This article, previously published in August of 2022, has been updated for 2023.
Amidst the treatable conditions that can lead to blindness, dry age-related macular degeneration (AMD) is one in which current treatment options are lacking. The likelihood of acquiring dry AMD increases with many non-modifiable risk factors, such as age, ethnicity, genetics, and pre-existing dry AMD in the contralateral eye. There are also modifiable risk factors such as smoking, diet, weight, and UV exposure.
To date, no true treatments for dry AMD can reverse its disease state. For decades, patients have been advised to take preventative actions such as modifying potential risk factors attributed to the progression of dry AMD. Oral AREDS2 vitamins are currently the only supplements clinicians can advise patients to initiate for those with at least intermediate-staged disease.
However, Apellis and Iveric have recently targeted the complement cascade pathway for treating dry AMD and geographic atrophy (GA) with pegcetacoplan and avacincapted pegol, respectively. Both show promising results in slowing down the progression of the disease.
Dry AMD treatment pathways
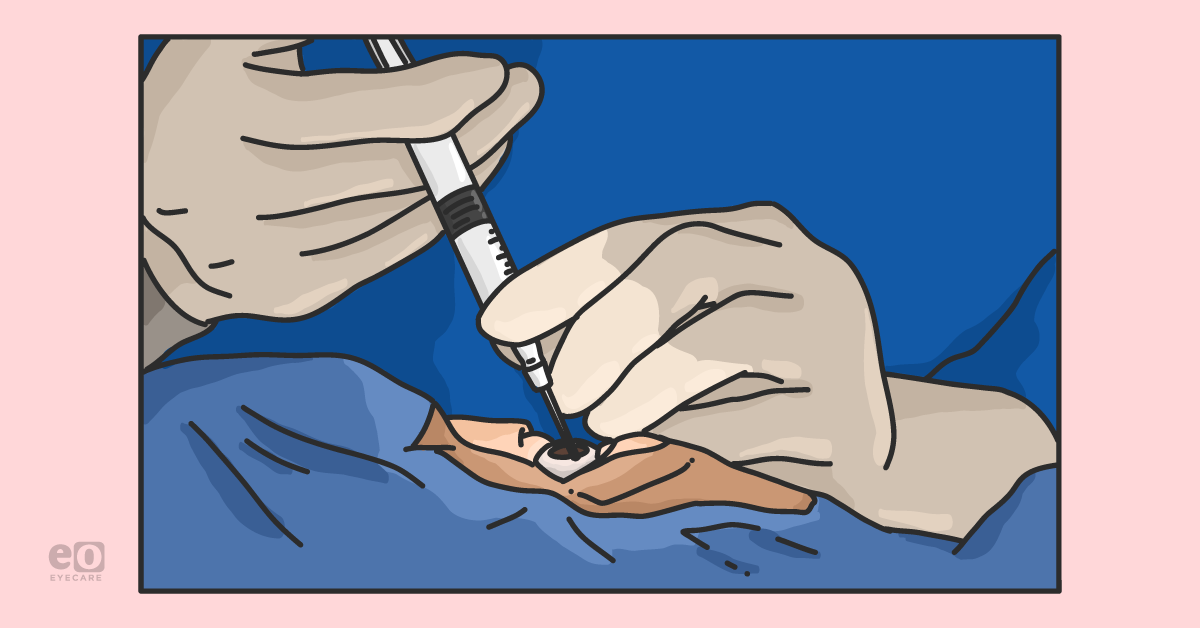
Figure 1 highlights various pathophysiological treatment pathways that have been used to treat dry AMD and current and failed approaches.
Figure 1: Image courtesy of authors.
The present of dry AMD treatment
1. AREDS/AREDS2 vitamins
AREDS vitamins are the only treatment available to delay the progression of dry AMD. AREDS vitamins consist of high-dose vitamin C 500mg, vitamin E 400 IU, beta-carotene 15mg, zinc 80mg, and copper 2mg, which have been shown to reduce the progression from dry AMD.
