The term ocular surface neoplasm refers to a lesion located on the conjunctiva and/or cornea, and encompasses a wide spectrum of conditions, ranging from benign to malignant.1
Benign entities include pterygium and corneal pannus, which must be distinguished from malignant entities, such as ocular surface squamous neoplasia (OSSN).
Pterygium
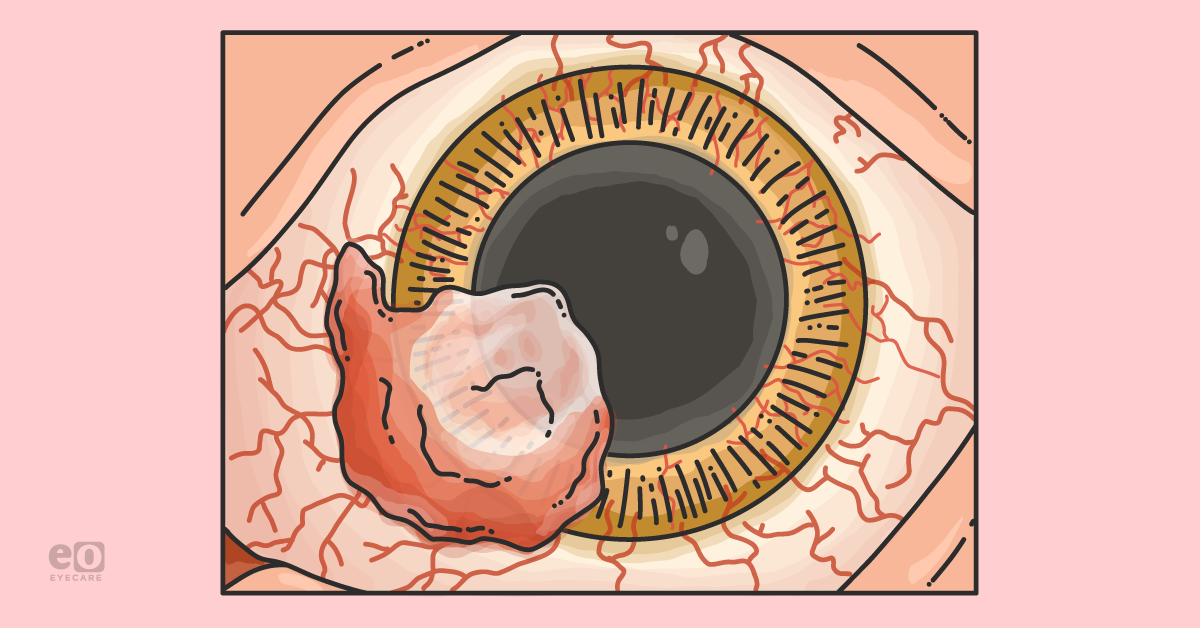
Pterygium is a common and often benign ocular surface lesion with a “wing-shaped” appearance that begins most frequently at the nasal limbus and extends onto the cornea.
2 The prevalence of pterygium ranges from about 1.2% to 40%, with a greater prevalence in regions located near the equator.
3,4 The main risk factor for pterygium is exposure to ultraviolet (UV) light, and it is commonly seen in those who work outdoors or live in tropical climates.4 Other possible risk factors include living in a dry or dusty environment and various viral infections, such as herpes simplex virus (HSV) and human papillomavirus (HPV).3,4
Diagnosing patients with a pterygium
Diagnosis of pterygium is made based on clinical examination findings. Typical features of pterygium include a raised, triangular-shaped, white- to pink-colored conjunctival growth extending from within the palpebral fissure onto the corneal surface. The lesion is characteristically located at 3 o’clock or 9 o’clock, and can be present unilaterally or bilaterally.
Patients with pterygium may be asymptomatic, but in some cases, the lesion can cause
ocular surface irritation when inflamed. In addition, it is possible for pterygia to cause visual disturbances, either by inducing corneal astigmatism or by directly covering the visual axis. Some patients may also dislike the appearance of pterygium and desire removal for cosmetic reasons.
4,5Using imaging to identify a pterygium
Optical coherence tomography (OCT) has been described as a useful tool for confirming the diagnosis of pterygium. Classic features of pterygium on OCT include a mildly hyperreflective, normal to slightly thinned epithelium with a highly hyperreflective subepithelial lesion in the space between the epithelium and Bowman’s layer.
6 The slit lamp photo in Figure 1 shows a pterygium of the left eye that extended onto the cornea nasally at 8 to 10 o’clock.
Figure 1: Courtesy of Anat Galor, MD, MSPH.
In Figure 2, OCT demonstrates a hyperreflective, subepithelial lesion (white arrowheads) with mild epithelial hyperreflectivity and thinning.
Figure 2: Courtesy of Anat Galor, MD, MSPH.
Discerning between benign and malignant lesions
It is possible for benign lesions, such as pterygium, to coexist with malignant lesions, such as OSSN. For example, one
study conducted in South Florida of 2,005 surgically excised pterygia found that 1.7% harbored OSSN.
3Therefore, it is crucial for clinicians to differentiate pterygium from OSSN and be cognizant of the possibility of OSSN existing concomitantly with benign lesions, such as pterygium. It is for this reason that it is recommended to send all excised tissue for histopathologic analysis in order to prevent missing a malignant diagnosis.
Treating a pterygium
Treatment options for pterygia range from conservative management to surgery. Nonsurgical therapies include lubricating eye drops for irritation and short-term usage of topical vasoconstrictors (e.g., Naphazoline HCl 0.025%) or anti-inflammatory agents during periods of inflammation.
Surgical excision is indicated in cases of persistent ocular irritation, documented growth, visual disturbance, or concern for malignancy.4,5
Surgical treatment of pterygium
The two main surgical techniques currently used for pterygium removal are excision with conjunctival autograft (CAG) and excision with amniotic membrane transplantation (AMT), with our preferred approach being CAG.
Literature supports our approach as well. In one
study of 86 eyes with pterygium randomized to CAG (n=42) or AMT (n=44), the AMT group had a significantly greater rate of pterygium recurrence compared to the CAG group (40.9% vs. 4.8%; p<0.007) up to 12 months post-operatively.
7The bare sclera technique is no longer favorable due to recurrence rates as high as 80%.4 Surgical excision may be combined with adjuvant therapies, such as application of mitomycin C (MMC).
We use MMC in individuals with a higher risk of aberrant wound healing after surgery (e.g., young age, inflamed pterygium), taking care to avoid direct contact of MMC with the sclera, which can result in complications such as scleral ulceration and calcification.
Pannus
A
corneal pannus is a benign, subepithelial ingrowth of fibrovascular tissue that appears as a white, vascularized, variably elevated opacity. Pannus extends centrally from the limbus onto the cornea and, in severe cases, can involve the entirety of the cornea for 360°.
8 Causes of pannus include contact lens wear, keratitis, inflammation, and trauma.
9Diagnosing patients with a pannus
The diagnosis of pannus is made clinically based on examination findings. However, it is important to distinguish pannus from malignant entities, such as OSSN, as they can present with overlapping clinical features.
In cases where pannus may be difficult to differentiate from OSSN, OCT has been previously described as a helpful diagnostic tool. Classic features of pannus on OCT include a normal to thin epithelium overlying a flat, hyperreflective subepithelial lesion along Bowman’s layer.10
Utilizing OCT to differentiate between pannus and OSSN
A
retrospective study comparing clinical features and OCT findings between corneal pannus (n=6) and OSSN (n=4) found that clinically, blood vessels often reached the border in pannus (noted in 67% of eyes), whereas this was not the case in OSSN (0% had a vessel that reached the border).
9Additionally, on OCT, none of the pannus cases had epithelial thickening, whereas this feature was seen in 100% of OSSN cases. Finally, the angle of transition between normal and abnormal epithelium was noted to be an important distinction between the two entities.
Specifically, pannus appeared as an angled transition around 45° to Bowman’s layer, whereas OSSN appeared as an abrupt, 90° angle perpendicular to Bowman’s layer.9
Figure 3 illustrates a slit lamp photo of a right, inferotemporal opacity (dashed white line) at 6:30 to 8:30 o’clock with blood vessels that extended to the border (white arrows).
Figure 3: Courtesy of Anat Galor, MD, MSPH.
The OCT image in Figure 4 shows a thin epithelium overlying a hyperreflective subepithelial lesion along Bowman’s layer and an angled (~45°) transition (white dotted line and arrowhead) between normal and abnormal tissue, consistent with pannus.
Figure 4: Courtesy of Anat Galor, MD, MSPH.
Treating a pannus
Treatment of pannus is primarily dependent on addressing the underlying cause. For example, in cases of
contact lens wear, the contact lenses may need to be refitted, such as with rigid gas permeable lenses, or discontinued.
11In severe cases, surgery may be considered.8 However, in cases where the pannus is stable and there is no visual disturbance, the lesion can be monitored over time.
Ocular surface squamous neoplasia
Ocular surface squamous neoplasia encompasses a spectrum of squamous epithelial malignancies involving the cornea or conjunctiva, ranging from mild dysplasia, to non-invasive intraepithelial neoplasia, to invasive squamous cell carcinoma.
12 Occurring primarily in elderly white males, OSSN is the most common non-melanocytic tumor of the ocular surface.9,13 Various risk factors have been implicated in the development of OSSN, including UV light exposure, immunosuppression, and genetic predisposition (e.g., xeroderma pigmentosum).12
Diagnosing OSSN
OSSN presents as a variably elevated, white or grey opacity with irregular borders, vessel abnormalities (e.g., hairpin loop, feeder vessels), and a leukoplakic, gelatinous, or papilliform appearance.9,12
Along with clinical characteristics, OCT has been described as a useful tool for the diagnosis of OSSN.
