We’ve all had those optometry cases—the ones where we know that if our patient had waited just a day longer, they might have never made it in at all.
- That teenage cross country runner with the intracranial aneurysm?
- The mother of two whose blurred vision turned out to be from a tumor—but hadn’t been able to make it to the doctor for herself this year?
- The dad who thinks he’s perfectly healthy but has a blood pressure measurement of 200/120?
As ODs, we can sometimes get caught up in the routine of exam after exam after exam . . . but every so often we encounter a patient where we can say, yes: my intervention saved that person’s life. These life-saving interventions happen every day, and it’s amazing how much the eyes can truly tell about the body.
It doesn’t matter what setting you practice in—whether it’s a hospital, private practice, group practice, or a corporate location—you’ll see cases like these. That is the beauty of what we do as eye care professionals; we have the opportunity to make a difference every day.
There is a common misconception that optometrists just refract in corporate-affiliated settings, but it is exactly that, a misconception. Optometrists practicing in these offices have ample opportunities to treat and manage ocular disease, as well as the opportunity to impact a patient’s life.
These cases were originally collected in fall of 2018 and the information shared reflects where the OD practiced at the time the case took place.
Here we share four case studies managed by optometrists practicing in offices at National Vision retail locations where timely intervention was likely the difference between life and death.
Case Study 1: Parinaud Syndrome and Pineal Gland Germinoma
DOCTOR: SVETLANA PEKOVIC, OD
Doctor’s Exchange of Indiana, P.C.
Practices at an America’s Best Contacts & Eyeglasses location in Merrillville, IN
BACKGROUND: 12-year-old male
CHIEF COMPLAINT: The patient’s mother reported crossing of eyes for the last five months, and complaints of periodic headache over the last nine months. The patient and his mother believed his symptoms were caused from current glasses that were three years old.
CASE FINDINGS:
Examination revealed:
- Fixed dilated pupils, non-responsive to light
- Poor motility in left, right, and up gaze
- Alternating esotropia with and without current specs
- Best corrected visual acuities were 20/60 OD and 20/30 OS.
- Dilated fundus examination revealed blurred disc margins and hemorrhaging of both optic nerves.
Figure 1: MRI of brain with pineal germinoma, sagittal view
Figure 2: Bilateral papilledema
TREATMENT PLAN: Bilateral papilledema in the presence of Parinaud syndrome is highly suggestive of a lesion of the dorsal midbrain. This patient was referred for imaging STAT. MRI confirmed a mass of the midbrain. Craniotomy was performed to place a shunt in order to relieve excess cerebrospinal fluid. The mass was found to be a germinoma of the pineal gland and was positive for cancer. Aggressive treatment of the cancer will include chemotherapy followed by radiation.
IMPACT ON PATIENT’S LIFE: The location of the tumor was causing obstructive hydrocephalus which can be fatal. By making the appropriate diagnosis and swiftly putting the plan into action, a life was saved. Furthermore, cancer was detected and may be appropriately treated.
Case Study 2: Type 1 Chiari Malformation
BACKGROUND: 12-year-old male patient presented for examination. He had been examined six months prior for a complete exam with unremarkable findings.
CHIEF COMPLAINT: Blurry vision OU x three days, persistent horizontal diplopia, constant, worsening occipital headache with onset concurrent with blurry vision.
CASE FINDINGS:
Examination revealed comitant eso deviation OS of magnitude 14 prism diopters and bilateral optic nerve head edema, grade 3 OD, OS on the modified Frisen scale.
TREATMENT PLAN: Patient was referred for STAT MRI of brain/orbits with differential diagnoses of space occupying lesion, cavernous sinus syndrome, and idiopathic intracranial hypertension. Sagittal view MRI with weighted T1 contrast revealed 5 mm downward displacement of the cerebellar tonsils through the foramen magnum and into the cervical spinal column. This led to a diagnosis of Type 1 Chiari malformation.
Patient was referred to pediatric neurology and underwent successful posterior fossa decompression with duraplasty and tonsillar resection three weeks after initial diagnosis.
Figure 3: MRI of human brain with type 1 Arnold Chiari malformation and herniated cerebellum
Figure 4: Mata OS before (left) and after (right)
Figure 5: Mata OD before (left) and after (right)
IMPACT ON PATIENT’S LIFE: Chiari malformation is an often-congenital cerebellar malformation that can cause severe neurological deficits in patients. Type 1 (of four classifications) is the only classification that affords the potential for a normal life. Had the underlying cause of the patient’s symptoms not been identified within a timely matter, irreversible damage to the cerebellum could have occurred. The secondary increased intracranial pressure (from cerebellar tonsil position within the spinal column) could have led to seizures, stroke, neurological damage, or death if the underlying cause was not identified.
Case Study 3: Malignant Hypertension, Stage 3 Hypertensive Retinopathy, and BRVO
DOCTOR: ASHLEY KADAKIA, OD
Redwood Sage, PC
Practices at an America’s Best Contacts & Eyeglasses location in San Jose, CA
BACKGROUND: 50-year-old female presented for examination. She denied any remarkable medical history and stated she had never had a complete eye exam with dilation.
CHIEF COMPLAINT: Patient complains of mild blur at distance and near without glasses and wants contact lenses. She reports being very healthy because she does not feel any pain or unusual symptoms. She only wants a spectacle Rx and prefers not to be dilated.