“The initial AREDS formula underwent randomized double-masked multi-centered clinical trials in 2001.”
Patients were categorized as either having small drusen, intermediate drusen, large drusen, noncentral geographic abnormalities in one or both eyes, advanced AMD, or vision loss due to AMD in one eye. The AREDS formula was administered to the experimental group, and the results were compared against the placebo group. Studies showed that these supplements significantly reduced the development of severe AMD without any significant adverse effects. The risk reduction for the development of advanced AMD from intermediate AMD was reduced by 25%, while the risk of vision loss was reduced by 19% when using AREDS.1
The AREDS2 study was a 5-year study that started in 2006, which took the original AREDS formula and added either omega-3 fatty acids or lutein and zeaxanthin. Concurrently, beta-carotene was removed from the formula. Those in the group with the addition of lutein and zeaxanthin had a better outcome in treating and preventing the progression of dry AMD compared to the original formula in patients with a dietary deficiency. Adding lutein and zeaxanthin and removing beta-carotene compared to the original AREDS formula resulted in an 18% reduced risk of progression of dry AMD.2
Download the Dry Age-Related Macular Degeneration Treatments cheat sheet!
Dry Age-Related Macular Degeneration Treatments Cheat Sheet
This cheat sheet covers past (failed), current, and future (pipeline) treatment modalities aimed at treating dry AMD.
Pegcetacoplan (Syfovre) targets C3 inhibition, which has been shown to decrease the rate of progression of GA when compared to sham controls.3 Currently, this drug is in two Phase 3 clinical trials titled DERBY (n = 621) and OAKS (n = 637), which are 24-month, multicenter, randomized, double-masked sham-controlled studies. For these studies, dosages are set to 15mg/0.10 mL scheduled for monthly or every-other-month intravitreal injections.
“During Apellis’ primary endpoint of 12 months for its trials, the results between the two identically set-up studies evidenced two slightly differing results.”
Monthly administration of pegcetacoplan in the OAKS datasets showed a decrease of GA by 22% (p = 0.0003), and every other month showed a decrease of GA by 16% (p = 0.0052) when compared to sham. The results generated by DERBY datasets with monthly administration showed a decrease of GA by 12% (p = 0.0528), and every-other-month showed a decrease of 11% (p = 0.750) compared to sham.4 Extension of data to 18 months for DERBY showed a 13% reduction with monthly administration (P = 0.0254) and a 12% reduction with every-other-month administration (p = 0.0332) when compared to sham. During the same timeframe, OAKS showed a 22% reduction with monthly administration (p < 0.0001) and a 16% reduction with every-other-month administration (p = 0.0018) when compared to sham.5
Most recently, in November 2022, Apellis submitted their 24-month update, which showed DERBY to have a 36% monthly decrease (p < 0.0001) and a 29% every other month (p = 0.0002) reduction when compared to sham. OAKS showed a 24% monthly (p = 0.0080) and 25% every-other-month ( p= 0.0007) reduction when compared to sham.6 Initially, the PDUFA date was set for late November 2022, but Apellis planned to use the 24-month results to demonstrate a stronger product profile during its launch.7 These results showed increasing effects of the drug with every-other-month injections with consistent results throughout the additional months of testing with a favorable safety profile. The most recent projected PDUFA date is set for February 26, 2023.
Overall, pegcetacoplan has thus far shown both safety and efficacy in both of its Phase 3 trials for both monthly and every other month datasets. Over 24 months, the rate of infectious endophthalmitis was 0.34%, and the rate of intraocular inflammation was 0.24% per injection. These results are consistent with studies of other intravitreal therapies.6 The combined rate of new-onset wet AMD was 11.9%, 6.7%, and 3.1% in the pegcetacoplan monthly, every-other-month, and sham groups, respectively.
