Note: Dr. Arthur Epstein contributed to this piece over several months last year, which is an honor to all of us at Lumenis. Throughout his career, Art’s contributions and curiosity resulted in fresh perspectives, unique insight, and a perpetuation of knowledge and visionary patient care that will be greatly missed by all of us in the dry eye community. He will never be forgotten.
Dry eye disease (DED) affects nearly 49 million Americans,1,2 making it a common condition that can cause burning, irritation, “tired” eyes, and fluctuating vision.3 The TFOS DEWS II Definition and Classification Subcommittee Report defines DED as a multifactorial disease characterized by the loss of homeostasis of the tear film due to tear film instability, hyperosmolarity, ocular surface inflammation, and neurosensory abnormalities.4 The most common cause of DED is meibomian gland dysfunction (MGD), also sometimes simplistically referred to as evaporative dry eye, which causes a disruption of the lipid layer of the tear film.3-6 Another, though less common cause is aqueous deficiency, which is usually associated with Sjögren’s syndrome and other autoimmune conditions, which leads to a reduction in the aqueous component of the tear film.4 Other conditions such as bacterial and Demodex blepharitis, ocular rosacea, post-refractive surgery state, lagophthalmos, and many others can also contribute to DED given its multifactorial nature.6 The commonality between the different causes of DED is a disruption of homeostasis of the tear film and ocular surface. If this disruption persists, it can ultimately result in inflammation, which exacerbates the underlying causes of DED and triggers further inflammation resulting in a vicious cycle and a gradually worsening condition. More severe variants of DED can greatly disrupt patients’ lives and should not be underestimated.
Because DED is multifactorial, it requires a multifaceted treatment approach to address all the constituent elements of the condition. This often means the use of multiple foundational therapies such as artificial tears, warm compresses, lid hygiene, and omega-3 supplementation to address the various causes of DED. However, intense pulsed light (IPL) offers a unique therapeutic option for DED as it functions through several different mechanisms of action that target the varying causes of DED at once in a single treatment modality. Specifically, Lumenis’ OptiLight is a light-based treatment that combines IPL and Optimal Pulse Technology (OPT) to deliver a controlled amount of light energy around the eyes to potentially break the cycle of tear film instability and dysfunction and the resultant loss of homeostasis and associated inflammation. When applied appropriately to selected patients, restoration of function may be achieved. This guide will address some of the most common causes of DED, the physics behind IPL, how IPL may address the causes of DED, ocular conditions that might benefit from the use of IPL, patient selection and education, and a step-by-step approach to performing the procedure, as well as how to implement OptiLight IPL into your practice.
What are common causes of dry eye disease?
Meibomian gland dysfunction
As previously mentioned, DED is a multifactorial disease with numerous potential causes and contributory conditions.4 However, meibomian gland dysfunction (MGD) is the leading cause or contributor to dry eye disease, with nearly 86% of cases of DED involving MGD.7 The meibomian glands are modified sebaceous glands that are found in the tarsal plate of the upper and lower eyelid, with approximately 20-30 glands in the lower eyelid and 30-50 in the upper eyelid7,8 The glands contain grape-like clusters of individual acini filled with meibocytes and exhibit holocrine secretion of meibum, which is composed of both lipids and proteins.7,9 The acini are connected to a central duct which releases the meibum onto the surface of the lid margin upon completion of each blink.7,8
The meibum is then spread over the ocular surface as the lids blink across the eye. Because the glands utilize holocrine secretion, the meibocytes contained in the acini must constantly be replenished.7,8 However, if the glands become obstructed or meibocyte turnover is impeded due to physical blockage, changes in meibum composition, or inflammation, this delicate system is disrupted and MGD can occur. A key function of the lipid layer is to prevent evaporation of the tear film, so either a reduction in meibum production or quality can result in faster than normal breakup of the tear film, which is clinically observed as a reduced tear breakup time (TBUT), which is why DED caused by MGD is often referred to as evaporative dry eye.4,6 Disruption of the lipid layer of the tear film causes instability of the entire structure and results in a loss of homeostasis which can lead to inflammation that further exacerbates the condition. While the exact underlying etiology of MGD is not fully understood; nevertheless, it is also believed to be multifactorial with behavioral, environmental, hormonal, dietary, genetic, and age-related factors, as well as the use of certain medications, all potentially playing a role in the development of the condition.10-12
In incidences of chronic dysfunction, the meibum's composition changes to include fewer unsaturated fats, which can lead to a significantly higher melting point that is warmer than body temperature.13-16 Therefore, this abnormal meibum does not properly integrate into the tear film's lipid layer and can also cause clogging of the glands. This results in dysfunctional meibomian glands and an unstable tear film leading to a loss of tear film and ocular surface homeostasis, which manifests as the burning, grittiness, foreign body sensation, redness, periocular swelling and irritation, and fluctuating vision characteristic of dry eye.11,17 The hallmark signs of MGD are clogged or inspissated glands, which may be enlarged and inflamed, and a reduction or absence of meibum expression with thickened, semi-solid toothpaste-like secretions rather than oil-like droplets.18,19
Distended, inspissated, and inflamed meibomian glands are characteristic of MGD. Photo courtesy of authors.