Classic features of OSSN on OCT include epithelial hyperreflectivity, epithelial thickening, and an abrupt (90°) transition from normal to abnormal epithelium.
14Discerning between OSSN and pterygium with ophthalmic imaging
Specifically, when differentiating between OSSN and pterygium, an epithelial thickness cut-off of 120 to 140μm has been previously found to have a sensitivity of 94% to 100% and a specificity of 100%.6,15
In addition,
in vivo confocal microscopy has been investigated as a noninvasive imaging tool for the diagnosis of OSSN due to its ability to reveal abnormal squamous epithelial cell number and morphology, but it is less commonly used in clinical practice.
16 However, excisional biopsy with histopathological examination remains the gold standard for the diagnosis of OSSN.
17The slit lamp photo in Figure 5 captures a right, inferotemporal, opalescent lesion at 7 to 9:30 o’clock with irregular borders (dashed white line) and vascularization that did not reach the edges (white arrows).
Figure 5: Courtesy of Anat Galor, MD, MSPH.
The OCT image in Figure 6 shows a hyperreflective and thickened epithelium with an abrupt, vertical (90°) transition (white dotted line and arrowhead) between normal and abnormal epithelium, consistent with ocular surface squamous neoplasia.
Figure 6: Courtesy of Anat Galor, MD, MSPH.
Medical treatment of OSSN
Treatment of OSSN includes medical therapy with topical chemotherapeutic agents and surgical excision. In particular, three common medical treatment options are 5-fluorouracil (5FU), interferon alfa-2b (IFN-2b), and MMC.18
Our first line agent is 5FU, as IFN-2b is no longer available in the United States, and MMC has the least favorable side effect profile of the three agents. Side effects that are seen more frequently with MMC include redness, pain, corneal erosion, punctal stenosis, and limbal stem cell deficiency.
Comparing the various medical treatment options for OSSN
In a
study comparing the efficacy of topical 5FU (n=54) and IFN-2b (n=48) for the treatment of OSSN, the frequency of resolution was greater with 5FU versus IFN-2b (96.3% vs. 81.3%; p=0.01); however, this difference did not remain significant in a multivariable analysis.
Time to resolution (6.6±4.5 vs. 5.5±2.9 months; p=0.62) and recurrence frequency are generally similar between 5FU and IFN-2b. Of note, 5FU does have a less favorable side effect profile, with tearing (22.2% vs. 4.3%; p=0.02) and eyelid edema (9.3% vs. 0%; p=0.04) more frequently noted in comparison to IFN-2b.19
However, most patients tolerate 5FU therapy well. We use a topical corticosteroid in cases of 5FU-associated conjunctival inflammation and recommend petroleum jelly on the skin around the eye in individuals who develop contact dermatitis. Although rare, we advise patients to occlude their puncta after 5FU application to minimize the risk of punctal stenosis.
Surgical treatment of OSSN
If an excision biopsy is performed, the technique for surgical excision involves a “no-touch” technique with wide margins of 3 to 4mm.
18 In a
study of 389 OSSN lesions excised using the “no-touch” technique, the 1-year and 5-year recurrence rates were 10% and 21%, respectively.
21Factors associated with an increased risk of tumor recurrence after surgical excision included a previous history of OSSN (hazard ratio [HR]: 2.32; p=0.03), superior location (HR: 3.33; p=0.003), tarsal involvement (HR: 4.12; p=0.007), papillomatous appearance (HR: 1.95; p=0.04), and positive surgical margins (HR: 2.73; p=0.008).
The risk of tumor recurrence was found to be decreased with treatment with adjuvant cryotherapy (HR: 0.51; p=0.03). Additionally, in patients with positive margins, the usage of post-operative topical IFN-2b was found to reduce recurrence to a similar rate as in patients with negative margins.21
Differences between medical and surgical treatments for OSSN
When comparing medical therapy with topical IFN-2b (n=49) to surgical excision (n=49), the 1-year and 5-year recurrence rates were found to be similar between the groups (3% vs. 5% and 25% vs. 11%; p=0.80).22 Adverse effects, including pain, irritation, itching, and redness, were also not significantly different when comparing medical therapy and surgical excision.22
Overall, we prefer medical therapy for the treatment of OSSN, but consider surgical excision when the lesion is small enough (<4 clock hours of limbal involvement) that the risk of subsequent limbal stem cell deficiency is low.
Conclusion
Due to the possibility of malignant lesions, such as OSSN, masquerading as benign lesions, such as pterygium and pannus, clinicians must distinguish between the various ocular surface neoplasms.
Diagnostic tools, such as OCT, can be invaluable in identifying features that may raise suspicion for malignancy, lending to proper evaluation and management of ocular surface lesions.