3. Avacincaptad pegol (Zimura, IVERIC Bio)
Avacincapted pegol (Zimura) is a complement C5 inhibitor being similarly studied for the treatment of GA. Complement C5 protein inhibitors decrease the activity of the MAC inflammation cascade downstream, which in theory, reduces the degeneration of retinal cells and, thus, the progression of GA. Iveric Bio recently announced the completion of GATHER2, the second Phase 3 trial for avacincapted pegol.9 GATHER2 is an international, randomized, double-masked, sham-controlled, and multicenter trial.8 It included 447 participants, 225 in the treatment arm and 222 in the sham arm. For the first 12 months, participants received either avacincapted pegol 2mg or sham injection monthly.9 At the end of the 12 months, participants were re-randomized to receive either avacincapted pegol 2mg once a month or every other month until month 23.8
The primary endpoint was the mean rate of growth (slope) in the GA area, which was measured by fundus autofluorescence readings at 0, 6, and 12 months. It was calculated using the square root transformation of the GA area growth. The square root transformation was 0.336mm for avacincapted pegol 2mg and 0.392 mm for sham—a difference of 0.056mm and a percentage difference of 14.3%. The study also included the observed mean rate of GA area growth, which was 1.745mm2 in the avacincapted pegol group and 2.121mm2 in the sham group.8 The difference was 0.376mm2, and the percentage difference was 17.7%.8
“Iveric Bio also reported the difference in efficacy depending on geographic region.”
In the U.S., there was a 25.5% reduction in the mean growth rate using the square root transformation and a 32.0% reduction using the observed atrophy area.8 Participants in the U.S. made up 42.7% of the study and had a mean baseline lesion size 13% smaller than participants outside the U.S. These results support the hypothesis that avacincapted pegol is more impactful in earlier stages of the disease.
The mean change in best corrected visual acuity (BCVA) showed a favorable trend for avacincapted pegol but no favorable trend was seen for the low luminance best corrected visual acuity (LL BCVA).9 There were no adverse events of endophthalmitis, intraocular inflammation, or ischemic optic neuropathy throughout the 12 months of treatment.9 There was a 6.7% incidence of choroidal neovascularization in the avacincapted pegol 2mg group compared to 4.1% in the sham group.8 This included wet and dry macular choroidal neovascularization (CNV) and peripapillary CNV.
The company had previously completed GATHER1 involving 177 patients, a similar Phase 3 trial which showed a mean rate of GA growth of 0.283 mm in avacincapted pegol 2mg group and 0.392mm in the sham group with a percentage difference of 27.7% based on square root transformation. The avacincapted pegol group had a 1.221mm2 mean rate of GA growth compared to 1.889mm2 in the sham group, with a percentage difference of 35.4% based on the observed area.9 The GATHER1, there was one reported case of intraocular inflammation related to an injection procedure that was transient and mild. There was 9% total CNV in the avacincapted pegol group in GATHER1 at 18 months, compared to 2.7% in the sham group.8
Both GATHER1 and 2 showed statistical significance in slowing down the progression of GA. Iveric Bio is expected to submit a New Drug Application (NDA) to the FDA by the end of the first quarter of 2023, and a Special Protocol Assessment (SPA) by the FDA could see the drug in clinical use very soon.
The future of dry AMD treatment
1. ANX007 (Annexon)
This antigen-binding fragment (Fab) inhibits the classic complement pathway by binding to C1q. In Phase 1 clinical trials, it was studied on monkeys with a single dose of 1mg and 5mg administered using intravitreal injection.9 Tissue sampling was then examined for levels of C1q.9
Another study used repeat doses with 0, 1, 2.5, and 5mg on days 1 and 29 with sampling on days 44 and 59.9 C1q levels were measured using specific and sensitive ELISA-based assays. The half-life of the drug was found to be 3 days.9 Aqueous and vitreous levels were highly correlated, and aqueous levels were four-fold lower, confirming the drug's diffusion to the target in the back of the eye.9 The Phase 1 trials proved that the drug is well-tolerated and is a successful mechanism to target and inhibit the classic complement pathway.9
Recently, Annexon announced that it completed Phase 2 clinical trial, ARCHER, which is a multi-center, double-masked, placebo-controlled trial with 270 patients.10 This trial evaluates monthly and every other month, with the primary endpoint being changed in geographic atrophy lesion size using fundus autofluorescence.10
2. CB2782 (Catalyst Biosciences)
CB2782 is a drug by Catalyst Biosciences from San Francisco, California, studied to treat dry AMD. It works as a complement protease that degrades available C3, thus decreasing the inflammatory response.11
CB2782 was under development through the collaboration of Catalyst Biosciences and Biogen, though progress was paused when Biogen decided to cease its involvement in further development. Catalyst Biosciences
regained the rights to CB2782.