Another potential complication of MGD is the development of chalazia. The disruption of normal gland function in MGD can result in a chronically obstructed and inflamed gland which can cause the development of a lipogranuloma in the form of a chalazion.20 A chalazion presents as a “bump” on the lid, and while it may self-resolve, in some cases it can become chronic,21,22 which can be both a cosmetic and functional concern for the patient
MGD can also be caused or exacerbated by other ocular surface diseases such as ocular rosacea, bacterial and Demodex blepharitis, and abnormal eyelid function, which will be described in more detail in the corresponding sections below.
Meibography of upper and lower eyelids displaying significant meibomian gland loss. Image courtesy of authors.
Aqueous deficiency
Although not as common as MGD, aqueous deficiency is another cause of DED that results in a reduced production of the aqueous component of the tear film. Unlike other causes of DED that are not necessarily inflammatory in nature, cases of aqueous deficiency are often intrinsically inflammatory as they are typically associated with autoimmune conditions such as Sjögren’s syndrome.6 For instance, in Sjögren’s syndrome there is lymphocytic infiltration of the lacrimal gland which results in inflammation and disruption of aqueous production.4 This can result in an unstable tear film, reduced tear volume, and ocular surface inflammation.6 It is worth noting that a diminished aqueous tear volume can also exacerbate evaporation, suggesting that evaporative dry eye and aqueous deficient dry eye typically exist as part of a continuum rather than as two completely distinct and independent entities.23
A reduced tear meniscus height can be a sign of aqueous deficiency, which is common in conditions such as Sjögren’s Syndrome. Image courtesy of authors.
Ocular rosacea
Ocular rosacea is characterized by the presence of fine, spider-like blood vessels that develop on the lid margin and conjunctiva known as telangiectasia.24 These vessels are proinflammatory and can cause significant cosmetic redness and ocular irritation16,17,24-26 and are prone to flushing when exposed to certain environmental triggers, such as extreme heat or cold, spicy foods, alcohol, or cosmetics, all of which can worsen inflammation.25,27-29 Additionally, ocular rosacea, like facial rosacea, affects the sebaceous glands, including the meibomian glands, which are modified sebaceous glands, causing inflammation which results in MGD.16,17 The chronic inflammation observed in ocular rosacea leads to further development of telangiectatic vessels which are adjacent to the meibomian glands and release proinflammatory factors that inflame the glands and disrupt their function.16,17,30 This disruption of the meibomian glands can also alter the microbiome of the lids and lashes, as normal, healthy meibum impedes bacterial growth.31 Therefore, alteration of meibum quality can lead to an overgrowth of bacteria that can further exacerbate MGD and inflammation associated with ocular rosacea. Epithelial cell turnover is also significantly increased in rosacea, including on the lid margin which can lead to a buildup of dandruff-like debris which can in turn cause dead epithelial cells to block the meibomian gland orifices resulting in obstruction and impeded meibum secretion.16,32 In addition to irritation, ocular rosacea causes significant redness of the eyes and lids due to the presence of abnormal, dilated vessels creating a major cosmetic concern for many patients. There is also a noteworthy association between ocular rosacea and Demodex, with Demodex even being suggested as the causative agent of rosacea.25,27-29,33,34 While the cause versus effect relationship between the two conditions is unclear, it is important to note that patients displaying signs of ocular rosacea will often also have Demodex present and vice versa.35-37
Telangiectatic vessel development on the eyelids and lid margins are hallmark signs of ocular rosacea. Photo courtesy of authors.
