The chronicity and progressive nature of glaucoma makes new treatment modalities in our armamentarium needed and welcomed. Many patients with glaucoma will endure multiple treatment types to lower intraocular pressure (IOP) including, drops, laser, surgery, and most recently drug delivery. Drug delivery is a hybrid option that leverages powerful pharmacologic molecules in an extended-release fashion to lessen the burden of patient compliance. Like many areas in glaucoma, drug delivery is evolving at a rapid pace, and optometry should be armed to collaborate in this care. This review aims to cover the currently available options and preview future therapies completing in clinical trials.
Bimatoprost Implant (Durysta-Allergan)
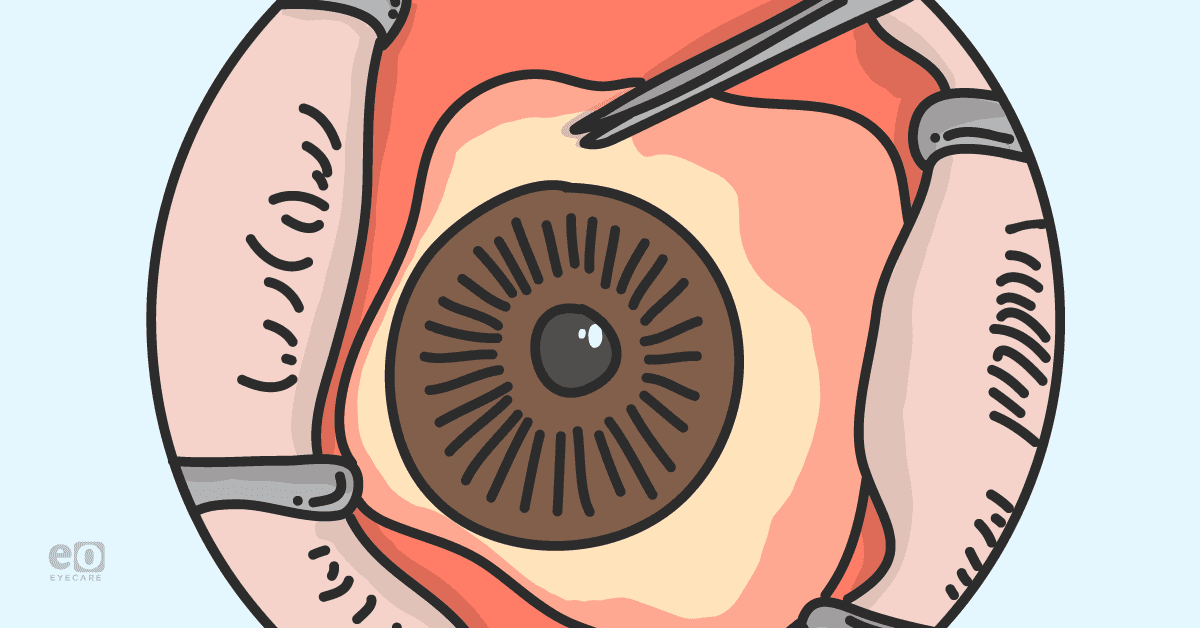
Currently, the only FDA-approved glaucoma drug delivery device is a 10 mcg bimatoprost implant (Durysta). This implant is indicated for the reduction of intraocular pressure in patients with open angle glaucoma or ocular hypertension. The implant is placed into the anterior chamber using a sterile applicator with a preloaded implant and a 28-gauge needle.1 It is 1 mm in Iength, biodegradable, preservative-free, and delivers drug intracamerally for up to 4 months.1
A recent Phase III (ARTEMIS) clinical trial demonstrated 5 to 8 mm Hg IOP reduction over a 15 week period from a mean baseline IOP of around 24.5 mm Hg.1 This IOP reduction equaled up to a 31-32% mean IOP from baseline.1 Reported adverse events were minimal with no patients suffering from endophthalmitis, 27.4% demonstrating conjunctival hyperemia, and 5.4% of patients have reported corneal endothelial cell loss.1
Travoprost Intraocular Implant (iDose TR - Glaukos)
Currently, in clinical trials, this 1.8 x 0.5 mm biocompatible titanium implant releases a proprietary formulation of travoprost inside the anterior chamber.2 The implant is implanted into the trabecular meshwork using an ab interno approach in an operating room. It consists of three parts: a scleral anchor that affixes into the trabecular meshwork, the body that serves as the drug reservoir, and the elution membrane that titrates travaprost release.2 A Phase 2 clinical trial including 154 patients has revealed an average IOP reduction from baseline of 7.9 mmHG (a 29% decrease) in the fast elution arm and a 7.4 mmHG (a 28% decrease) in the slow elution arm at 24 months.3
Microdose Latanoprost (EyeNovia)
A device delivering a micro-dose of latanoprost uses 75% less drug and preservative while maintaining efficacy.4 Patients self-administer the micro-dose of latanoprost and according to a Phase 2 clinical trial were successful in doing so 88% of the time compared to less than 50% of the time with standard drops.4 The micro-dose demonstrated a 29% drop in IOP from baseline, consistent with the average of 26% decrease that conventional latanoprost eye drops have shown.4 Phase 3 clinical trials are ongoing.
Sustained-Release Depot
Optometrists use punctal plugs daily to manage ocular surface disease, so it only makes sense to utilize this type of technology to deliver medication to the ocular surface to manage glaucoma. Two intracanalicular inserts are undergoing clinical evaluation.
OTX-TP (Ocular Therapeutix)is a resorbable, preservative free, intracanalicular that delivers travoprost to the ocular surface for 90 days.5 In a phase 3 clinical trial, the insert did lower IOP between 3.27 mm Hg and 5.27 mm Hg in patients with primary open-angle glaucoma or ocular hypertension.5
A L-shaped punctal plug utilizing both a latanoprost and travoprost core (Evolute, Mati Therapeutics) is designed to create a unidirectional flow into the tear film to reduce systemic absorption of the drug.6 A phase 2 clinical trial utilizing the L-shaped insert with latanoprost showed a 20% reduction in IOP at 3 months with 92% retention.6
Drug-Eluting Contact Lenses
Drug-eluting contact lenses are an attractive option to deliver medication due to their large residence time on the eye and upward of 50% bioavailability in comparison with eye drop formulations.7,8 Challenges still exist such as patient compliance, prescription in the lenses, ocular surface disease issues, and replacement schedules.
Multiple drug-eluting contact lenses are in phase 1 and 2 clinical trials. These contact lenses are utilizing approved drugs such as latanoprost and bimatoprost along with patented drug-eluting processes to lower IOP. Certain studies have reported IOP-lowering effects that last longer than conventional eye drops, suggesting less frequent administration may be possible.
Travoprost Intracameral Implant (OTX-TIC – Ocular Therapeutix)
An intracameral implant providing a steady release of travoprost has demonstrated favorable results in a phase 1 clinical trial.9 The implant is injected into the anterior chamber, is bioresorbable, and releases travoprost with a target duration of 4 to 6 months.9 In the phase 1 clinical trial, a total of 19 patients, obtained a mean reduction in IOP from baseline of 7-11 mmHg with onset of action as early as 2 days after insertion.9 No serious adverse events were noted along with no meaningful changes in endothelial cells counts across the 19 patients.9
Bringing new tools to glaucoma drug delivery
Any treatment in glaucoma that provides high safety, good efficacy, and increases patient convenience will be accepted. Candidacy for glaucoma drug delivery can really span a wide range of patients starting with anyone who needs IOP lowering.
More specifically, the above treatments employ prostaglandin analogues (PGAs), and patients with aggressive allergic side effects, active uveitis, or current macular edema should be excluded. As more options become available in drug delivery, practitioners can balance insertion effort and risk versus treatment duration.
Patient education will be key because surveyed patient preference still favors drops, and the word surgery can induce anxiousness. In our practice, patient experiences have been very positive with a recurring theme of, “I no longer forget to take my drops.” After a patient concludes drug delivery in glaucoma is right for them, communicating in the referral you want to collaborate in continued glaucoma care is key.
An important pearl to remember for doctors and patients is that these devices can’t cure glaucoma, so follow-up with continued ancillary testing is needed.
Doctors who embrace glaucoma drug delivery have another tool that minimizes the major hurdle of patient non-compliance. Drug delivery is here to stay and adding these devices to our toolbox in glaucoma further diversifies how we care for patients.
References
- Medeiros FA, Walters TR, Kolko M, et al; ARTEMIS 1 Study Group. Phase 3, randomized, 20‐month study of bimatoprost implant in open‐angle glaucoma and ocular hypertension (ARTEMIS 1) [published online ahead of print June 13, 2020]. Ophthalmology. doi: 10.1016/j.ophtha.2020.06.018.
- Ibach M. Interim results of a prospective phase II study of travoprost intraocular implants. Paper presented at: the American Academy of Optometry Annual Meeting; November 9 2018; San Antonio, Texas.
- http://investors.glaukos.com/investors/press-releases/press-release-details/2021/Glaukos-iDose-TR-Demonstrates-Sustained-IOP-Reduction-and-Favorable-Safety-Profile-Over-24-Months-in-Phase-2b-Study/default.aspx. Accessed May 23 2021
- Pasquale LR, Lin S, Weinreb RN, Tsai JC, Kramm RL, Ianchulev T. Latanoprost with high precision, piezo-print microdose delivery for IOP lowering: clinical results of the PG21 study of 0.4 µg daily microdose. Clin Ophthalmol. 2018 Nov 28;12:2451-2457. doi: 10.2147/OPTH.S185027. PMID: 30568423; PMCID: PMC6276603.
- Srilatha Vantipalli, Kenneth N Sall, Emil Stein, Howard Schenker, Jay Mulaney, Robert Smyth-Medina, Douglas Day, Robert Benza, El-Roy Dixon, Nicole Rissman, Jamie Lynne Metzinger, Michael H Goldstein; Evaluation of the Safety and Efficacy of OTX-TP, an intracanalicular travoprost insert, for the treatment of patients with open-angle glaucoma or ocular hypertension: A Phase 3 Study. Invest. Ophthalmol. Vis. Sci. 2020;61(7):3488.
- Blum-Shouchane K, Geffen, N, Zahavi, A.Sustained drug delivery platforms-A new era for glaucoma treatment. Clinical and Experimental Vision and Eye Research. 2019;2:22-29.
- Li, CC, Chauhan, A. Modeling ophthalmic drug delivery by soaked contact lenses. Ind Eng Chem Res 2006; 45: 3718–3734.
- Peng, C-C, Kim, J, Chauhan, A. Extended delivery of hydrophilic drugs from silicone-hydrogel contact lenses containing Vitamin E diffusion barriers. Biomaterials 2010; 31: 4032–4047.
- https://ocutx.gcs-web.com/static-files/7c581c00-f838-44a2-8ad3-03ed5f14f16b. Accessed May 23, 2021