12 CB2782 is not currently under clinical trials, though it is expected to enter Phase 1 shortly.
This anti-C5, optimized for subcutaneous delivery, binds and prevents activation of C5.13 C5 is an essential mediator of disease progression,13 in the complement, cascade C5 is cleaved into C5a and C5b9. C5a is a chemotactic agent which attracts neutrophils, and C5b is part of the membrane attack complex (MAC).13
Phase 1 clinical trials were conducted to examine the drug for serious side effects.13 Phase 1 trials were completed in four groups studied: SQ route in single-dose, SC in multiple doses, SC single dose with rHuPH20, and an IV single-dose; rHuPH20 is used to reversibly modify the hypodermis to improve the bioavailability of subcutaneous injection.14
4. HMR59 (Hemera Biosciences)
HMR59 is a novel gene therapy treatment developed by
Hemera Biosciences for treating dry and wet AMD. It is an analog to the naturally found protein, CD59 (also known as MAC-inhibitory complex), that protects host cells from the inflammatory and damaging complement cascade.
15 Increased levels of complement lead to unnecessary chronic inflammation damaging the retina. Injection of HMR59 into the vitreous cavity results in the production of soluble CD59 (sCD59), allowing the retina to inhibit the damaging effects of complement activation. HMR59 is currently in Phase 1 clinical trials.
15Danicopan is an orally active, first-generation, small-molecule inhibitor of factor D. Factor D is an enzyme in the alternative complement pathway.16 It is a serine protease enzyme and the rate-limiting enzyme in the reactions that make C3 convertase. C3 convertase is essential in mitigating the complement cascade because it cleaves C3 and C5, resulting in downstream inflammatory effects, including the attraction of neutrophils and activation of phagocytosis.16
It is currently in Phase 2 clinical trials in a double-masked, placebo-controlled study examining its effects on patients with geographic atrophy secondary to dry AMD. The study examines 100mg twice daily, 200 mg twice daily, and 400mg daily oral tablets.17 The clinical trial is expected to end in June 2025.17
6. Ionis-FB-LRX (Ionis Pharmaceuticals Inc.)
Ionis-FB-LRX is a ligand-conjugated (LICA) antisense drug under development by Ionis Pharmaceuticals Inc in partnership with Roche that works by decreasing the production of complement factor B. When activated, factor B allows for the catalytic activity of both C3 and C5 convertases of the alternative pathway.
Ionis-FB-LRX is currently under Phase 2 clinical trials for its efficacy in changing the difference in the rate of change in the area of geographic atrophy due to dry AMD through the GOLDEN study.18 This Phase 2 study is a double-masked, randomized, stratified, placebo-controlled study that is being performed at multiple centers. Three dose levels are being studied to determine the most effective therapeutic dose.
7. ALK-001 (Alkeus)
One pathology of dry AMD is the formation of vitamin A toxic dimers due to the defective visual cycle.
19 ALK-001 (Alkeus) is a chemically modified vitamin A administered as an oral tablet.
19 ALK-001 is modified with deuterium instead of hydrogen.
19 This stabilizes the molecule and slows the rate of formation of toxic vitamin A dimers.
19The drug is currently in Phase 3 clinical trial, Study of ALK-001 in Geographic Atrophy (SAGA), a double-blind, randomized placebo-controlled study with 200 participants taking the drug and 100 taking the placebo.20 Results are expected in 2023.20
Kamuvudines are a class of molecule analogs to nucleoside reverse transcriptase inhibitors (NRTIs) that can inhibit inflammasome activation, which is linked to increased geographic atrophy. Unlike NRTIs, kamuvidines are metabolized through a different mechanism and lack the mitochondrial toxicity found in NRTIs.21
It has been observed that in preclinical trials, kamuvudines have been highly influential in functionality. While not yet under clinical trials, Inflammasome Therapeutics plans to begin the clinical trial process for kamuvudines soon.22
9. Xiflam (InflammX Therapeutics Inc)
This orally administered small molecule once daily targets dysregulated Connexin43 hemichannels, which are responsible for autoinflammation.
