Surgeons should also know their own surgical limitations and refer to a more experienced surgeon if necessary.
1-5 Complex cataract cases require vigilance at all stages; surgeons must recognize and anticipate challenges preoperatively, and ensure they have the correct tools in the OR to help manage issues that may arise.
1-5 Having a plan and a back-up plan helps the surgeon stay focused and use appropriate techniques to improve surgical success.
This article focuses on key exam findings and diagnoses that can tip a surgeon off for a possible complex case—and how to adequately prepare!
Basic anatomical considerations
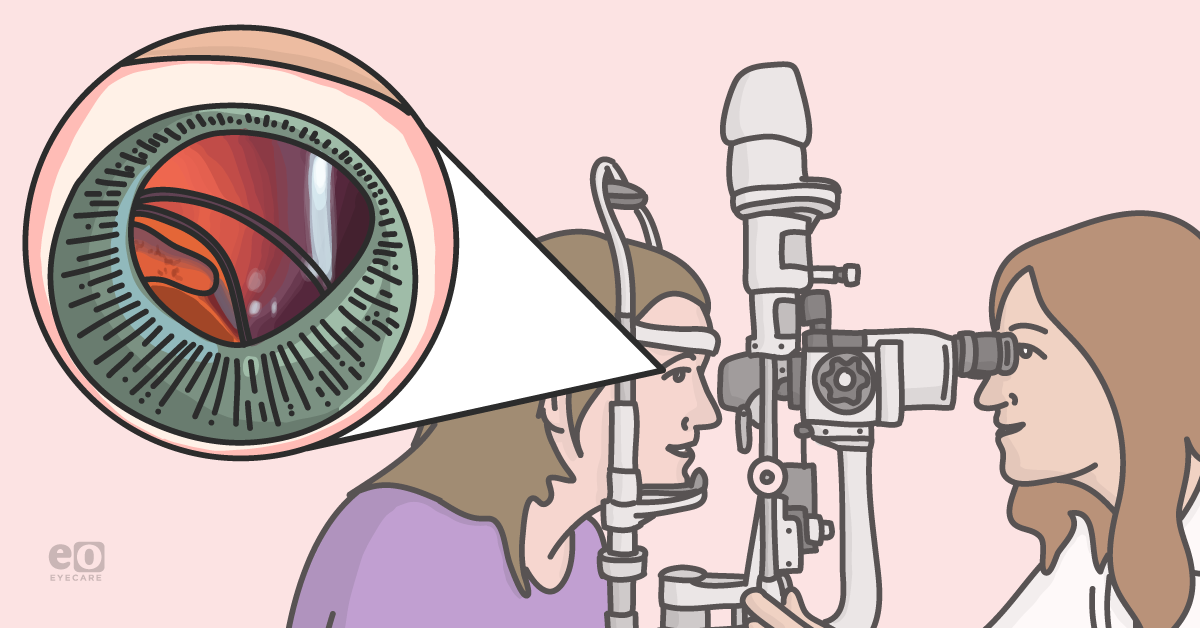
Success in any field of surgery depends on a comprehensive, in-depth understanding of anatomy. Understanding the nuances of your operative target (in this case, the crystalline lens) will help you prepare for anatomy anomalies, whether congenital or environmental (e.g., traumatic) in nature. The normal crystalline lens is suspended in its natural position by zonular fibers from the ciliary body.3-5 The lens has a capsule (anterior and posterior), epithelium, cortex, and nucleus.3-5
Straight-forward phacoemulsification-based cataract surgery depends on an uncompromised, centered crystalline lens as well as intact and strong zonules.3-5 Violation of the lens capsule and lens dislocation as well as weakness or loss of zonules can lead to a complex surgery—and even the need for additional surgeries.