Bacterial blepharitis
Chronic bacterial blepharitis is a common comorbidity of DED. Typically, blepharitis is caused by an overgrowth of the normal bacterial microflora found on the eyelids and lashes, usually Staphylococcal species such as Staphylococcus aureus.40 Staphylococcus epidermidis, and coagulase-negative staphylococci. These bacteria secrete exotoxins and waste that trigger inflammation of the eyelids and ocular surface.41,42 The presence of the bacteria stimulates an inflammatory response aimed at eliminating the pathogen, however, while this starts as an acute response, it can become chronic, which damages the lid margin and meibomian glands resulting in MGD.41 These bacteria produce lipases that break down the lipid component of the tear film and alter the ratio of saturated to unsaturated fats in meibum, which increases the melting point and results in increased viscosity that further impedes lipid secretion and contributes to tear film instability.18,32 Clinically, this breakdown of the lipid layer can manifest as the presence of saponification, which causes the tears to have a foamy or frothy appearance.43 Additionally, a byproduct of the breakdown of the lipid layer and meibum is oleic acid, which at high levels can cause keratinization of the lid margin that can physically obstruct the meibomian gland orifices.30 Additionally, healthy meibum has been shown to have antimicrobial properties; however, the meibum produced in MGD may no longer exhibit the same antibacterial effects, which then allows for further bacterial growth on the lid margin leading to even further degradation of meibum quality resulting in a vicious cycle.31 The signs of chronic bacterial blepharitis include burning, persistent erythema, grittiness, and recurrent lash debris and crusting.41 If left untreated, this chronic inflammation can cause scarring on the lid margin in the form of thickening or notching which could disrupt proper lid position and function.42 Consequently as the lipid layer continues to fail, evaporation of the tear film accelerates, osmolarity increases, and irritation and damage to the corneal surface ensues.11,17
Foamy or frothy tears, known as saponification, is a sign of bacterial overpopulation and can signal a breakdown of the tear film. Photo courtesy of author
Lid margin notching or scarring can result from chronic inflammation caused by blepharitis. Photo courtesy of authors.
Demodex blepharitis
Demodex are ectoparasitic mites that are part of our skin’s natural microflora.43,44 However, when they overpopulate on the lids and lashes, it can result in Demodex blepharitis.44-50 The two mite species found on humans are Demodex folliculorum and Demodex brevis, which inhabit the eyelash follicles and meibomian glands, respectively.44,50-54 These mites stimulate inflammation of the lids and ocular surface by physically feeding on epithelial cells and meibum, releasing digestive enzymes onto the lid margin and ocular surface, and physically obstructing the meibomian glands and burrowing into them resulting in gland hyperplasia and MGD.44,46,47,48,50,55,56 The pathognomonic sign of Demodex blepharitis is a cylindrical, sleeve-like buildup of waxy debris at the bases of the lashes known as collarettes.45,48,49,56-58 These collarettes are proinflammatory, as they contain a mix of Demodex waste, eggs, and digestive material.45,48,49,56,57 The mites also harbor streptococcal, staphylococcal, and bacillus bacterial species that are also capable of eliciting an inflammatory response as previously mentioned.36,59-61 Demodex are more common in patients with ocular rosacea, so it is common for patients to be affected by both conditions.35-37
Collarettes are cylindrical, sleeve-like buildups of debris consisting of waste, mite eggs, and digestive material at the base of the eyelashes and are pathognomonic for Demodex. Photo courtesy of authors.
Mechanical eyelid issues
Proper blinking mechanics are crucial to ocular surface health and function. Ideally, blinks should be complete, with the upper and lower lids coming into contact with each blink. The reason for this stems from the proposed mechanisms of meibum secretion. It is thought that meibum secretion has both passive and active elements, with the oil being continuously driven into the ducts and out of the glands by the constant production of meibocytes in the acini that are the basis for the holocrine secretions8,62 and with more active expression due to the contraction and relaxation of the orbicularis oculi muscle and muscle of Riolan.8,63 It has been proposed that with each blink the contraction of the orbicularis oculi pressurizes the glands and when the upper and lower lids touch, Riolan’s muscle, which encircles and seals the orifices of each gland, relaxes and opens allowing the meibum to be secreted onto the surface of the lid margin.8,63,64 After its secretion, the oil is then spread across the ocular surface by the blinking motion of the lids.65,66 Therefore, if these mechanics are abnormal either due to incomplete lid closure secondary to iagophthalmos or poor lid apposition to the globe due to ectropion or loss of lid rigidity or elasticity, then meibum secretion and/or its spread across the ocular surface can be disrupted which can contribute to MGD and DED.67
The eyelids naturally lose rigidity and elasticity with age, which can lead to incomplete lid closure, poor apposition to the globe, and abnormal blinking mechanics, all of which can have a detrimental effect on ocular surface stability and function. Photo courtesy of authors.
What is intense pulsed light (IPL) and how does it work?
Intense pulsed light (IPL) is a non-laser high-intensity light source that uses a xenon flash lamp to produce a light output of wavelengths in the range of 400 to 1200 nm.17,68 When used for the treatment of DED and MGD, IPL treatment delivers controlled pulses of intense light of only a few milliseconds duration, with pulses typically applied to the upper face.15 The application of this light has several different effects which can address and improve the underlying causes of MGD and DED, which will be discussed further in the following sections.