23,24 The pathology is related to the dysregulation of the inflammasome NLRP3 pathway.
23,24 The drug is also being studied for
diabetic retinopathy and diabetic macular edema.
23It was discovered two decades ago as a treatment for migraines but was eventually shelved.24 However, because it targets Connexin43 channels and crosses the blood-retina barrier, it shows promising mechanisms to slow the progression of dry AMD.24 In studies on a rat model with GA, the retinal structure was preserved for 3 months after treatment with Xiflam.24 Phase 2 clinical trials are expected in late 2022.24
10. Doxycycline (Oracea)
Oracea (Doxycycline) is another oral medication evaluated for efficacy in treating dry AMD due to its anti-inflammatory properties.25 It is currently in a Phase 2/3 randomized, double-blind, placebo-controlled clinical trial, which aims to evaluate its efficacy in treating geographic atrophy secondary to dry AMD.
Here, 286 patients will undergo a 6-month observation period followed by a 24-month treatment period.26 The treatment group will be administered a 40mg doxycycline capsule, and the placebo group will be administered a placebo capsule. The results of this study are still pending.
11. FHTR2163 (Genentech/Roche)
FHTR2163 is a novel antigen-binding fragment (Fab) that inhibits high-temperature protein A1 (HtrA1).27 HtrA1 typically induces the breakdown of extracellular matrix proteins and results in photoreceptor atrophy and destruction of retinal pigment epithelium and Bruch membrane choroid.27 The drug has been studied in Phase 1 clinical trials in which no limiting toxicities or serious adverse effects were reported.27 The drug is administered in intravitreal injections. Studies show sustained pharmacodynamic effects at a maximum dose of 20mg.27
It is currently in Phase 2 clinical trials examining its tolerability and efficacy.28 It is being studied every 4 weeks and every 8-week doses for 76 weeks, with the primary outcome being the mean change in GA area from baseline.28
Stem cell therapies for dry AMD
1. Human embryonic stem cells - Lineage Cell Therapeutics
Lineage Cell Therapeutics of California is currently conducting clinical trials for an innovative new treatment for dry AMD. They are taking a transplant approach to address the degenerating effects of dry AMD by using stem cells. Currently, in Phase 1/2a open-label clinical study, Lineage Cell Therapeutics is producing allogeneic RPE cells derived from pluripotent stem cells that would be implemented subretinally in patients who suffer from dry AMD.
29 2. Human embryonic stem cells - Lineage Cell Therapeutics
OpRegen is a cell-based product composed of retinal pigment epithelial (RPE) cells derived from human embryonic stem cells (hESC) with the suspension of Balanced Salt Solution Plus or CryoStor 5.
30 It is currently in Phase 1/2 of clinical trials testing the safety, tolerability, and efficacy.
30 There are 24 subjects in this dose-escalating study with a target dose of 50,000 to 200,000 cells delivered via surgery into the subretinal space. Results are expected to be completed in December 2025.
31 Neuroprotection
Neuroprotection strategies are another method being studied to aid in decelerating the progression of geographic atrophy secondary to dry AMD. This is done by targeting ways to reduce oxidative stress, leading to a decrease in toxic molecules that are capable of damaging the retina. This idea was initially postulated through the successes of the AREDS vitamins trials, which led to the belief that reducing oxidative stress may lead to preserved vision.