Top tools to keep in your cataract surgery toolbox
When evaluating a patient for cataract surgery, there are several entities that may tip you off regarding a possible complex case. These include: pseudoexfoliation syndrome, history of trauma, lens abnormalities, zonular abnormalities or loss, poor dilation (small pupils), extremely long or short eyes as well as very dense brunescent and white intumescent cataracts.1-5 The following is a list of items to have available to you in the OR to help make these complex cases more manageable:
Viscoelastic
This gel can be used to help shield the corneal endothelium from excess ultrasound energy and prevent wound burns.5-7 It can also be used to viscodissect the lens nucleus in cases of posterior polar cataract, and push back vitreous from presenting in the case of a posterior capsular tear.5-10
Anterior vitrectomy
This may be needed in case of posterior capsular rupture, or zonular loss.1,7,11,12 Presence of vitreous can make cataract surgery difficult and removal of nuclear pieces inefficient (and in some cases impossible). In addition, a vitrector should be used to cut vitreous, as an aspiration probe can induce vitreous traction, and subsequent risk of retinal tear and detachment.1,7,11,12
Trypan blue
This dye aids in improving visualization of the anterior capsule during cataract surgery—especially those with a decreased red reflex (very dense or white cataracts as well as eyes with retinal disease).1,13,14
30-Gauge needle on an air syringe
This may be helpful to decompress an intumescent cataract prior to capsulorhexis creation to avoid anterior capsular run-out.14
Triamcinolone intraocular steroid
This can be injected into the anterior chamber during anterior vitrectomy, or used to determine if there is presence of vitreous, as it stains the vitreous white.11 This highlights the areas where vitreous is presenting, which can be especially helpful to identify if going to a wound, or causing tilt or a shift in an IOL.11
Capsular tension hooks
The presence of zonular weakness increases the risk of intraoperative complications and therefore capsular support devices are important management tools for eyes with zonulopathy.15-18 They facilitate safe and successful cataract surgery by improving capsular bag stability and centration.
Capsular tension rings/segments
Capsular tension rings and segments increase the chance of capsular bag placement of an intraocular lens (IOL).1,15-18 Rings and segments exert an outward force that redistributes tension from areas of intact zonules to strengthen areas of weak or missing zonules. 1,7,15-18 A standard capsular tension ring may not be adequate for eyes with advanced zonular weakness—eyes with >4 clock hours of zonular loss or progressive zonulopathy may require endocapsular segments that can be scleral-fixated.1,7,15-18
Pupillary expansion devices
Non-dilating or poorly dilating pupils pose challenges during cataract surgery due to reduced surgical space, small capsulorhexis, difficulty maneuvering the lens during surgery as well as risk of anterior or posterior capsular tear.
1,15,17 When pharmaceutical dilation is not adequate, mechanical dilation of the pupil may be employed using iris hooks or pupil expansion rings (e.g., Hydroview Iris Protector Ring (Grieshaber &Co, AG Schaffhausen, Schaffhausen, Switzerland, Seipser iDeal iris ring (Eagle Vision, Memphis Tennessee USA),
Malyugin Ring (Microsurgical Technology/MST Inc, Redmond, Washington USA)).
1,15,17Back-up IOLs
In cases of posterior capsular rupture or unstable zonules, it may not be possible to insert a single-piece IOL in the capsular bag.1-5 When this occurs, it is important to have back-up IOL’s on hand, including 3-piece IOL’s that can be placed in the ciliary sulcus, sutured to the iris, or scleral fixated as well as anterior chamber IOLs (ACIOL), if necessary.
Common patient risk factors for complex cataract surgery
Pseudoexfoliation syndrome
Pseudoexfoliation syndrome (PEX) is a systemic syndrome that targets mainly ocular tissues though gradual deposition of fibrillary white, flaky material onto the lens capsule, ciliary body, zonules, corneal endothelium, iris and pupillary margin—these deposits may also been found elsewhere in the body, including skin, heart, lungs, liver, and kidneys.1,10,12 PEX may be bilateral and asymmetric; it is more prevalent in older age (<70 years old) and those of Scandinavian descent.1,10,12
Precautions must be taken here during cataract surgery due to possible zonular instability, loss or dialysis, poor pupillary dilation, and phacodonesis.1,10,12 Therefore, these patients may be at higher risk of intraoperative complications and will require specific instrumentation available in the OR, should cataract surgery become complex and require capsular support, anterior vitrectomy, or use of a 3-piece or ACIOL.
Figure 1 demonstrates a dislocated IOL due to advanced pseudoexfoliation.
Figure 1. Photo courtesy of Eric Rosenberg, DO MSE
Blunt ocular trauma
Trauma can affect the lens in several ways; it may result in subluxation or dislocation.1,2,7 Traumatic cataracts can also be intumescent in nature, but their type and clinical course depend on the trauma mechanism and capsular bag integrity.1,2,7 If the anterior capsule is not intact, microscissors may be used to create a controlled rhexis—trypan blue is also helpful here to aid in visualization.1,2,7,13 Zonulopathy and zonular weakness may also be present, therefore, care must be taken to be gentle with the capsule; capsular support devices may be required.