History of IPL
IPL has long been used in dermatology to treat a number of skin conditions and for the removal of lesions such as hemangiomas, telangiectasia, and rosacea.10,16,26 Additionally, it has been used for cosmetic purposes such as in “skin tightening” photofacial treatments.69 In the ophthalmic community, IPL has been in use for nearly two decades, with the use of IPL for the treatment of dry eye first discovered in 2002.70 Serendipitously, while treating dermatological conditions, such as rosacea, Rolando Toyos, MD, found that patients who also had concomitant dry eye noted improvements in their signs and symptoms after IPL treatment.17,71 This observation eventually resulted in a research grant that accelerated the exploration of IPL as a treatment for MGD and dry eye which led to the development of the techniques and treatment patterns used today.72,73
Biophysics
At a fundamental level, IPL works by delivering energy in the form of light which directly and/or indirectly interacts with different target tissues. Pigmented structures within the skin such as melanin and hemoglobin are described as chromophores and are frequent targets, as the light emitted in IPL is absorbed by pigment.10,16,26,68 As light is a form of energy, when high intensity light is absorbed by pigment, energy is also absorbed. This energy absorption results in the therapeutic effects of IPL including improvement of MGD,74-80 eradication of Demodex and bacteria,10,16,81,82 and destruction of telangiectatic vessels10,26,77,83 along with a decrease in the level of inflammatory factors present in the tear film and on the ocular surface.16,84-92 Another effect of this process is referred to as photobiomodulation, which is the delivery of light energy to a target tissue which results in the stimulation of intracellular biological processes that can even occur at the protein and gene level.10,16,93,94 IPL is particularly efficacious when used in the periocular region, as the skin in this area is some of the thinnest on the body and the light produced can easily penetrate the tissue to reach underlying targets.10
The physics behind IPL can be quite complex, especially when treating DED. However, understanding the physics of IPL is essential to proper use and establishing appropriate settings for treatment. Because light serves as an “envelope” for energy, energy control is a primary consideration, and is one of several key factors that can be recognized and controlled.
One of the most important factors in assessing an IPL patient is skin pigmentation. Skin tone has a close, if not direct, correlation to light, and, therefore, energy absorption. Darker skin tones absorb greater amounts of light energy requiring a reduction of fluence (applied energy to a treated area) to achieve the desired result. The Fitzpatrick scale, often referred to as the “Fitz scale”, ranges from skin pigmentation Type I to Type VI with Types I to IV generally being treatable with appropriate energy setting compensation, and Type V being treated using the lowest fluence (energy) settings and only after a careful test treatment of a small inconspicuous area is performed prior to performing a full treatment. Type VI is generally considered untreatable due to the high levels of pigmentation and energy absorption even at low fluence settings. This will be discussed in greater detail in the sections below.
Treatment elements that can be controlled by the OptiLight instrument settings include fluence, which is defined as the energy applied over a given area, the Fitzpatrick skin type as mentioned above (with an approved indication for Types I to IV), and the light filter (which can be changed using the upgraded configuration) which determines the wavelength of light produced and will be described in more detail below. Fluence is typically measured in joules/centimeter.4 The higher the fluence, the greater the energy applied to a given area. Commercially available IPL devices vary from relatively simple single pulse units to sophisticated modern devices that deliver precisely controlled multi-pulse, semi-resonant square waves. Designed to distribute high levels of energy in smaller, more consistent packets, multi-pulse systems such as Lumenis’ OPT system provide state of the art control paired with the potential to improve patient comfort while maintaining high therapeutic energy levels.
Additionally, advances in these modern instruments allow for control of both waveform and wave train – the shape, energy, and number of pulses applied. Tissue penetration and interaction are accomplished through the use of cutoff or high-pass filters, as these filters determine the wavelength of light emitted, and, in turn, the wavelength determines how deeply the light penetrates the tissue and the targets it reaches and affects. The cutoff filter most commonly used in IPL for the treatment of DED is a 590 nm filter, which means all wavelengths below are “cut off” while the wavelengths above are transmitted. Therefore, a 590 nm filter produces light that corresponds to yellow, orange, and red visible light in addition to near infrared light.95,96
The standard OptiLight 590 nm filter emits wavelengths that span from 590 to 1200 nm corresponding to yellow, orange, and red visible light, as well as near-infrared light, on the electromagnetic spectrum.
