The visual pathway is a circuit of complexity that contains various changes in direction as light information travels from the outside world to the visual cortex. Lesions can occur along the pathway, resulting in various visual field defects. This article will discuss the components of the visual pathway and the types of defects that may result from a lesion along the pathway.
Visual fields
To understand the visual pathway, it is important to understand the visual and retinal fields of the eye. The visual field is defined as the region of space that the eye can see looking straight ahead when there is no movement of the head involved.1 A vertical line divides the visual field into a left and right half; a horizontal line divides the hemifields into superior and inferior sections.
At this point, the field is split up into four quadrants, right and left superior, and a right and left inferior quadrant. The point of intersection of the two lines is known as the fixation point, where the fovea is located. Similarly, the retinal field can be divided similarly to the visual field. In this case, a vertical line divides the field into a nasal and temporal hemiretina, and a horizontal line again produces superior and inferior halves. The point of intersection marks the center of the fovea.1
Objects seen in the visual field are right-left reversed and inverted onto the retina; for example, objects present in the left half of the visual field of the left eye project to the nasal hemiretina, whereas objects present in the right half of the visual field of the left eye project to the temporal hemiretina.1 The same relationship follows for the right eye.
Additionally, both retinae can see the center portion of the visual field for both eyes, also known as the binocular visual field.1
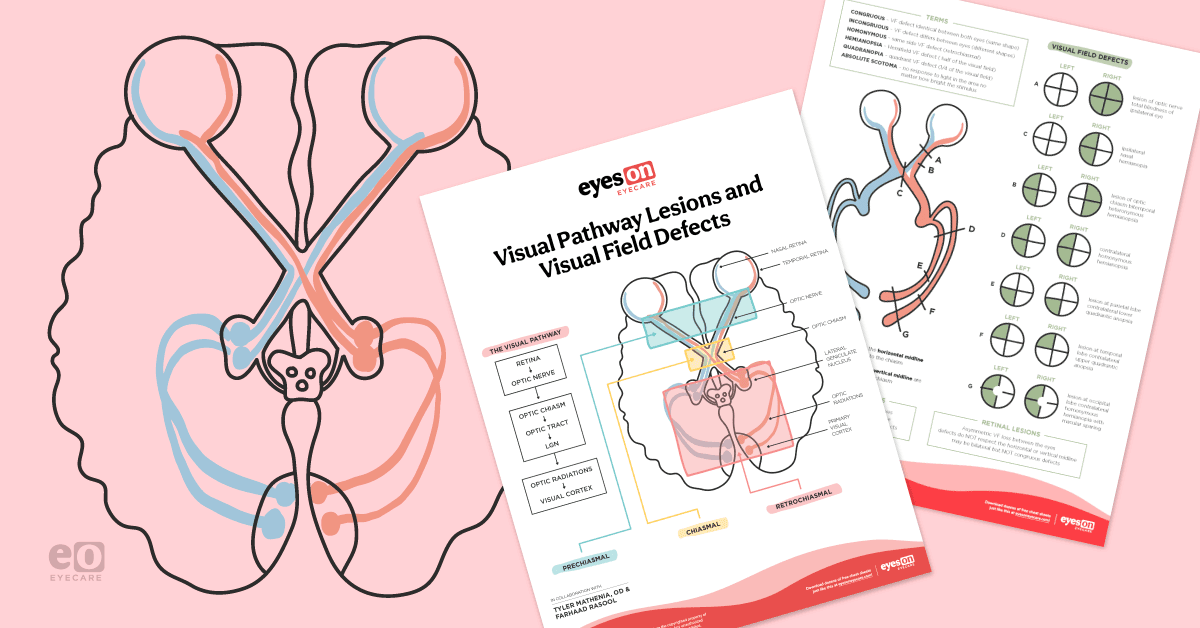
Download the illustrated cheat sheet now!

Visual Pathway Lesions and Visual Field Defects Cheat Sheet
Get ready for easy referencing with this illustrated guide!

