Valsalva retinopathy is a rare condition that is specifically characterized by pre-retinal hemorrhages caused by a sudden increase in intrathoracic pressure and at times, a problematic vascular system.1 Most of the time, there is no need for clinical intervention because the particular form of ocular retinopathy usually presents in healthy individuals and spontaneously resolves on its own. Here is an overview of how to recognize and manage this unique condition.
What is Valsalva retinopathy?
Valsalva retinopathy commonly occurs secondary to the Valsalva maneuver, which is medically known as a forceful exhalation against a closed airway that causes a sudden increase in pressure in the chest and abdomen hindering venous return of blood to the heart.1 This hindrance of the venous system causes a rise of blood pressure that transmits to the eye and leads to a sudden increase of intraocular venous pressure that ruptures the small, superficial retinal capillaries forming pre-retinal hemorrhages under the internal limiting membrane or posterior hyaloid face.1
Valsalva maneuvers can occur through a number of everyday activities, including:
- Sneezing
- Vigorous coughing
- Vomiting
- Trying to lift heavy objects,
- Blowing musical instruments,
- Excessive straining through constipation
- Any strenuous physical exertions that may involve holding one’s breath
Valsalva retinopathy frequently presents in healthy eyes with no predilection for gender, ethnicity, or region.1 Although, individuals that are more at risk includes patients that already have presented with ocular vascular disease such as diabetic and hypertensive retinopathy, retinal vessel changes similar to retinal arterial tortuosity, retinal telangiectasias, or retinal macroaneurysms. Those taking anticoagulant medications are also more susceptible to Valsalva retinopathy.
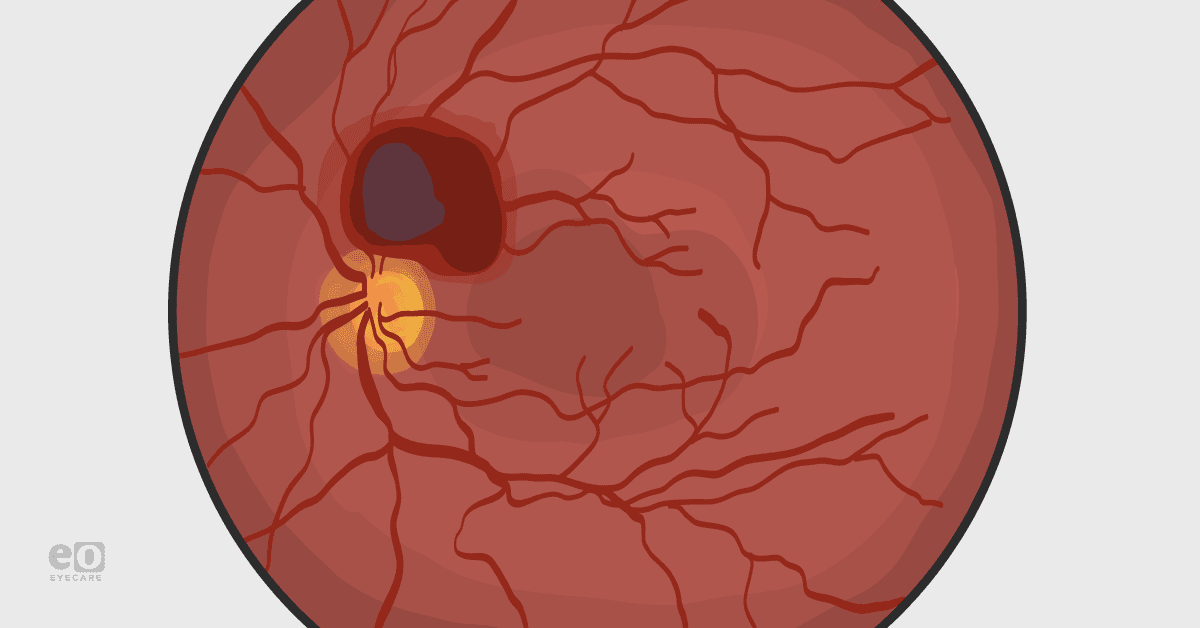
The clinical presentation of Valsalva retinopathy can be quite alarming depending on the severity and location of the preretinal hemorrhage. Keep in mind that the severity of the retinopathy is not necessarily correlated with the severity of the Valsalva maneuver. Typically, the presentation is unilateral, and the red hemorrhages appear large, well-circumscribed, and round and may extend several disc diameters over the macular area. If the hemorrhages involve the foveal region, visual acuities will likely be compromised. It is possible for the blood to break through the internal limiting membrane or posterior hyaloid face into the vitreous, thus becoming a diffuse vitreous hemorrhage. Other ocular signs can include subconjunctival hemorrhages and petechial hemorrhages of the eyelids.2
Patients can report a variety of complaints that include a sudden onset of painless unilateral vision loss, seeing a black spot or scotoma that is obstructing their vision. They may also complain of floaters that have a reddish hue, or even describe experiencing a sudden occurrence of blurred vision. Gathering and assessing information about the patient’s prior history is critical because these specific descriptions of sudden vision changes that are associated with Valsalva retinopathy are usually preceded by a history of Valsalva maneuvers.