Notable studies included the VITAL clinical study that randomized administration of vitamin D3 and/or omega 3 fatty acids and OT-551, which is applied topically.32 OT-551 is converted to its active metabolite, TEMPOL-H, which can neutralize free radicals. No studies have concluded the initial idea of neuroprotection through oxidative stress.33
1. Elamipretide (Stealth BioTherapeutics Inc)
Dry AMD has been shown to have decreased number of mitochondria and fewer cristae in each mitochondrion in the retinal pigment epithelium.34 There is also significant abnormal morphology and disorganization compared to normal aging.34 This results in the disruption of respiratory complexes and leads to apoptosis.34
Elamipretide is a peptide that targets the inner mitochondrial membrane and binds reversibly to cardiolipin.
34 It increases mitochondrial respiration and improves electron transport chain function and ATP production.
34 It also reduces ROS levels and normalizes the mitochondrial membrane, and improves mitochondrial function.
34 It can be used in the treatment of non-central geographic atrophy.
34 The drug is administered subcutaneously 40mg.
35 In the Phase 2 study, the primary endpoint at 48 weeks examined low-luminance VA.
35 This study was completed in April 2022, and data is expected in late 2022.
35 2. Risuteganib (Allegro Ophthalmics)
Risuteganib is a synthetic peptide that regulates the function of integrins that play a role in the pathogenesis of dry AMD. It regulates mitochondrial dysfunction and down-regulates oxidative stress response to restore retinal homeostasis. In its most recent Phase 2a study, Risuteganib showed that 48% of patients had met the primary end goal of >8 letter gain in BCVA compared to the sham group, in which only 7.1% of patients had an improvement.
36 This study proved that Risuteganib effectively improves vision in patients with dry AMD without geographic atrophy. Allegro successfully completed a Phase 2a trial of patients with intermediate dry AMD and is preparing to initiate a Phase 2b/3 trial.
3. Photobiomodulation (LumiThera)
Light-based technology is a new model of treatment that stimulates bioenergetic output in tissue.37 It uses far-red to infrared spectrum (500 to 1000nm) to stimulate photoreceptors, improving ATP output by the mitochondria’s respiratory chain components.37 It also modulates the production of ROS and NO and improves cell function and livability.37 In LIGHTSITE 1, 46 eyes were treated in two series of treatments three times per week for 3-4 weeks over 1 year.37 There was an average BCVA score gain of four letters after each treatment. There was also a significant improvement in contrast sensitivity, central drusen volume, thickness, and quality of life.37
LIGHTSITE 2 and 3 are ongoing clinical trials in Europe and the United States, respectively.38 Both are double-blind trials that examine the effect of photobiomodulation (PBM) over a 2-year period, with participants receiving a placebo or PBM every 4 months.39
Initial results show decreased progression of dry AMD to GA in patients who received PBM, 9.3% of patients progressed to geography atrophy in the sham group versus only 1.1% in the PBM group.37 In the PBM group, at 13 months primary endpoint, there was around 5.5 letter improvement from baseline, 55% showed 5 letters or more improvement, the mean was 9.7 letters, and 26% achieved 10 letters or more with a mean of 12.8 letters.37
4. Brimonidine tartrate (Allergan)
Brimonidine tartrate, an alpha-2 adrenergic receptor agonist, is best known for its therapeutic effects in treating
glaucoma. Recently, a brimonidine drug delivery system is under clinical trials to treat dry AMD. In primate models, it has been shown to be effective in protecting the RPE and photoreceptors from blue light-mediated damage.
40A Phase 2, randomized, multicenter, double-masked, 24-month study used 132μg, 264μg, and a sham to test its efficacy in treating dry AMD with geographic atrophy. Results of this trial showed that in both the 132μg and 264μg groups, the area of growth for geographic atrophy was consistently smaller than the area of growth for the sham group at month 3 and month 12.40 Side effects were only related to the procedure of performing the injection. These Phase 2 results support the movement of the brimonidine drug delivery system to enter Phase 3 clinical trials.
