While white cataracts can offer several surgical challenges, these cases are often very gratifying and life changing for our patients. The term “white cataract” describes an opalescent, mature lens (Image 1). There are many different subtypes of white cataracts, including fluffy acute diabetic cataracts, hypermature brunescent cataracts, liquified cortical cataracts, and traumatic cataracts.
Image 1
White cataracts: setting patient expectations
When a patient presents for their initial consultation with a white cataract, it is crucial to set realistic vision expectations. Looking closely at the other eye (assuming there is a posterior view) for signs of typically bilateral disease can be helpful. A B scan is necessary for setting these expectations and looking for evidence of
retinal detachment, masses, vitreous opacity, or optic nerve cupping that may ultimately impact the patient’s final visual outcome.
For white cataracts with liquified cortex and an anterior capsule that may be pressurized, a thin slit beam over the anterior capsule can often be revealing. A subtle curve along the anterior capsule may be evident for these pressurized lenses. Looking for a gap between the anterior lens plane and the iris may be evidence of some zonular loss, which can also add extra complexity to the case.
White cataracts in the operating room
It is vital to prepare for
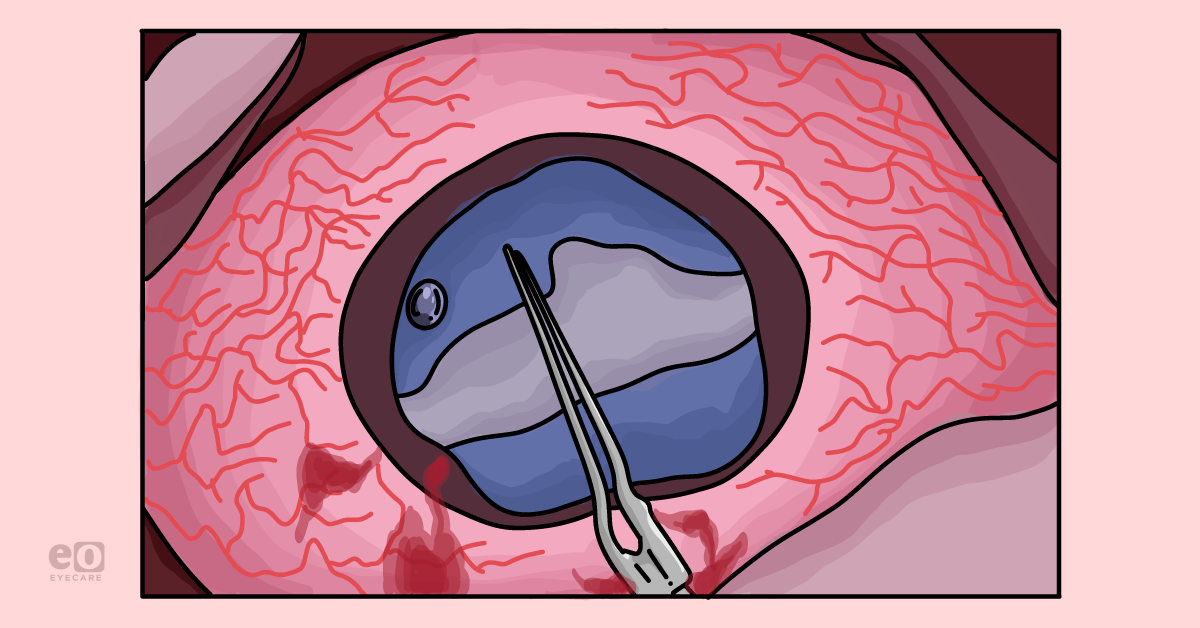
several possible complexities of white cataracts in the operating room. Making the capsulorhexis is often the most challenging aspect of the case. I always use trypan blue to stain the anterior capsule to ensure adequate visualization (Image 2).
Image 2 illustrates the use of trypan blue to aid in the visualization of the anterior lens capsule.
Image 2
I then use a cohesive viscoelastic to flatten the anterior capsule as much as possible. Keeping the anterior chamber pressurized before the first incision into the anterior capsule is crucial to decrease the chance of an anterior capsule running out and the dreaded Argentinian flag sign when the anterior capsule tears out across the lens diameter, with possible posterior capsule extension.