How do you treat and manage Valsalva retinopathy?
Appropriately managing Valsalva retinopathy must begin with an accurate diagnosis. Even in atypical cases where the patient does not mention a history of Valsalva maneuver, it is still crucial to rule out the various conditions which can mimic Valsalva retinopathy. This includes acute posterior vitreous detachments where it is also necessary to rule out peripheral retinal tears, and the proliferative vascular retinopathies caused by diabetes, hypertension, retinal vein occlusion, sickle cell anemia and other diseases.
Along with providing a comprehensive ocular examination to initially monitor the patient, additional tests that are strongly recommended include optical coherence tomography to help pinpoint the location of the retinal bleeding, fundus fluorescein angiography to look for neovascularization, and ordering blood work to help rule out predisposing conditions such as diabetes, hypertension, sickle cell anemia, and blood clotting disorders amongst other diseases.2
Once the diagnosis of Valsalva retinopathy is established, observation involving monthly follow ups is the standard treatment. The typical recovery time is six weeks to six months, where larger hemorrhages can take a longer time to be reabsorbed. It is important to educate patients on avoiding strenuous activities and anticoagulant medications that could potentially worsen the retinal bleeding and/or produce additional pre-retinal hemorrhages. Additional recovery tips can include advising the patient to sleep in a seated or elevated position to stimulate blood settling, which can potentially improve visual acuities in cases that involve the macula.2
Earlier clinical intervention should be considered in cases with extensive bleeding that involve obscurity of the foveal region and significantly reduced visual acuities. This is because there is a concern of prolonged retinal exposure to hemoglobin and iron that can induce cellular toxicity, leading to irreversible visual impairment. In these particular cases, immediate surgical intervention through Nd:YAG laser is used to make an opening in the internal limiting membrane or posterior hyaloid face, blood can then escape into the vitreous cavity and settle inferiorly. This procedure clears the visual axis and helps improves overall visual acuities. Pars plana vitrectomy can be considered if there is long-standing and extensive pre-macular hemorrhaging, or a dense vitreous hemorrhage that causes difficult views during retinal evaluations.3
Lastly, it is important to note that patients presenting with the symptoms and signs highly suggestive of Valsalva retinopathy require a multispecialty evaluation to help confirm the exact cause of the retinal bleeding.
Valsalva retinopathy should not only be treated and managed by eyecare providers, but also should involve the patient’s primary care doctors to ensure compliance with maintaining healthy body weight, exercising regularly, and avoiding activities that lead to straining. A dietician can guide the patient towards a healthier diet in order to avoid issues like constipation. Pharmacists can verify appropriate dosages on certain medications and report any issues with pharmacological therapy being prescribed.
In order to ensure optimal patient outcomes, a collaborative, interprofessional healthcare team should be involved in the proper approach to care for and manage Valsalva retinopathy patients.
References
- Duane TD. Valsalva hemorrhagic retinopathy. Trans Am Ophthalmol Soc. 1972;70:298-313.
- Khan MT, Saeed MU, Shehzad MS, Qazi ZA. Nd:YAG laser treatment for Valsalva premacular hemorrhages: 6 month follow up : alternative management options for preretinal premacular hemorrhages in Valsalva retinopathy. Int Ophthalmol. 2008 Oct;28(5):325-7.
- Bourne RA, Talks SJ, Richards AB. Treatment of preretinal Valsalva haemorrhages with neodymium:YAG laser. Eye (Lond). 1999 Dec;13 ( Pt 6):791-3.