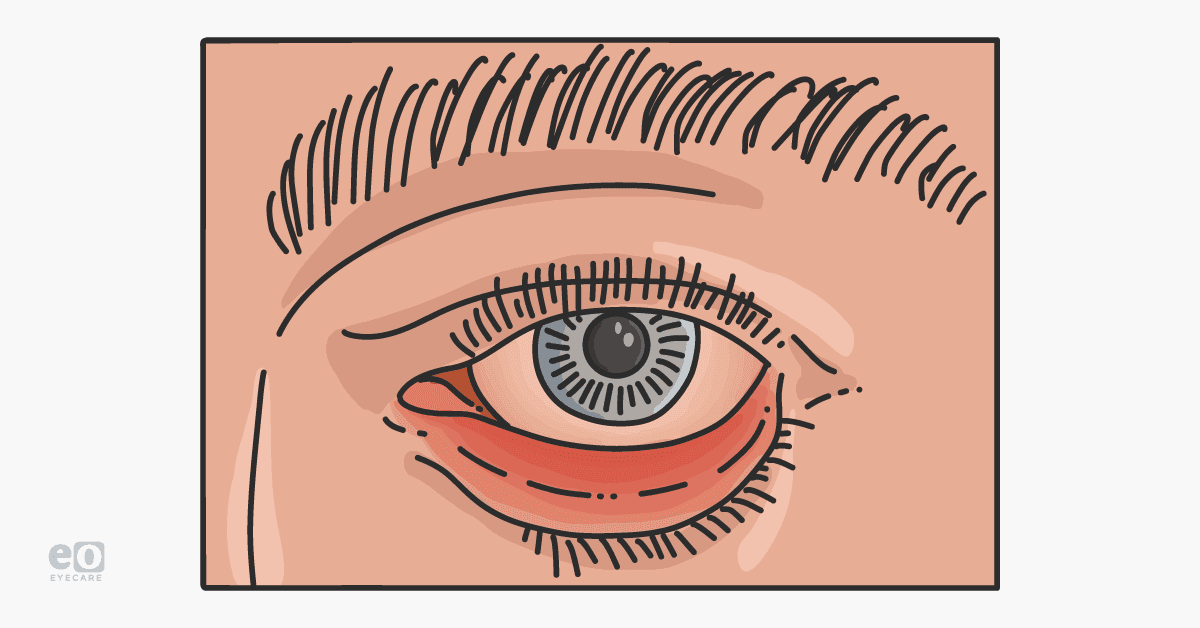
Ectropion is the downward positioning and sagging of the lower eyelid;1 this can expose more of the inferior ocular surface leading to dryness and irritation.
The excess exposure and dryness of the cornea can cause foreign body sensation and potentially serious corneal pathology, such as keratopathy and even ulceration.2 Lower eyelid ectropion is more common, and its incidence increases with age.1
Prevalence of ectropion
The prevalence of ectropion is the same between genders but presents at a higher rate in men aged 80 and older.3 Factors that lead to ectropion development include a history of systemic hypertension, diabetes, tobacco use, and stroke.3 The risk of ectropion development is increased when there is a history of skin cancer and sun sensitivity.
Untreated ectropion can lead to severe dry eyes, persistent corneal abrasions, corneal ulcers, and eye infections. Ectropion can decrease visual acuity and may lead to blindness if left untreated or in chronic and severe cases.
Figure 1 illustrates the downward positioning and sagging of the lower eyelid as seen in ectropion.
Figure 1: Courtesy of Leonid Skorin, DO, OD, MS, FAAO, FAOCO
Evaluation of ectropion
Ectropion can be identified on physical and slit-lamp examination. When the lid margin excursion is greater than 6mm, ectropion is present. The greater the lid excursion, the greater the severity of ectropion.
Structural findings of ectropion include:
- Punctal eversion
- Lateral canthal laxity
- Medial canthal laxity
- Total lid laxity
Punctal eversion is a clinical sign of medial ectropion. Fluorescein application can be used to highlight the corneal surface to identify any indications of corneal surface dryness. Dry eye secondary to punctal eversion is managed with artificial tears or eye ointment. When assessing for dry eye, tear production should be measured. The Schirmer/Basal secretion test measures total tear production with special eye strips.2,4
When the strips show less than 10mm of wetness in 5 minutes, decreased tear production is confirmed.2,4 Dry eyes can cause excessive tearing (epiphora) as well, particularly as the cornea is exposed with increasing ectropion severity. Excessive tearing and poor drainage compound dryness.