CASE FINDINGS:
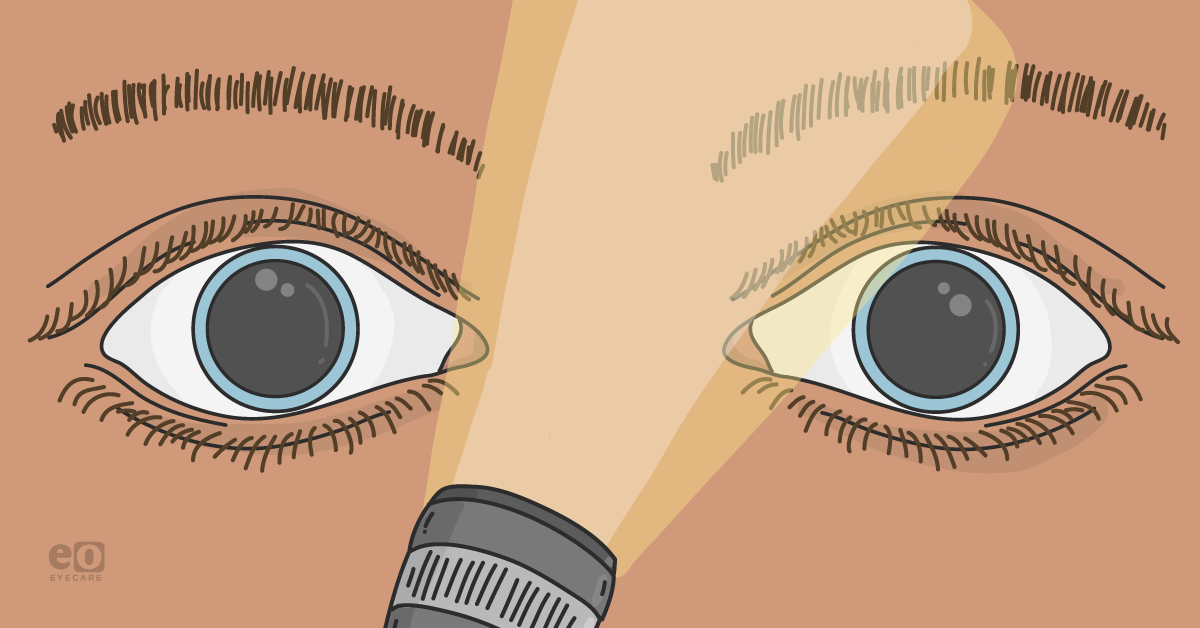
- Pupils: ERRL (-)APD
- EOMs: SAFE
- FDT: 1 defect inferior nasal OD, wnl OS
- BCVAs: 20/20 OD, OS
- Anterior segment: Unremarkable
- IOP: Normal tension range OU
Fundus exam revealed scattered flame hemorrhages, exudates, and BRVO inferior to the optic nerve OD, with nicking and banking of blood vessels OS. There was no pallor/edema of the optic nerve heads. The patient’s blood pressure in office was 202/123 left arm sitting.
Figure 6: HTN OD and HTN OS
After further discussion and probing and questioning of medical history, the patient mentioned she had high blood pressure before but does not measure it at home. She is not taking any medications for hypertension as she prefers natural remedies such as exercise and diet.
TREATMENT PLAN: Deferred spectacle Rx. Patient was directed to ER immediately.
FOLLOW-UP: After calling the patient that evening, the patient reports immediate intervention at the ER to lower blood pressure over the course of several hours, and was given antihypertensive medication for the remainder of the month.
IMPACT ON PATIENT’S LIFE: This patient presented to her eye exam without any idea of the state of her medical condition. She was reluctant to even believe clinical findings. Fortunately, with the assistance of fundus photography, she was able to observe exactly what those findings were for herself. She reported that this examination was truly eye-opening, and did not know she could have health problems without symptoms, and had no idea what the eyes can reveal about the body.
Case Study 4: Intracranial Brain Aneurysm
DOCTOR: JOSH ROGERS, OD
Buckeye State Optometry Associates, P.C.
Practices at an America’s Best Contacts & Eyeglasses location in Macedonia, OH
BACKGROUND: 52-year-old, female
CHIEF COMPLAINT: Routine eye exam. She reported mildly decreased vision and wanted to get back into contacts.
CASE FINDINGS: All entrance testing normal, with insignificant vision changes from when she was seen about a year ago. Fundus examination revealed optic nerve edema OD. This patient was sent to the Cleveland Clinic Emergency Room for CT scan/MRI STAT.
Figure 7: Optic Nerve Edema
TREATMENT PLAN/FOLLOW-UP: After 3-4 months, the patient returned for follow up. She had been in and out of the hospital for the past few months. She went to the ER for her MRI and they found a large brain aneurysm that was close to bursting. She had emergency surgery later that same day and underwent surgical clipping, during which they had to remove the upper right 1/4 of her skull to get to the aneurysm and clip it off.
After surgery, the patient had run out of contacts and said she was tired of wearing her old glasses at the hospital, but couldn’t make it in to see me. I got her trials and finalized her prescription. Before she left she hugged me and thanked me for saving her life. In the fall she came in for an ocular allergy issue at which she was doing much better! I saw her back for her full exam in March and she was noticeably continuing to improve.
IMPACT ON PATIENT’S LIFE: Likely saved her life.
These are just some examples of life saving or altering interventions resulting from eye examinations. In some cases, patients were asymptomatic; in others, patients had a distinct complaint. Regardless, one of the greatest things about the profession of optometry is that we can and do in fact make massive differences in our patients’ lives.
From providing excellent vision with glasses or contact lenses, to saving a patient’s life, it is hard to find a more rewarding and dynamic profession!
This is a sponsored post by National Vision, a supporter of NewGradOptometry & new graduate optometrists! 😎 Free eBook: The Guide to Understanding National Vision Career Options!
In this beautifully illustrated eBook, you'll find commentary and resources that will help you understand the career options, growth opportunities, and a typical workday for ODs practicing within the National Vision Doctor of Optometry network.
View new National Vision optometry job openings near you: