the ophthalmic division of the trigeminal nerve (V) which provides sensory innervation to the face. It is divided into 3 main branches: V1 ophthalmic, V2 maxillary, and V3 mandibular (shown in Figure 2). Further, the ophthalmic division contains 3 branches: frontal, lacrimal, and nasociliary branches.
Figure 2 highlights dermatomes of the trigeminal nerve.
Figure 2: Courtesy of Evan Canellos, OD, FAAO.
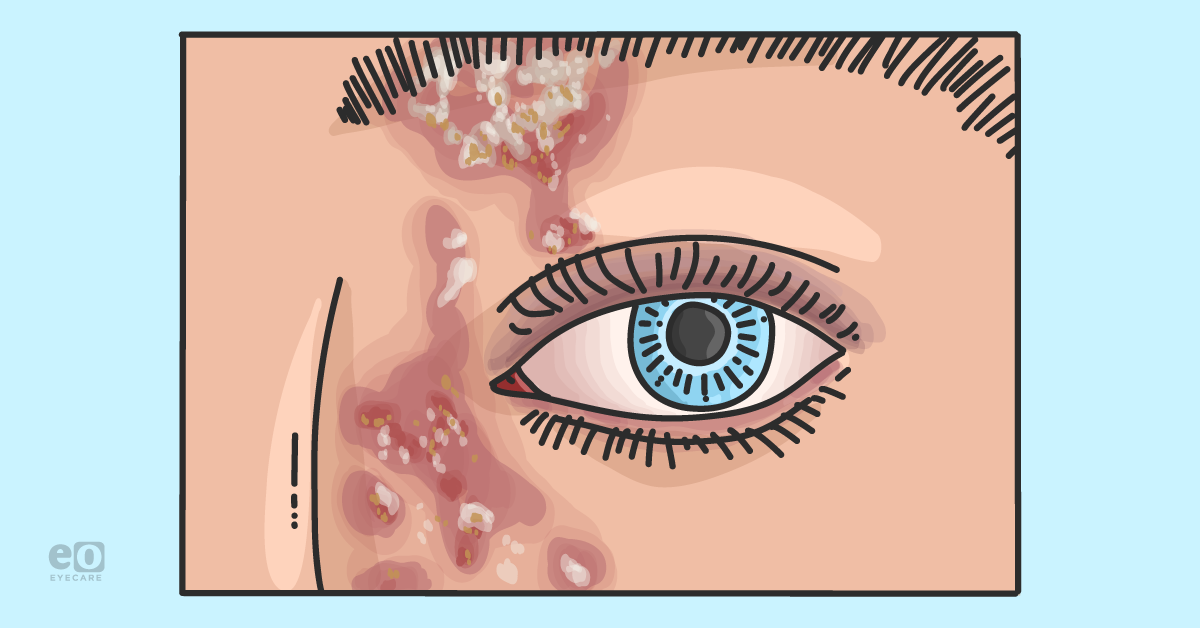
Involvement of the tip or side of the nose, Hutchinson’s sign, is considered a clinical predictor of ocular involvement (shown in Figure 3). However, up to ⅓ of patients without the sign develop ocular manifestations. HZO represents up to 25% of all cases of herpes zoster.4
Figure 3 illustrates a patient with HZO and visible vesicular rash and Hutchinson’s sign.
Figure 3: Courtesy of Evan Canellos, OD, FAAO.
Ocular manifestations of HZO
The most common ocular manifestations are eyelid involvement,
conjunctivitis, keratitis, and uveitis. However, HZO can affect any part of the eye. As a result, it is necessary to evaluate each patient carefully, including a dilated fundus examination.
It is important to note that the ocular signs may be delayed from the onset of the vesicular rash. The first follow-up for these patients could be 1 to 7 days depending on clinical circumstances.
Table 2 lists ocular symptoms associated with herpes zoster ophthalmicus.
| Area | Ocular Symptoms |
|---|
| Lids/conjunctiva | Blepharitis, lid edema, lid scarring, lash loss, trichiasis, and cicatricial entropion, puncta and canaliculi scarring, conjunctivitis, episcleritis, and scleritis. |
| Cornea | Dendritic-like epithelial keratitis (pseudo dendrite), elevated mucoid plaques, nummular subepithelial/anterior stromal infiltrates, stromal edema, disciform edema, endotheliitis, bullous keratopathy, lipid keratopathy, serpiginous ulceration and perforation, and neovascularization. |
| Iris/anterior chamber/IOP | Uveitis, hypopyon, trabeculitis, anterior and posterior synechiae, patchy sector iris atrophy, and glaucoma. |
| Optic nerve head/retina | Retinitis and choroiditis: Acute retinal necrosis (immunocompetent patients) and peripheral outer retinal necrosis (immunocompromised patients); optic neuropathy, and occlusive arteritis. |
| Neuro-ophthalmic | Cranial nerve palsies (III, IV, VI) and pupil abnormalities (light near dissociation). |
Potential long-term ocular sequelae of HZO
Severe dry eye, corneal scarring, and recurrent or smoldering
uveitis are the most common long-term manifestations. Herpetic infection can also cause impaired corneal nerve function and reduced corneal sensation leading to
neurotrophic keratitis.
There are different ways to test corneal sensitivity, such as a fine wisp of a cotton-tip applicator, non-flavored dental floss, or the Cochet-Bonnet esthesiometer. Herpetic eye disease is a leading cause of neurotrophic keratitis.
Finally, post-herpetic neuralgia occurs in up to 30% of patients with HZO.4 The associated pain can persist for weeks, months, or years.