When IPL was initially discovered and developed as a well-tolerated treatment for a variety of dermatological and related aesthetic conditions, its mechanism of action was primarily thought to be through direct interaction with tissue. This included heating, and in some cases, disruption or destruction of chromophores specifically targeted within the different layers of the skin. Examples of such uses include treating facial rosacea, removing pigmented lesions of the skin, and hair removal. Other direct beneficial dermatological effects were subsequently recognized, such as increased and improved skin collagen and elastin.16,97-10
To understand how IPL can improve meibomian gland function and dry eye symptoms, a bit of reverse system engineering and understanding of relevant physics and anatomy is required. The inverse square law is an essential rule of physics and states energy will diminish as the square of its distance from the source. What that means practically for IPL treatment is the energy directly applied using a standard tragus to tragus treatment pattern will have diminished exponentially by the time it reaches the eyelids and the meibomian glands. However, a fundamental property of electromagnetic radiation (EMR) is that its wavelength specifies the actual length of the generated or transmitted wave as well as its energy. Critical to the understanding of wave propagation, and, clinically, tissue penetration, is the fact that wavelength and frequency, as well as energy, are inversely proportional. Radio waves, which have the longest wavelength of the electromagnetic spectrum, of which visible light is also a part, are an excellent example of this relationship. For instance, a radio transmitter operating at a frequency of 7 MHz will create a signal with a wavelength of 40 meters. This is a relatively long wavelength with a low frequency and energy, but this wave can travel great distances. Therefore, the longer the wavelength, the lower the frequency and energy but the deeper the tissue penetration, and, conversely, the shorter the wavelength, the higher the frequency and energy but the more superficial the wave’s penetration. Accordingly, cutoff filters can be used to deliver energy to specific target tissues by producing light of the necessary wavelength required to reach the target. For instance, different cutoff filters can be used to produce wavelengths of light that specifically target certain chromophores, such as melanin or hemoglobin, based on their depth. The typical cutoff filter used for the treatment of MGD and DED produces wavelengths ranging from 590 to 1200 nm, which reach and concentrate light energy from approximately the dermal-epidermal junction to the hypodermis and beyond.
The wavelength of light determines how deeply it can penetrate skin and the target tissues it reaches. The high intensity yellow, orange, red, and near-infrared light produced by the standard 590 nm OptiLight filter penetrates from approximately the dermal-epidermal junction to beyond the hypodermis.
Additionally, the long-recognized law of conservation of energy states that the total energy of an isolated system remains constant; it is neither created nor destroyed. However, it may be transformed or transferred. Therefore, once the wavelengths of light produced by IPL reach the meibomian glands, the energy carried by the light is transferred to the glands. It is likely this transfer of energy that stimulates the meibomian glands and produces the therapeutic effects of IPL observed in MGD.
When discussing energy absorption in relation to the meibomian glands and IPL, it is worth noting the controversial role that thermal energy, or heat, plays in its effects on MGD. Although it was initially thought that the standard tragus to tragus application technique generated sufficient heat to liquify congealed meibum within the glands (which is likely why treatments were followed by manual gland expression when the use of IPL for DED was first being explored), experience, physics, and actual measurement would suggest otherwise.16,102,103 While there may be some minor disruption of meibum carbon bonds upon IPL treatment, any liquefaction is transient at best, which is discussed further in a later section.
What is OptiLight?
Lumenis’ light treatment is a drug-free, drop-free solution that is the first and only IPL device FDA approved for the -management of MGD and dry eye. The device uses Lumenis' patented and innovative Optimal Pulse Technology (OPT) easily allowing for a consistent, precise, and controlled light-based treatment of the signs of MGD and DED.77
Unique Features of OptiLight:
- Patented Optimal Pulse Technology that transforms light-based therapy. Lumenis’ OPT allows for targeted, precise, and controlled treatment with homogeneous pulses that provide controlled, optimal energy with a no-spike consistency.
- An ergonomic IPL handpiece with a patented SapphireCool™ technology which actively cools the lightguide while performing the procedure, allowing for comfortable treatment even with higher levels of energy.
- The patented OPT handpiece with Opti-Tip disposable tip is ideal for hard-to-reach places which allows for precise, customizable treatment of every curve and outline of a patient’s unique facial contours while ensuring treatment is safe, hygienic, and effective.
- Lumenis’ clinically validated treatment protocols, based on information gathered from hundreds of patients, allow for the use of preset, fixed settings that can easily be used to provide well-tolerated and effective treatments.
- While the default version of OptiLight contains the standard 590 nm filter used for the management of MGD and dry eye, it is a modular system that offers additional ExpertFilters tailored for different skin conditions for optimized results, which are all suitable for one handpiece.
OptiLight IPL uses several different mechanisms of action to address the various causes of dry eye disease in a single treatment modality.
How does OptiLight manage dry eye?