Figure 2 shows a traumatic cataract with iridodialysis.
Figure 2. Photo courtesy of Eric Rosenberg, DO MSE
Penetrating ocular trauma
In the cases of acute traumatic cataract due to penetrating trauma, care must be directed towards stabilizing and closing the globe.
1,2,7,13 Other penetrating and external ocular injuries must be ruled out and addressed. Ensuring the patient is stable prior to surgery is necessary as well. Closure of all
open globe injuries should be prioritized first; cataract removal may need to wait until the globe is stabilized in order to prevent inadvertent damage to internal ocular structures.
In addition, a lacerated or traumatized globe compromises IOL calculations—if the surgeon wishes to emergently place an IOL at the time of globe repair, they may base calculations on the opposite eye’s measurements.1,2,7,13 It should be made clear to the patient that IOL calculations here are an estimate, and primary focus is on repair and reconstruction of the globe–as well as saving vision.1,2,7,13
Figure 3 demonstrates an eye post-repair of penetrating trauma with a subluxated crystalline lens.
Figure 3. Photo courtesy of Eric Rosenberg, DO MSE
Zonulopathy
Loose or missing zonules may be a result of prior trauma, coloboma, and pseudoexfoliation.1,2,4,5,7,10,18,19 Sometimes, tapping the slit lamp at time of preoperative exam can demonstrate phacodonesis.1,2,4,5,7,10,18,19 Examining the patient lying flat may also show a tilting of the crystalline lens; occult zonular loss may be visible with good dilation.1,2,4,5,7,10,18,19 In these cases, the surgeon should be prepared to perform anterior vitrectomy, use capsular support devices (hooks, rings, segments, if necessary), and inform the patient that it may not be possible to place an IOL at time of surgery if removal of the cataract is especially difficult. 1,2,4,5,7,10,18,19
Figure 4 demonstrates a subluxated crystalline lens due to zonulopathy from Marfans syndrome.
Figure 4. Photo courtesy of Eric Rosenberg, DO MSE
Lens abnormalities (spherophakia, coloboma, posterior polar cataract)
Cataract surgery in patients with lenticular abnormalities can pose specific concerns, especially for zonulopathy and difficult cataract removal. 1,2,4,5,7,10,18,19 Specifically, these entities may include, spherophakia, coloboma, and Marfan’s syndrome.1,2,4,5,7,10,18,19 I treat all of these patients as complex cases, as they are at high risk (or guaranteed risk) of zonular loss/weakness, requiring capsular tension support devices.
These patients need to be informed that due to abnormal anatomy, IOL placement at time of initial cataract surgery may not be possible; and that further surgery, including vitrectomy, may be required.1,2,4,5,7,10,18,19 In general, these eyes must be handled with great caution due to the increased risk of retinal detachment, and association of maculopathy.1,2,4,5,7,10,18,19
Figure 5 demonstrates a lens with microspherophakia that has dislocated into the anterior chamber.
Figure 5. Photo courtesy of Eric Rosenberg, DO MSE
Figure 6 demonstrates an eye with coloboma of the iris and lens.
Figure 6. Photo courtesy of Eric Rosenberg, DO MSE
Posterior polar cataracts are unique, as they pose a significant risk of posterior capsular break and therefore risk of vitrectomy (up to 36%) at the time of surgery. 1,2,8,9 This is due in part to possible adherence of posterior polar cataracts to the posterior capsule.1,2,8,9 Care should be taken to avoid too much manipulation of the lens within the capsule; hydrodissection should not be performed in order to avoid creating a split in the already (potentially) weakened posterior capsule. 1,2,8,9
In addition, hydrodelineation may prove helpful in cataract removal in these cases. Having extra viscoelastic on hand in these cases is very helpful in that it can be used to viscodissect lenticular material as well as tamponade vitreous, should it present itself.
1,2,8,9 It is important to inform these patients that IOL implantation may also be compromised in the case of a compromised capsular bag; always try have a
3-piece IOL or ACIOL available, if needed.
1,2,8,9Figure 7 demonstrates a dense posterior polar cataract.