Treatment options for HZO
It is beneficial to start oral antiviral therapy within 72 hours of onset of skin lesions.5 This reduces viral shedding and decreases systemic dissemination of the virus. It may reduce the severity of ocular complications and the severity and duration of acute neuralgia. Treatment with oral corticosteroids is controversial and shows no definitive benefit.
Oral antiviral options to treat herpes zoster:
- Acyclovir 800mg 5x/day for 7 to 10 days
- Valacyclovir 1g TID for 7 to 10 days
- Famciclovir 500mg TID for 7 to 10 days
Table 3 outlines treatment options, in addition to the oral antiviral therapy, for the various complications of a herpes zoster infection.6
| Complication of HZO | Treatment |
|---|
| Eyelid | Topical antibiotics to avoid secondary infection, topical steroid cream. |
| Keratitis | Punctate keratitis: preservative-free lubrication, antibiotic ointment. Corneal pseudo-dendrite: in general, adding a topical antiviral is not beneficial, the oral antiviral is sufficient. Immunocompromised patients may need more aggressive treatment. Stromal, endothelial keratitis and uveitis: topical corticosteroids based on degree of anterior chamber inflammation and corneal edema. A long taper is essential. |
| Neurotrophic keratitis | Preservative-free lubrication, punctal occlusion, amniotic membranes or drop derivatives, autologous serum, therapeutic contact lenses, and Oxervate (cenegermin-bkbj): a recombinant form of human nerve growth factor, ophthalmic solution. Surgical considerations for significant ulcerations: tarsorrhaphy, conjunctival flap, or penetrating keratoplasty. Potential for corneal neurotization. |
| Viral retinitis and choroiditis | Same day retina referral, diagnostic PCR testing with anterior chamber or vitreous Tap. Patients are empirically treated with intravitreal antivirals and IV or oral antivirals, typically double the Zoster oral dose. |
| Post-herpetic neuralgia (PHN) | Co-manage these patients with their primary care provider or pain management specialist. Treat with Capsaicin 0.25% cream BID, topical lidocaine patch, gabapentin, pregabalin, tricyclic antidepressants (amitriptyline), and oxycodone. |
The herpes zoster vaccine
The CDC recommends healthy adults aged 50 and over get vaccinated. The
SHINGRIX vaccine contains an inactivated form of the varicella-zoster virus. In addition to providing protection against Shingles, it may also reduce risk of post-herpetic neuralgia. It is 90% effective with 2 intramuscular doses 2 to 6 months apart and effective for at least 7 to 10 years.
7New clinical study on herpes zoster ophthalmicus: ZEDS
The
Herpes Zoster Eye Disease Study (ZEDS) is an ongoing NYU-sponsored, multi-center, randomized, placebo-controlled clinical trial that started in 2017 and is estimated to be completed in 2024.
Its objective is to determine whether a 12-month daily treatment with 1000mg of valacyclovir reduces the ophthalmic complications of HZO.7 Their second aim is to evaluate whether this same treatment reduces the severity and duration of postherpetic neuralgia.8
Case report of a patient with HZO
A 50-year-old Asian male was referred to our clinic by his dermatologist for a same-day consult for corneal evaluation. His dermatologist had diagnosed him with herpes zoster ophthalmicus. The patient had reported a tingling sensation and pain along the left forehead a week prior to presentation. His skin lesions appeared 48 hours prior to his dermatology appointment.
His eye was
hyperemic, but he denied pain or photophobia. The patient self-reported being under “tremendous stress” recently. His review of systems was unremarkable, and he reported using Chinese herbal ointment over his lesions. His entering correct acuity was OD 20/30 OS 20/40 with unremarkable pupil evaluation and full extraocular motilities.
An external exam revealed vesicles and erythema on his left forehead, respecting the midline (shown in Figure 4). He had erythema on the bridge of his nose, but there was no erythema or vesicles on the apex of his nose.
His slit lamp exam was positive for left upper eyelid edema and periorbital vesicular eruptions. His cornea was clear without staining, but he did have a grade 2+ conjunctiva injection OS with a deep and quiet anterior chamber. His iris was flat, and his dilated fundus examination revealed: no vitreous cells; his optic nerves were sharp and distinct; and his retinal vascular, macula, and peripheral retina were flat and intact. His right eye was unremarkable.
He was prescribed Valtrex 1 gram TID po for 10 days and triamcinolone ointment TID (prescribed by his dermatologist) to be applied to his skin lesions. We added
preservative-free artificial tears, educated the patient on his current findings, and scheduled him for a 1-week follow-up with us.
Figure 4 is a clinical image of the patient with herpes zoster ophthalmicus.
Figure 4: Courtesy of Harriette Canellos, OD, FAAO.
Follow-up care for the patient
Interestingly, our patient did not show up for his follow-up exam. When we contacted his home, his wife reported that her husband became confused, his memory was deteriorating, and he had developed photophobia and phonophobia. He was immediately admitted to a local hospital.
Ultimately, our patient was diagnosed with aseptic meningitis and treated with IV acyclovir for 14 days. On hospital discharge, his mental status returned to baseline. On follow-up in our clinic, his conjunctival hyperemia resolved without ever developing additional ophthalmic sequelae.
Final thoughts on herpes zoster ophthalmicus
Herpes zoster ophthalmicus is a serious disease with the potential for grave complications. This case highlights a patient who presented initially with mild ocular findings but eventually developed a serious neurologic condition that his past medical history would not have predicted. Early detection, proper treatment, and follow-up are critical factors in patient outcomes.
We should also be aware of potential relapses in older or immunocompromised patients. Extending antiviral therapy and appropriate steroid taper (when prescribed) may be necessary to avoid relapses.
Co-management is necessary to monitor for systemic complications and management of post-herpetic neuralgia.