IPL has been shown to improve the signs and symptoms of dry eye.17,74-76,80,102,104 For patients with dry eye disease, IPL treatments utilize pulses of light to treat the condition through several different mechanisms including: photobiomodulation,10,16 reducing inflammatory factors present in the tear film and on the ocular surface,16,84-92 improving meibomian gland structure, function, and secretions,74-80 destroying proinflammatory telangiectatic vessels, especially those associated with ocular rosacea,10,26,83,87 decreasing Demodex and bacterial populations present on the lids and lashes,10,16,81,82 and potentially improving blinking mechanics.16,97-100 These findings have been backed by many peer-reviewed prospective studies that have shown that the Lumenis IPL devices improved tear breakup time, meibum quality, and meibomian gland expressibility,74,105 and reduced ocular surface inflammation as well.84-87 This has led to Lumenis’ light therapy being FDA-approved for use in the management of DED due to MGD which makes it the first, and currently only, device of its kind to receive this approval.79
Benefits of IPL:
- Improves meibomian gland structure, function, quality of meibum, and tear breakup time (TBUT)74-80
- Reduces inflammatory factors found in the tear film and on the ocular surface16,84-92
- Destroys telangiectatic blood vessels (ocular rosacea), which are a major source of inflammation to the eyelids10,26,83,87
- Decreases Demodex and bacterial load on eyelids10,16,81,82
- Potentially improves blinking mechanics by increasing the tone of lid skin and improving lid margin notching and scarring through stimulation of collagen synthesis16,97-100,106
Dry eye disease is a multifactorial condition with many contributory factors. However, these individual factors can exacerbate one another leading to a vicious cycle that results in worsening tear film stability and ocular surface homeostasis.
The fundamental reason IPL could be a successful treatment option for dry eye is that it addresses the various root causes of the disease, including MGD and downstream inflammation through multiple mechanisms of action that collectively interrupt the vicious cycle that instigates and perpetuates dry eye and possibly helps restore tear film and ocular surface homeostasis. These proposed mechanisms are discussed in greater detail in the following sections.
IPL and photobiomodulation
While IPL addresses the various conditions that contribute to DED in a manner that is specific to each, it also broadly acts through photobiomodulation.107 Photobiomodulation refers to the delivery of energy to a target tissue in the form of light in the visible and infrared regions of the electromagnetic spectrum which stimulates intracellular biological processes through photochemical reactions including effects at the protein and gene levels.10,16,93,94 The ultimate target of photobiomodulation is thought to be cytochrome c oxidase (COX) contained in the mitochondria of cells treated with IPL.16,108,109 COX is an enzyme that is part of the electron transport chain responsible for producing adenosine triphosphate (ATP).16,186-110 COX is also a chromophore that contains pigments that absorb the light energy produced by IPL, which results in photoexcitation of the enzyme and increased energy production in the form of ATP.16,108-110 This increase in ATP enhances the function of intra- and extracellular exchange structures, such as pumps and transporters, that ultimately leads to an increase in free intracellular calcium.16,108,109,111 Another proposed separate or complementary mechanism for photobiomodulation suggests that the energy delivered by IPL causes physical vibrations of cellular calcium channels, changing their permeability and thus increasing the level of free intracellular calcium.94 Calcium is a key intracellular signaling molecule that can stimulate cell proliferation, migration, and differentiation, as well as cellular repair and healing.10,112-114
Photobiomodulation stimulates tissue repair and regeneration through action on several different cell types including fibroblasts, keratinocytes, T cells, and macrophages.10,97,115,116 Activation of fibroblasts stimulates cell proliferation and collagen synthesis,100 keratinocytes regulate epithelial wound healing,117 T cells control immune and inflammatory responses,118 while macrophages clear dead cells and proinflammatory debris.119 Additionally, the chemical cascade induced by photobiomodulation is also thought to have anti-inflammatory effects as well, including an increase in antioxidant levels and a decrease in stress-related genetic material associated with cell death.120 Photobiomodulation is simultaneously thought to increase local blood flow, which can aid in tissue healing and repair.10,16 However, this enhanced blood flow is not likely due to an increase in intracellular calcium, as an increase in calcium stimulates smooth muscle contraction which reduces arterial diameter and decreases blood flow.121 Rather, it is thought this increase in blood flow is stimulated by elevated nitric oxide, which is a potent vasodilator.122 Photobiomodulation may increase nitric oxide through stimulation of COX leading to increased activity of nitrite reductase, or through dissociation of nitric oxide from COX upon photoexcitation,123 thus stimulating vasodilation and increasing blood flow.
How could IPL improve inflammation?