Citrus Therapeutics is developing a novel dry and wet AMD therapy called CTZ1, which has both anti-oxidative and anti-angiogenesis properties. The small molecule consists of two distinct pharmacophores: an antioxidant carbazole moiety fused with a nicotine analogue. It has been shown in silico to be both stable and effective at reducing oxidative stress.
By way of its nicotinic inhibition, the small molecule has also been shown to inhibit endothelial cell proliferation and blood vessel formation. Together, this pipeline drug may have vascular disruptive properties that can stabilize retinal endothelial cells and modulate the aberrant angiogenic mechanism that goes beyond simple VEGF blockade.
The past and failures of dry AMD treatment
It is essential to recognize recent drugs and trials that were unsuccessful in further progress. These studies may give scientists and clinicians more insight into what mechanisms or modes of delivery may or may not work in the future.
1. Lampalizumab (Genentech)
Lampalizumab is a selective factor D inhibitor and was studied in CHROMA and SPECTER, Phase 3 clinical trials that examined the drug’s effect on reducing the enlargement of GA lesions secondary to AMD.
41 Patients in the treatment groups received either 10 MG IVT every 4 weeks or every 6 weeks.
41 There were 906 patients in CHROMA and 975 patients in SPECTRI.
41 The study found no significant benefit in patients receiving lampalizumab compared to the sham group at 48 weeks.
41,42 2. Eculizumab (Alexion)
Eculizumab is a monoclonal antibody under clinical trials for treating dry AMD and geographic atrophy in the COMPLETE study. It functions by binding to C5 complement protein and inhibiting its conversion to C5a and C5b, ultimately preventing the formation of the membrane attack complex.43
“The study concluded that intravenous eculizumab was well tolerated, however, it showed no efficacy in decelerating or improving the progression of dry AMD and geographic atrophy.”
At 52 weeks, the treatment group showed a geographic atrophy growth of 0.37+/- 0.22mm, and the placebo group showed a geographic atrophy growth of 0.37 +/- 0.21mm (P = 0.93).43 The effect of eculizumab on drusen volume was also studied; initially, the mean drusen volumes were 0.49 and 0.47 in the treatment and placebo groups, respectively. At 26 weeks, volumes were found to be 0.51 and 0.42mm in the treatment and placebo groups, respectively (P = 0.17).43 Eculizumab has since stopped the further investigation.
3. Tesidolumab (Novartis)
Tesidolumab (LFG316) is an IgG1 monoclonal antibody directed against complement factor C5.44 It binds to C5 and prevents its cleavage in C5a and C5b, thus preventing downstream activation of signal transduction and membrane attack complex (MAC) formation.44 The drug was studied in two doses, 10mg/100μL and 50mg/100μL intravitreal injections, administered every 28 days for 12 injections.44 The drug had an acceptable safety profile but was ineffective in reducing the GA lesion growth rate.44
4. CLG561 (Novartis)
Properdin is a positive regulator of the alternative pathway in the complement system.
45 It prevents the destruction of C3 and C5 convertase and thus amplifies downstream complement activity.
45 CLG561 is an anti-properdin antibody that was found to inhibit C3a and C5a generation and C3b and C5b-9 deposition.
45 In Phase 1, clinical trials showed improved BCVA in different dose groups, but there was elevated intraocular pressure, and a common adverse effect was conjunctival hemorrhage.45 CLG561 failed Phase 2 clinical trials, which were completed in December 2017.45 The clinical trial also studied a combination of CLG561 with LFG316, an IgG1 that targets C5 and inhibits the classic and alternative complement pathways.45 LFG316 had an acceptable safety profile but failed the 12-month end-points in Phase 2 clinical trials.45,46 There was no significance in combination therapy with CLG561 and LFG316.46
Emixustat inhibits the development of retinal pigment epithelium-specific associated with atrophy.47,48 It modulates the visual cycle by inhibiting a critical enzyme of the RPE65 pathway. The visual cycle is the process by which vitamin A is typically recycled in the eye. Slowing the visual cycle reduces the availability of vitamin A derivatives to form precursors of toxic A2E and related compounds.