Figure 7. Photo courtesy of Eric Rosenberg, DO MSE
Intumescent white cataracts
Intumescent white cataracts pose challenges during different steps of surgery.1,2,4,10,13,14 Preoperatively, biometry may be difficult to achieve due to large lens size and lack of red reflex.1,2,4,10,13,14 However, capsulorhexis creation may be the most difficult, due to the high pressure gradient within the swollen, fluid-filled capsular bag.1,2,4,10,13,14
During the initial exam, the entire ocular system must be examined carefully, especially if there is a history of trauma.1,2,4,10,13,14 A shallow anterior chamber depth in the presence of normal axial length could indicate zonular laxity.1,2,4,10,13,14 Wrinkling or fibrosis of the capsule could indicate capsular damage, which could lead to rupture and displacement of the nucleus into the posterior cavity during surgery.1,2,4,10,13,14 Presence of a sensory exotropia may be noted in cases of a long-standing cataract, which can lead to diplopia after surgery.1,2,4,10,13,14
With no view to the posterior segment, an ultrasound B-scan should be used to get a gross image of the retina and vitreous cavity—this can help rule out occult retinal detachment or mass.1,2,4,10,13,14 Use of trypan blue dye is a must in these cases to stain the anterior capsule to aid in visualization during creation of the capsulorhexis.1,2,4,10,13,14 However, due to the pressurized capsule, it may be best to first decompress the capsule using a 30G needle to aspirate liquified cortex and prevent radialization of the rhexis.1,2,4,10,13,14 Femtosecond laser assisted cataract surgery can also be used to assist in capsulorhexis creation.1,2,4,10,13,14
Post-vitrectomy
In vitrectomized eyes, there may be an increased incidence of zonular dehiscence and unstable lenses.1,2,4,5 In addition, the anterior chamber may be very deep, and managing phacoemulsifcation fluidics is very important here.1,2,4,5 Extra viscoelastic is important in these cases, with pristine care being taken not to put too much stress on the capsule or zonules. 1,2,4,5
Small pupils
In cases of small pupils, examination for posterior synechiae is important (this may occur in history of iritis or trauma).1,2,10,13,15-17 The surgeon should attempt to gently break synechiae, if present, and examine how the pupil expands with instillation of viscoelastic.1,2,10,13,15-17 If the pupil still does not dilate well, iris hooks or pupillary expansion rings may be used to expand the pupil for adequate access to the cataract.1,2,10,13,15-17 Some surgeons may also make use of cyclopentolate or atropine in the miotic eye several days prior to surgery to promote better pupillary dilation.1,2,10,13,15-17
Very dense/brunescent cataracts
Dense cataracts can present with a several comorbid issues: small pupil size, zonular instability, and a tough posterior plate.1-6,13 The density of the lens may not even allow for routine phacoemulsification.1-6,13 Though this can be attempted, setting the ultrasound to higher power (e.g., the “dense” or “super-dense” setting) and adjusting surgical technique can prove helpful (e.g. switching from “divide and conquer” to a chopping technique).1-6,13 Femtosecond laser-assisted cataract surgery may prove helpful in these cases as well, as it is able to pre-soften the cataract prior to the patient entering the OR.1-6,13
The
MiLoop (Carl Zeiss Meditec Jena, Germany), which can pre-chop cataracts and therefore be used to segment the cataract prior to phacoemulsification.
1-6,13 Extra viscoelastic is helpful in these cases to allow for viscodissection (this can protect the lens capsule) and protection of the corneal endothelium in the cases of high/excessive ultrasound power.
1-6,13 Judicious use of phacoemulsifcation can also help prevent a wound burn.
