In the current pandemic, lifestyle modifications have impacted our everyday lives. We are constantly reminded to sanitize our hands, disinfect surfaces, and social distance, to name a few. The pandemic is also changing the dynamics of a contact lens examination, especially in a
specialty contact lens practice.
Multipatient contact lens protocol
Multipatient-use diagnostic contact lenses are permitted to be used on more than one person. These lenses must be disinfected prior to storage and use on another patient. There is the possibility of transferring potential pathogens from one patient to another when reusing diagnostic contact lenses on multiple patients in practice. These pathogens may be introduced into the system from one patient to another or may be transferred by the practitioner or staff during handling and storage or both.
Pathogens can cause acute or chronic infection that can lead to significant ocular morbidity (temporary or permanent), including vision loss. According to the new Guidelines for Handling of Multipatient Contact Lenses in the Clinical Setting, contact lenses are divided into three categories for disinfection purposes:
- Soft contact lenses (hydrogel) include silicone hydrogels and hydroxyethyl methacrylate (HEMA) hydrogels.
- Gas Permeable (GP) contact lenses include corneal and scleral lenses.
- Hybrid contact lenses (composite) are composed of a GP center with a hydrogel periphery.
For individuals with transmissible infections, contact lenses must be disposed immediately after use.
These infections include hepatitis, HIV, Prion disease, ocular herpetic infection, adenovirus, and
acanthamoeba keratitis. It is common to assess visual potential over a corneal scar secondary to ocular infection with a diagnostic lens.
All diagnostic contact lenses used in individuals who are carriers (or identified as potential carriers) of infectious diseases must be disposed of instantly after use. These organisms either have potential sustained survival outside the host,2 ocular reservoirs with theoretical risk of transmission,3-6 latency7 or encystment,8 or persist detectable in tears despite an otherwise quiet host.9, 10 For active bacterial and fungal ocular infections, the lens must be disposed.
When fitting over inactive corneal scars without signs of infection or inflammation after bacterial and fungal keratitis, the contact lens may be used, and disinfection procedures should be followed.
All contact lenses should be rubbed with a daily surfactant cleaner according to the manufacturer instructions to clean, not disinfect, contact lenses. The cleaner is used to remove particulate matter, deposits, and debris from contact lenses to ensure more effective disinfection.
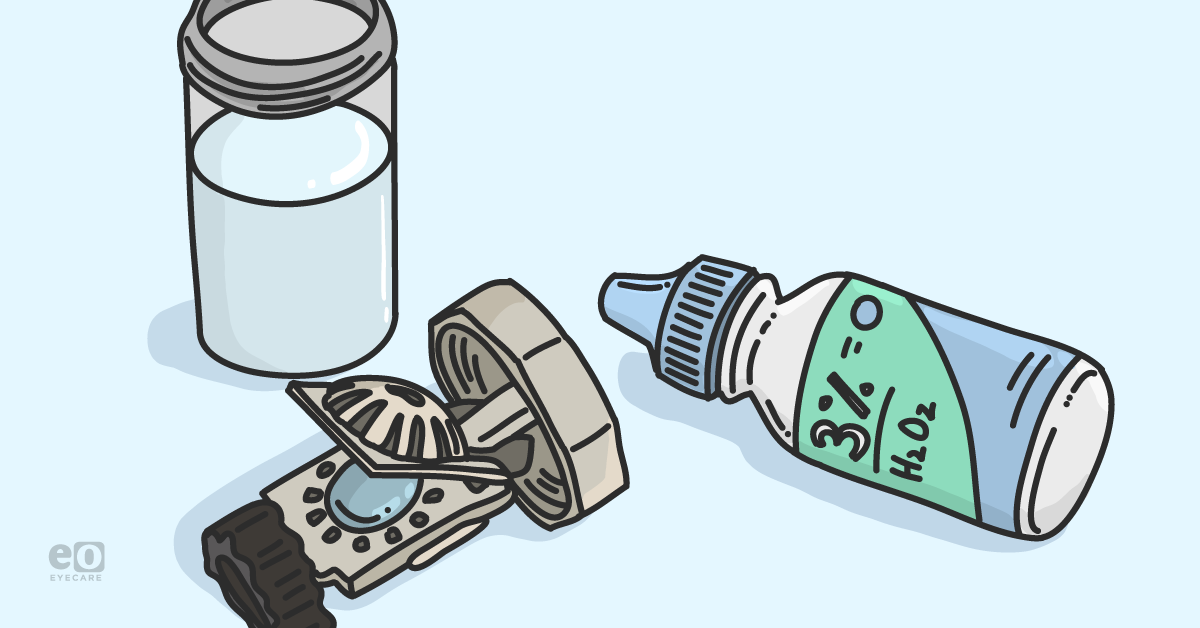
Next, diagnostic lenses are soaked in non-neutralized ophthalmic grade 3% hydrogen peroxide solution for a minimum of three hours.1 Finally, the lenses are neutralized by rinsing with sterile saline or multipurpose solution and then stored dry in a disinfected case.