As discussed in the previous sections, IPL improves inflammation by addressing its root causes whether it be MGD, ocular rosacea, or bacterial or Demodex blepharitis. Additionally, through photobiomodulation the presence of proinflammatory molecules is reduced and anti-inflammatory factors are stimulated.14 Inflammation reduction is a major benefit of IPL, as there are elevated levels of proinflammatory factors found in the tears and on the ocular surface of dry eye patients, with these proinflammatory factors being associated with pain, tear film instability, and ocular surface disruption, including goblet cell dysfunction and/or dropout.124-126 IPL addresses inflammation by disrupting the inflammatory cascade by altering the production of proinflammatory and anti-inflammatory molecules.16 Specifically, IPL has been shown to increase IL-10, which is an anti-inflammatory factor that blocks cytokine production by T cells, and decreases IL-6 which is proinflammatory.88,87,90 IPL also alters the levels of TGF-β,89,127 TNF-α,91 and MMPs.92,128 TGF- β can be both pro- and anti-inflammatory as it modulates T cell proliferation on the ocular surface.127 It has been noted that IPL decreases the presence of TGF- β at low fluences and increases its levels at high fluences.89 TNF-α, which is involved in acute inflammation, is also decreased by IPL.91 Additionally, this downregulation of TNF-α indirectly decreases the levels of MMP, which is an enzyme that breaks down extracellular matrix, as TNF-α upregulates MMP production.91, 129 MMP levels are directly reduced by IPL at the mRNA level as well.92
IPL additionally appears to alter the levels of reactive oxygen species (ROS), also known as free radicals, present in the tear film. ROS levels are elevated in the tear film of dry eye patients, which can create damaging oxidative stress.130 However, IPL seems to have a somewhat contradictory effect on ROS as it is shown to decrease ROS levels, while from a mechanistic standpoint the treatment should increase these levels.131,132 As IPL is thought to stimulate the electron transport chain in mitochondria via photobiomodulation, an increase in the production of free radicals as a byproduct of this process would be expected.131 Therefore, it has been proposed that the decrease in ROS levels after IPL treatment is due to a biphasic dose response referred to as an Arndt-Schultz curve.133,134 In this model, at low energy levels IPL would induce ROS formation, while at high energy levels it would promote antioxidative effects.16 It has been suggested that both these responses may be beneficial in dry eye as an increase in ROS can have antimicrobial effects which could reduce the bacterial burden on the lids and lashes, whereas a decrease in ROS would have an overall anti-inflammatory effect.16
How does IPL potentially improve meibomian gland dysfunction?
IPL has been shown to improve meibomian gland structure, function, and quality of meibum.74-80 OptiLight is proposed to improve MGD through several different mechanisms. Light energy from IPL is thought to liquefy the stagnant meibum in clogged glands which clears obstruction and improves the quality of secretions and the lipid layer of the tear film.74-77 This further improves the morphology of the meibomian glands, as the dilated and distended glands are returned to a normalized anatomical position.77 Initially, it was thought that the heat generated by the intense pulses of light would melt any clogged oil in the glands,10 but the heat generated dissipates so quickly it is likely not sustained for a long enough duration to facilitate full melting.16,102,103 However, IPL may liquefy the solidified meibum through a photochemical process rather than a thermal one, whereby it alters the bonds of the fatty acids present, as it has been shown that the normal hydrocarbon chain configuration and lipid-lipid interaction strength of meibum are altered in MGD.14,16,135
Lumenis light based therapy has been shown to improve meibomian gland structure, function, and meibum quality as shown by this example of lipid layer interferometry displaying significantly increased lipid layer thickness (LLT) after treatment with OptiLight (bottom) compared to before treatment (top). Image courtesy of authors.
Additionally, photobiomodulation may improve MGD directly and indirectly. As a reminder, the meibomian glands are holocrine glands, which means entire cells are secreted in the process of meibum production. This means meibocytes, which ultimately mature and disintegrate to form meibum, must constantly be replenished.7,8 Therefore, an increase in meibocyte proliferation due to the effects of photobiomodulation may directly propagate meibum production through enhanced production of the cellular source material of the secretion. Photobiomodulation may also indirectly improve MGD by improving blinking mechanics. By stimulating fibroblast activity, collagen synthesis is increased which can tighten the skin surrounding the eyes, including the eyelids.16,97-101 As skin naturally loses its rigidity and elasticity with age, this can lead to improper lid closure and poor lid apposition against the globe, which can interfere with meibum secretion and spreading of the lipid over the ocular surface. However, increased collagen production can help restore rigidity and elasticity to the lid skin which may aid in proper meibum secretion and its spread across the ocular surface. These mechanisms likely play a role in the improved structure and function of the meibomian glands, as well as the quality of meibum secretions.74-80 Ultimately, the clinical study by Dell et al illustrated this improvement in meibomian gland function and meibum quality after IPL treatment had a significant impact on tear breakup time, as a full series of treatment was shown to nearly double TBUT.74
Lumenis light based therapy has been shown to significantly increase tear break up time (TBUT) as is demonstrated by these noninvasive tear break up times (NITBUT) from before (top) and after (bottom) treatment. Image courtesy of authors.