Visual pathways
Continuing on from where objects are projected to the hemiretinas of each eye, the information then travels to the optic nerve. To reach the optic nerve, axons of the ganglion cells must travel to the eye's posterior pole and become myelinated to exit the eye through the posterior aspect of the optic nerve. The optic nerve of each eye intersects at a point known as the optic chiasm, where fibers of each nasal hemiretina cross to the contralateral side.1
However, each retina's temporal side's fibers remain on the ipsilateral side. Moving further along the pathway, the contralateral fibers of the nasal hemiretina and ipsilateral fibers of the temporal hemiretina for each eye converge to form the optic tracts. This means that the left optic tract possesses fibers that display visual information from the right half of each eye’s visual field. Conversely, the right optic tract contains fibers that transmit visual information from the left half of each eye’s visual field. The optic tracts then project to their corresponding lateral geniculate nucleus (LGN) of the brain's thalamus.1
The LGN contains six layers; the first two layers are called magnocellular layers due to the large cells, whereas the next four are called parvocellular layers and contain smaller cells. The magnocellular layers involve location and movement, while parvocellular layers process form, color, and detail. Axons of the neurons in both the magnocellular and parvocellular systems of the LGN then project through the geniculocalcarine tract (optic radiations) to the primary visual cortex of the occipital lobe.1
The fibers in the optic radiation that serve the inferior quadrant of the opposite visual hemifield synapse on the superior aspect of the calcarine fissure of the visual cortex. Axons that serve the superior quadrant of the contralateral visual hemifield loop caudally (“Meyer’s loop”) and then synapse in the inferior aspect of the calcarine fissure of the cortex.1
Visual pathway lesions and defects
Visual pathway defects can occur due to various causes, such as compression of the optic nerve via a tumor, aneurysm, ischemic optic neuropathy, and many more.1 When a patient is affected by a pathway lesion, they may lose vision in a certain visual field area, which can be detected during an eye exam or visual field test. A scotoma is an ophthalmic term that describes a blind area in a patient's visual field, while anopia describes a complete loss of vision.1
Various lesions can occur along the visual pathway, each of which may result in a different visual field defect.
Scenarios of damage for visual field defect
Optic nerve
Starting with a lesion at the optic nerve, there will be a total loss of vision in that eye; this means that a lesion at the right optic nerve can cause total blindness in the right eye.1
Pituitary adenoma
Large pituitary adenomas are frequently the cause of non-homonymous bitemporal hemianopia.1 This is because the pituitary adenoma may compress the optic chiasm, disrupting the axons from the nasal hemiretina of both eyes. Thus, there is a loss of vision in the left visual field of the left eye and the right visual field of the right eye. Sometimes, the tumor may be surgically removed or irradiated to preserve vision and even reverse symptoms.
Optic tract
Damage to an optic tract typically causes contralateral homonymous hemianopia.1 Using the right optic tract as an example, it receives signals from the temporal hemiretina of the right eye and nasal hemiretina of the left eye. Both hemiretinas receive projections from the left visual field of each eye, thus causing loss of vision in the same half of each eye.2
Temporal lobe
Damage to the temporal lobe may affect Meyer’s loop; this may be caused by vascular occlusion in the middle cerebral artery, which supplies the inferior temporal lobe. Axons of neurons in the LGN project through the optic radiations to the ipsilateral primary visual cortex. Thus, if damage occurs in the right temporal lobe (Meyer’s loop), vision is lost in the superior left quadrant of each eye’s visual field, otherwise known as superior left homonymous quadrantanopia, or “pie-in-the-sky” visual field defect.1
Parietal lobe
Damage to the parietal lobe may also be caused by vascular occlusion of the middle cerebral artery. In the optic radiations, axons transmitting information about the inferior visual hemifields travel laterally to the ventricle in the inferior parietal lobe. Thus, vision loss will occur in the inferior left quadrant of each eye’s visual field if damage occurs to the right parietal lobe. This is also known as inferior left homonymous quadrantanopia or a “pie-on-the-floor” visual field defect.1
Geniculocalcarine tract
If there is damage to the full geniculocalcarine tract (optic radiation), vision loss is comparable to damage to the optic tract.1 If the optic radiation is damaged entirely on the right side, patients will suffer from contralateral homonymous hemianopia, in which the left half of the visual field for each eye is lost.
Calcarine fissure
Inferior: Damage to the inferior aspect of the calcarine fissure will produce a visual deficit similar to when Meyer’s loop is damaged; however, in this case, there is usually macular sparing, meaning that the center of the visual field may remain intact for each eye.1 Because the fibers of Meyer’s loop on the right side project to the inferior bank of the right calcarine fissure, the damage will typically lead to a superior left quadrantanopia.
Superior: Damage to the superior aspect of the calcarine fissure results in a visual impairment similar to when the parietal lobe is damaged, except that macular sparing may occur here.1 For example, the superior bank of the right calcarine fissure receives fibers from the LGN that is associated with input from the inferior quadrant of the contralateral visual hemifield; thus, an injury will result in an inferior left homonymous quadrantanopia, with conservation of central vision if macular fibers are indeed spared.
Both: Lastly, damage to both the superior and inferior aspects of the calcarine fissure will result in a visual impairment similar to damage to the entire optic tract, except for macular sparing.1 The defect is known as contralateral homonymous hemianopia.
Knowing these patterns of visual deficits can help to diagnose and manage patients. By performing a visual field exam, we can analyze the results and potentially find an underlying neurologic cause of vision loss. While the visual pathway is complex, breaking it down into individual steps can help isolate causes of vision loss and further implement treatment options for patients.
Don't forget to download our Visual Pathway Lesions and Visual Field Defects Cheat Sheet!
References
- Siegel A, Sapru HN. Essential Neuroscience. Philadelphia, PA: Wolters Kluwer; 2019.
- Grujicic MD R. Optic Tract. Kenhub. https://www.kenhub.com/en/library/anatomy/the-optic-tract. Published June 28, 2022. Accessed July 27, 2022.