A contact lens storage case can be a reservoir of microbial contamination. To ameliorate risk, avoid putting used or soiled lenses directly back into the original storage container after removal from the eye. It is recommended to place lenses in a disposable container until disinfection is complete.
Disinfection of lens containers is critical
Since microbial contamination and biofilm formation increase over time, replace the lens container whenever possible. The disposable plastic / rubber stopper in a glass bottle should be disinfected with non-neutralized ophthalmic grade 3% hydrogen peroxide for a minimum of three hours and rinsed with saline or multipurpose solution before reuse or replaced with a fresh stopper.
Every lens container should be disinfected with non-neutralized ophthalmic grade 3% hydrogen peroxide for a minimum of three hours and then rinsed thoroughly with a multipurpose solution or saline. Glass contact lens storage cases may be disinfected using moist heat disinfection at 134°C for 3 minutes or 121°C for 15 minutes.1
Lens containers should be labeled with a lens identification number (if there are multiple lenses with the same parameters), lens material, and lot number. And, if available, label with the date of last disinfection and lens parameters, including lens design, power, diameter, curvature, and additional parameters specific to the lens design. If the lens and containers are stored wet, they must be redisinfected, and the storage solution should be replaced every 28 days.
In addition, the 2018 ISO Standards suggest documenting each contact lens disinfection and maintaining a record for each diagnostic fitting set. The record should include the reference number for each lens, the patient reference for each lens, date(s) of use, date(s) of disinfection, method of disinfection (e.g., peroxide or moist heat), and the person performing disinfection. This record could be helpful if an infection was present during the fitting to inform subsequent patients fit with the diagnostic lens to advise of potential risks of infection.
Ideally, diagnostic contact lenses would be used a single time and then either discarded or dispensed to an individual. If reuse of the contact lens is necessitated, moist heat management is preferred over chemical management when applicable per the 2018 ISO Standards.
Conclusion
Practitioners must take every precaution to reduce multipatient contact lens transmission of disease by educating themselves and their staff on best practices for disease control. This includes the practices of hand washing; gloving; disinfection of instruments, contact lenses, and storage cases; and management of in-office contact lens solutions. If empirical fitting is an option based on the patient's individual needs, empirical fitting without the use of a trial lens is suggested.
A quick reference guide (below) is helpful for the contact lens practice when disinfection of diagnostic lenses is required.
References
- Sindt C, Bennett E, Szczotka-Flynn L, Sclafani L, Barnett M; American Academy of Optometry (AAO) Section on Cornea, Contact Lenses & Refractive Technologies, and The American Optometric Association (AOA) Contact Lens and Cornea Section. Technical Report: Guidelines for Handling of Multipatient Contact Lenses in the Clinical Setting [published online ahead of print, 2020 Aug 6]. Optom Vis Sci. 2020;10.1097/OPX.0000000000001547. doi:10.1097/OPX.0000000000001547
- Gordon YJ, Gordon RY, Romanowski E, et al. Pro- longed Recovery of Desiccated Adeno-viral Serotypes 5, 8 and 19 from Plastic and Metal Surfaces in Vitro. Ophthalmology 1993;100:1835–9.
- Armstrong RA. Creutzfeldt-Jakob Disease and Vision. Clin Exp Optom 2006;89:3–9.
- Fujikawa LS, Salahuddin SZ, Ablashi D, et al. HTLV- III in the Tears of AIDS Patients. Ophthalmology 1986; 93:1479–81.
- Cantrill HL, Henry K, Jackson B, et al. Recovery of Human Immunodeficiency Virus from Ocular Tissues in Patients with Acquired Immune Deficiency Syn- drome. Ophthalmology 1988;95:1458–62.
- Gastaud P, Baudouin C, Ouzan D. Detection of HBS Antigen, DNA Polymerase Activity, and Hepatitis B Virus DNA in Tears: Relevance to Hepatitis B Transmission by Tears. Br J Ophthalmol 1989;73: 333–6.
- Gamus D, Romano A. Herpetic Imprint on Privileged Areas of Its Target Organs: Local Latency and Reactivation in Herpetic Keratitis. Metab Pediatr Syst Ophthalmol (1985) 1988;11:37–40.
- Schaap P, Schilde C. Encystation: The Most Prevalent and Underinvestigated Differentiation Pathway of Eukaryotes. Microbiology 2018;164:727–39.
- Han Y, Wu N, Zhu W, et al. Detection of HIV-1 Vi- ruses in Tears of Patients Even under Long-term HAART. AIDS 2011;25:1925–7.
- Komatsu H, Inui A, Sogo T, et al. Tears from Children with Chronic Hepatitis B Virus (HBV) Infection Are Infectious Vehicles of HBV Transmission: Experimental Transmission of HBV by Tears, Using Mice with Chimeric Human Livers. J Infect Dis 2012; 206:478–85.