It was examined as an oral compound in 320 subjects in a 24-month study but failed to mean its primary and secondary endpoints.
47,48 Acucela is exploring emixustat for slowing the progression of vision loss in patients with
Stargardt disease.
Fenretinide is a synthetic vitamin A retinoid homolog proposed to reduce systemic vitamin A levels, reducing toxic fluorophores and lipofuscin levels in the eye. Its proposed mechanism of action was indirect inhibition of retinol delivery to the RPE.49 It was studied in clinical trials for its efficacy in treating patients with geographic atrophy secondary to dry AMD. However, further testing was halted due to no significant difference from the placebo arm of the Phase 2 study.49
NT-501 is an intraocular implant with cells modified to secrete ciliary neurotrophic factor (CNTF) in the posterior segment.50 The cells are encapsulated in a semipermeable membrane, which releases neurotrophic factors for at least 1 year, as seen in animal models.50 This reduces photoreceptor cell loss and increases the thickness of the retina.50 The device is surgically implanted into the vitreous.
Phase 2 clinical trials showed the implants were well tolerated and had no adverse effects.51 There was a dose-dependent increase in retinal thickness and an improvement in BCVA in the high-dose group compared to the low-dose and sham groups.51 Results at 1 year showed a non-statistically significant trend toward stabilization of visual acuity in the high-dose group. In the subgroup of patients with initial good visual acuity, the high dose appeared to maintain that good vision; however, there was no difference in the progression of GA with the implant compared with the sham.
NT-501 is being studied in patients with macular telangiectasia Type 2 in a Phase 3 clinical trial.
8. AL-8309B, tandospirone (Alcon)
The GATE study was used to determine the efficacy of tandospirone, a topical selective serotonin 1A agonist, approved and marketed in Japan as an antidepressant. This study evaluated the difference in the progression of geographic atrophy secondary to dry AMD between the use of tandospirone (1% and 1.75%) and placebo for 30 to 36 months.52
Results from this study demonstrated that the total area of geographic atrophy was increased in all three groups. The area increase averaged 1.73, 1.76, and 1.71 mm2 for the 1%, 1.75%, and placebo groups, respectively.52 The two doses of the drug did not affect lesion growth in the eyes with GA, and thus further development of this drug was halted.
9. OT-551 (Othera)
OT-551 is hydroxylamine with antioxidant properties.53 It was investigated in a Phase 2 trial with ten patients with bilateral GA.53 Topical administration of OT-551 was used in one eye, three times a day, for 2 years. The drug was well tolerated with few adverse effects. There was no statistically significant difference between the eye treated with OT-551 and the contralateral eye.53 It was concluded that the drug is ineffective in treating GA at the current dose and mode of delivery.54
Conclusion
There are significant advances in treating GA secondary to dry AMD, with new treatments on the horizon; however, several questions remain unanswered. It is still being determined when exactly treatment should be initiated depending on the size of the lesion and its proximity to the fovea.
We expect the consensus to be larger areas of GA closer to the fovea (i.e., “fovea-threatening”) will have a lower threshold for initiation of therapy, in contrast to smaller areas further away from the fovea.
Some patients have central GA in one eye and non-central GA in the contralateral side—would it be worthwhile to treat the contralateral side sooner to prevent vision loss in a patient’s better-seeing eye? It must be clarified when treatment should be initiated on the contralateral side for such cases. In addition, the exact frequency and length of treatment are not well defined, and real-world, long-term data is ultimately needed.
“Interestingly, a subset of patients treated with these medications also succumbs to a higher rate of progression to wet AMD.”
How these patients get treated simultaneously for GA and wet AMD remains unclear (i.e., same-day anti-VEGF therapy, for example, versus alternating GA injection with wet AMD therapy on a subsequent visit). Because of the inflammatory issues seen with brolucizmuab (Beovu, Novartis) and recent recall issues seen with the port delivery system (PDS or Susvimo, Genentech), long-term safety measures must also be considered.
We remain cautiously optimistic and excited about a potential new intravitreal therapy to slow down GA progression in 2023.