Figure 2 shows Schirmer test strips that have been positioned in the lower lateral lid margin. Basal secretion is measured after topical ophthalmic anesthetic with fluorescein was instilled.
Figure 2: Courtesy of Leonid Skorin, DO, OD, MS, FAAO, FAOCO
Eyelid laxity caused by ectropion
Eyelid laxity is another clinical sign of ectropion. Laxity can be referred to as lateral canthal, medial canthal, or total lid laxity. The distraction test is where the lower eyelid is displaced away from the ocular globe. The distance between the eye and the eyelid margin is assessed. Normally, the maximum distance the eyelid can be distracted is only 2 or 3mm.5 When the distance is 10mm or greater, significant eyelid laxity is present and indicates severe ectropion.6
Figure 3 demonstrates the distraction test in which a measurement is taken with a millimeter ruler to gauge the amount of displacement of the lower eyelid from the globe.
Figure 3: Courtesy of Leonid Skorin, DO, OD, MS, FAAO, FAOCO
Laxity can also be measured by the snap-back test. In this test, the patient's eyelid is pulled inferiorly and released. The patient is instructed not to blink. The eyelid should snap back to its normal positioning against the globe almost immediately.5
Any delay in this indicates eyelid laxity. Severe laxity is evident when the eyelid completely fails to reposition itself against the globe even after the patient blinks or it takes more than 10 seconds for the eyelid to return to baseline.5,6
Using the snap-back test to measure eyelid laxity
Figures 4A and 4B represent the snap-back test. In 4A, the lower eyelid is being pulled down with the examiner's finger and then the lid is slowly released. After release, as seen in 4B, the eyelid does not reposition itself against the globe.
Figure 4A: Courtesy of Leonid Skorin, DO, OD, MS, FAAO, FAOCO
Figure 4B: Courtesy of Leonid Skorin, DO, OD, MS, FAAO, FAOCO
Assessing the lateral canthal tendon with the distraction test
Medial and lateral canthal tendon integrity can be assessed using the horizontal eyelid distraction test. The medial and lateral aspects of the eyelid are normally firmly attached to the periosteum.5 Weakening and stretching of these tendons can be demonstrated by moving the eyelid either medially or laterally.5 A displacement of 10mm or more is not uncommon when significant laxity is present.5,6
Figure 5 illustrates testing of the lateral canthal tendon; significant horizontal displacement can be noted.
Figure 5: Courtesy of Leonid Skorin, DO, OD, MS, FAAO, FAOCO
What is the etiology of ectropion?
Ectropion can be categorized as congenital or acquired. Congenital causes include primary ectropion as an isolated condition or secondary ectropion as coexisting with other health conditions.
Commonly, secondary ectropion is found with Down syndrome and blepharophimosis syndrome. Acquired ectropion is categorized as involutional, paralytic, mechanical, and cicatricial.
Types of ectropion
1. Involutional ectropion
Involutional ectropion is the most common condition encountered.6 It is most often associated with the processes of aging.7 Patients with increased eyelid tissue laxity, but especially horizontal laxity, are likely to develop involutional ectropion.7,8
Punctal eversion in conjunction with horizontal lid laxity indicates the presence of medial ectropion and would also need to be addressed if surgery is contemplated. Full rotation of the eyelid away from the globe is referred to as tarsal ectropion and indicates detachment of the lower eyelid retractors.8
“Based on the severity of the ectropion, management can begin with conservative therapy.”
This would include topical ophthalmic artificial tears during the day and bland ophthalmic lubricating ointment at bedtime. In more advanced involutional ectropion, surgical treatments would include lateral canthal strengthening to address the horizontal laxity and medial spindle procedure to correct any medial ectropion if it is present.9 For tarsal ectropion, both lateral canthal strengthening and reattachment of the retractors are necessary.8
2. Paralytic ectropion
Stroke, facial nerve paralysis, or any post-operative complication inducing facial nerve injury can cause paralytic ectropion.10 Paralytic, also known as neurogenic ectropion, isn’t associated with aging and is managed by the length of the episode.