1-6,13In some cases, surgeons may need to resort to extracapsular cataract extraction.1-6,13 In this case, the surgeon should have in the room the appropriate instruments – a lens loupe, suture, anterior vitrectomy if necessary, pupillary miotic agents (e.g., miochol, miostat), as well as 3-piece and/or anterior chamber IOLs.1-6,13
Extremely long eyes
Patients with extremely long eyes (as with those who have had vitrectomy) may develop reverse pupillary block, where the fluid being infused into the front of the eye greatly deepens the anterior chamber.1-5,10 Attention to fluid dynamics and signs of reverse pupillary block is important in these cases.1-5,10
Extremely short eyes
Small eyes have anatomic features that can complicate cataract surgery—shorter axial length is usually associated with a shallower anterior chamber and therefore less work space.1-5,10 In addition, the corneal diameter may be small and the effective lens position may be more difficult to calculate.1-5,10 Care should be taken in these cases to manage shallow anterior chambers with sufficient viscoelastic coating—the endothelium here will be in close contact with the phacoemulsification tip, predisposing to endothelial cell loss and corneal edema.1-5,10
Some eyes may do best with a limited 25-Gauge pars plana vitrectomy to reduce posterior pressure and provide a deeper anterior chamber.1-5,10 Smaller eyes may also be more at risk of developing iris prolapse; careful maintenance of fluidics and intraocular pressure as well as precise wound construction can permit for a case without having to keep pushing the iris back inside the eye.1-5,10
Preoperative counseling is key
It is important to know what you’re getting into with complex cataract surgery cases—and to communicate this honestly and fully to the patient.1,2 When you know the cataract surgery will not be straight-forward, this needs to be clear to the patient.1,2 Pragmatism is key, not only in meeting surgical challenges but also in making sure the patient knows the challenge you are both up against.
Success is in the
plan! The best weapon to use against a dense lens or other anatomic challenges that may occur is proactive preparation. Look for signs and symptoms that the cataract is likely to be difficult; it is critical to assess the whole patient preoperatively.
Prepare yourself, your team, and your patient for difficult cataract surgery. Always communicate known and expected challenges to the patient before surgery so that realistic expectations are set.
References
- McKinney S. Back to Basics: Complicated Cataracts. Review of Ophthalmology. 2019
- Mathenge W. Cataract surgery in patients with complex conditions. Community Eye Health. 2019; 31(104):77-78
- Basic Clinical Science Course (BCSC) of the American Academy of Ophthalmology. Section 11. 2006-2007
- Cataract in the Adult Eye: Surgery and Diagnostic Procedures. Preferred Practice Patterns. American Academy of Ophthalmology. 2006
- Bobrow JC, Blecher MH, Glasser DB, Mitchel KB, Rosenberg LF, Isbey EK,III, Reich J. AAO Basic and Clinical Science Course (BCSC) Lens and Cataract (91-161) Singapore: American Academy of Ophthalmology; 2008. Surgery for Cataract
- Davis G. The Evolution of Cataract Surgery. Mo Med. 2016; 113(1): 58-62
- Zamora de la Cruz D, Garzon M, Arrieta-Camacho J, Matiz-Morena H. Management of Traumatic Cataract. EyeNet Magazine. 2016
- Lee MW, Lee YC. Phacoemulsification of posterior polar cataracts – a surgical challenge. Br J Ophthalmol. 2003; 87(11): 1426-1427
- Vasavada AR, Singh R. Phacoemulsification with posterior polar cataract. J Cataract Refract Surg. 1999;25:238-245
- Yanoff M, Sassani JK. Lens. In Ocular Pathology, 10, 323-349. E3 (2015)
- Couch S, Bakri S. Use of triamcinolone during vitrectomy surgery to visualize membranes and vitreous. Clin Ophthalmol. 2008; 2(4): 891-896
- Sangal N, Chen T. Cataract surgery in pseudoexfoliation syndrome. Semin Ophthalmol. 2014; 29(5-6): 403-408
- Wong VW, Lai TY, Lee GK, Lam PT, Lam DS. A prospective study on trypan blue capsule staining under air vs under viscoelastic. Eye. 2005
- Devgan U. Intumescent white cataract causes many surgical challenges. Ocular Surgery News. 2018
- Goldman JM, Karp CL. Adjunct devices for managing challenging cases in cataract surgery: pupil expansion and stabilization of the capsular bag. Curr Opin Ophthalmol. 2007; 18(1): 44-51
- Masket S. Avoiding complications associated with iris retractor use in small pupil cataract extraction. J Cataract Refract Surg. 1996; 22(2): 168-171
- Tian JJ, Garcia GA, Karanjia R, Lu KL. Comparison of 2 pupil expansion devices for small-pupil cataract surgery. J Cataract Refract Surg. 2016; 42(8): 1235-1237
- Reidel PJ, Samuelson TW. Capsular tension rings. Colvard DM, editor. Los Angeles CA 2009. 115-121p
- Chaurasia S, Ramappa M, Sangwan V. Cataract surgery in eyes with congenital iridolenticular choroidal coloboma. British Journal of Ophthalmology. 2012; 96(1):138-140