I use a 30 gauge needle on a syringe to make a central stab incision into the capsule through the paracentesis incision. At the same time, I quickly aspirate any liquified cortical contents, thereby decompressing the lens and further flattening the anterior capsule before creating the rhexis.
For hypermature lenses with liquified cortex, cortical ‘milk’ will follow this incision, and the goal is to aspirate enough of it to decrease anterior capsular pressure. For non-liquified cases, this stab incision is a non-event and will be used to start my capsulorhexis.
I then make my main corneal incision using a keratome and proceed with my capsulorhexis using a bent cystotome and Utrata forceps. While the needle decompression technique helps relieve much of the risk of running out, there still may be some peripheral bowing of the capsule, so I start making a rhexis on the smaller side, knowing that I can spiral it out into a larger diameter as I gain further control.
The Little Technique, of applying perpendicular traction to the edge of a rhexis that is running out, can be helpful to save a rhexis under pressure. Viscoelastic is your friend, and generous reapplication of a cohesive viscoelastic can help re-flatten your anterior capsule working space and aid in the completion of a successful continuous curvilinear rhexis.
The
femtosecond laser can be a helpful adjuvant in creating a capsulorhexis for white cataract cases. Given the laser is able to create a rhexis within seconds, it is often able to overcome any anterior capsular pressure that can result in an anterior capsule tear out.
However, I still recommend using trypan blue dye to visualize the anterior capsule cap before proceeding in the case, as there is a possibility of having an incomplete rhexis formed by the laser. Any capsular tags are removed before proceeding with the rest of the case.
Argentinian flag signs: Avoiding anterior and posterior capsule compromise
Sometimes, despite every effort to avoid it, an Argentinian flag may be inevitable (Image 3). I have had this complication develop from the 30G needle stab incision alone. It is vital to have a plan to address this complication should it arise.
Image 3 demonstrates the Argentinian flag sign.
Image 3: photo courtesy of Alexander Robin, MD
I still decompress if there is milky cortical material with the 30G needle. Then I make my clear corneal main incision. To form a rhexis, either a bent needle cystotome or MST scissors followed by a utrata may be used to create a rhexis (Image 4). Thus I have enough room to crack the nucleus and proceed with phacoemulsification successfully.
In Image 4, utrata forceps are used after MST forceps to create a rhexis in the setting of an Argentinian flag.
Image 4: photo courtesy of Alexander Robin, MD
Hydrodissection is important even when there is an Argentinian flag sign or other anterior capsule compromise, as the cortical material can sometimes be sticky and challenging to pull out of the capsule without it.
Suppose there is an early concern for posterior capsule tear. In that case, dispersive viscoelastic may be used to visco-dissect the lens while offering a buffer of protection between the posterior capsule or any opening into the vitreous cavity. Lowering the bottle height and maintaining a stable anterior chamber, with generous use of dispersive viscoelastic, is important to decrease the risk of an anterior capsular tear extending posteriorly.
Phacoemulsification can be performed per surgeon preference, with chopping techniques often preferred due to less zonular stress. An occasional brunescent large nucleus may not be amenable to phacoemulsification, so being prepared to convert to extracapsular or manual small incision cataract surgery may occasionally be necessary for advanced brunescent cataracts.
Final steps and clinical pearls
Once it is time for cortex aspiration, it is essential to remember that these cases often have stretched-out and ‘floppy’ capsular bags. Zonular dialysis may also be encountered here, especially in the setting of trauma. Capsular segments or capsular tension rings should be placed at the first sign of any zonular dialysis to ensure a successful case.
A side-to-side sweeping of cortical material, as opposed to perpendicular force, can be more zonule-friendly.
Once cortical material has been removed, a standard one-piece lens may be placed in the intact capsular bag. In the setting of an Argentinian flag, if there is no posterior capsule extension, a one-piece lens may still be placed in the bag.
However, I typically set a three-piece lens in the bag or with reverse optic capture in these cases of future trauma or lens instability as there are more options for lens refixation with three-piece implants.
In summary, I recommend having the following available in your operating room for white cataract cases:
- Trypan blue
- 30 gauge needle
- Cohesive viscoelastic
- Dispersive viscoelastic
- Capsular hooks
- Capsular tension rings or segments
- Anterior vitrectomy
Best of luck with your future cases!