With a short episode of paralytic ectropion, lubrication is usually effective. Short-term tarsorrhaphy or upper eyelid gold weight placement can also be therapeutic. For persistent paralytic ectropion, a partial permanent tarsorrhaphy is indicated.8,10
3. Mechanical ectropion
When an anatomical factor influences the downward movement of the eyelid, it is called mechanical ectropion. It can occur with chalazion, tumor, dermatochalasis, neurofibromatosis, and swelling.8
Although mechanical ectropion is rare, it has an excellent prognosis. Ocular lubrication remains a mainstay, but surgical treatment includes excision and removal of mass.8
4. Cicatricial ectropion
Cicatricial ectropion occurs because of trauma, infection, chronic dermatologic conditions, inflammation from chronic uncorrected involutional ectropion (which can cause vertical skin shortage), as well as scarring from surgery.2,6,8 Differential diagnosis must rule out skin cell carcinoma.
The anterior lamella pulls the eye away from the globe, reducing punctal tear drainage and exposing the palpebral conjunctiva, which leads to keratinization of this mucous membrane. Treatment includes conservative therapy as well as addressing any pre-existing skin conditions. Horizontal strengthening and full-thickness skin grafts are the most common surgical options for cicatricial ectropion.2,6,8
How can eyecare practitioners treat ectropion?
Ectropion treatment includes lubrication with artificial tears and bland ophthalmic ointment. It is advised to keep the eyes moist at all stages, particularly for mild cases of ectropion. Short-term treatment includes taping the affected lid, but this is not a permanent treatment option. As ectropion severity increases, surgical intervention should be considered.
Surgical options for ectropion repair include lateral canthal strengthening, medial spindle procedure, and autologous graft for cicatricial ectropion repair. Both topical and local anesthetic is administered prior to each of these procedures. Thorough infiltration of the area with local anesthetics such as lidocaine 1% or 2% with 1:100,000 epinephrine must first be accomplished.
“The epinephrine decreases tissue bleeding and minimizes systemic absorption of the lidocaine.”
These procedures can be done in an office minor operating room, an ambulatory surgical center (ASC), or a hospital operating suite. For extremely anxious patients or those with multiple systemic pathologies, a surgical center or hospital facility would serve as a more optimal venue. In these locations, an anesthesiologist can then administer intravenous sedation and monitor the patient's oxygen level and cardiac status.
Those patients who have cicatricial ectropion that will require graft acquisition and placement should have the surgery performed in an ASC or hospital setting because of the extended time frame needed for the grafting part of the procedure.
Lateral canthal strengthening to treat ectropion
Lateral canthal strengthening is the backbone procedure of ectropion surgery. It involves a lateral canthotomy (splitting of the lateral canthus), cantholysis (incision of the lateral canthal tendon), excision of excess lateral lid tissue, and formation of a tarsal strip.
The tarsal plate of the eyelid is then secured with a suture to the inner aspect of the periosteum of the lateral orbital wall, and the lateral canthus is reconstructed.11 This results in horizontal shortening and tightening of the eyelid. The eyelid returns to its normal anatomical position and re-approximates itself against the globe.11
Medial spindle procedure to treat ectropion
Medial ectropion can be repaired with a medial spindle procedure. This involves the excision of a posterior lamellar fusiform wedge of conjunctiva, inferior eyelid retractors, and tarsal plate.11 This excision site is then closed with absorbable sutures.11 The closure results in the inversion of the medial eyelid back towards the globe. This procedure also addresses any punctal ectropion.11
Cicatricial ectropion repair
With cicatricial ectropion repair, a lateral canthal strengthening procedure is first performed, and all scar tissue is released. An autologous donor graft is obtained. This can be graft tissue from the upper eyelid (blepharoplasty) or tissue from behind the ear. The graft is then sutured to the recipient bed.11
Post-operative care involves conservative pain management, suture removal in 1 to 2 weeks, and topical antibiotic ointment for the affected eye for 2 weeks. Ice packs are recommended to decrease inflammation, redness, and swelling. Complications of eyelid surgery include infection, bleeding, pain, graft failure (after cicatricial ectropion repair), scarring, corneal damage, and ectropion recurrence.10
Final thoughts on ectropion
Physical and slit lamp examination can be used to efficiently assess ectropion appearance and its' potential progression. Assessment of risk factors and co-morbid conditions remains valuable in reducing the incidence of ectropion progression.3
Early detection can play a role in the conservative management of ectropion, which often leads to improved outcomes. For long-term management and in cases of severe ectropion, surgical intervention remains the definitive treatment.