How could IPL improve ocular rosacea?
IPL addresses ocular rosacea by targeting the proinflammatory telangiectatic blood vessels that are characteristic of the disease. When light passes through the appropriate filter and the desired wavelengths are produced, the incident light is selectively absorbed by the hemoglobin in the red blood cells of the telangiectatic vessels causing the blood to coagulate, and the vessel to involute and close.10,83 This destroys blood vessels that perpetuate inflammation and decreases the number of proinflammatory factors they secrete.26,83,102 Elimination of atypical blood vessels reduces a significant reservoir of inflammatory mediators, interrupts the vicious cycle of inflammation, and improves the symptoms of ocular rosacea and dry eye.26,75,83 The destruction of these vessels can also improve cosmetic appearance by reducing the facial and ocular erythema caused by telangiectasia.26 The regression of these abnormal vessels also improves meibomian gland health by eliminating a source of inflammation that disrupts gland function.16,26 Additionally, treatment with IPL can reduce the abnormally high turnover rate of epithelial cells, which can result in a reduction of buildup of dead epithelial cells on the lid margin and therefore reduce the likelihood of meibomian gland orifice obstruction by this debris.16,32
How does IPL potentiate improvement in blepharitis?
Overgrowth of normal microflora, such as staphylococcal bacterial species, is a common cause of blepharitis and contributing factor to DED. As previously discussed, these bacteria can also produce enzymes that break down the lipid layer of the tear film which can exacerbate MGD in addition to producing proinflammatory waste. IPL treatment has been shown to decrease the number of bacteria present on the lids and lashes,17 including the bacteria associated with Demodex mites.10,16 Therefore, treatment with IPL can reduce the inflammation caused by bacterial overgrowth and help restore healthy meibum by also reducing the bacterial lipases that disrupt the lipids of the tear film.10
How does IPL modulate or reduce Demodex populations?
IPL is demodicidal as the chromophores found in the mites’ exoskeleton absorb the energy generated by IPL causing rapid heating of the mites resulting in coagulative necrosis.81 This makes IPL an optimal treatment option for Demodex blepharitis as it reduces the mite population. This in turn scales down the inflammation caused by the mechanical damage inflicted when the mites feed on meibum and epithelial cells, production of proinflammatory lash collarettes, and the associated bacterial reservoir the mites harbor.26,36,44,46-48,50,55,56,59-61,82,83 Additionally, there is a strong association between Demodex and rosacea, and it has even been suggested that Demodex are the underlying causative organism of rosacea.25,27-29,33,34 Thus, there may be crossover synergistic benefit between the two conditions when IPL is used as treatment. Additionally, Demodex can exacerbate MGD, as Demodex brevis burrow into the meibomian glands which can physically obstruct the gland orifices and prevent oil from being secreted, so destroying the mites can remove a potential source of gland blockage.46,47,50 This gland obstruction by the mites has also been associated with chalazion formation,56,136 therefore IPL treatment can potentially reduce the likelihood of future chalazion formation in patients who are prone to the condition. Consequently, by treating this Demodex infestation, patients can experience an improvement in associated blepharitis and MGD which results in reduced chronic inflammation and likely requisite improvement in quality of the lipid layer.26,82,83
What is the link between IPL and mechanical eyelid issues?
IPL can potentially improve DED related to mechanical lid issues such as poor lid apposition to the globe and lid margin disruption. Through photobiomodulation, light energy in IPL is absorbed by cytochrome c within the mitochondria, which is part of the electron transport chain and stimulates ATP production as previously mentioned.16,108-110 This facilitates important cellular functions such as enhancing collagen and elastin synthesis in fibroblasts and motility in immunoregulatory cells.16,97-101 The ability of IPL to stimulate fibroblasts and enhance collagen synthesis can help improve the natural loss of skin rigidity and elasticity associated with aging. This is the reason IPL has long been used in aesthetics for photofacials aimed at reducing wrinkles and sun damage.69 However, this effect can have utility beyond the purely cosmetic, as IPL can help reduce poor apposition of the lids to the globe and incomplete blinks due to decreased elasticity of the skin of the eyelids, resulting in improved meibum secretion and decreased tear evaporation.26,77,83 Additionally, IPL can also improve the cosmetic appearance and function of the lid margin that has experienced notching and scarring due to chronic inflammation.106
Who is a good candidate for OptiLight treatment?
Prior to using OptiLight, a thorough dry eye exam including a dry eye questionnaire, evaluation of the ocular surface and lids, meibography, TBUT, assessment of tear meniscus height, and lipid layer analysis, if available, should be performed. Additionally, it is critical to talk to the patient to learn about their specific issues and concerns regarding their dry eye. Both this objective and subjective data is vital to identifying a good candidate for OptiLight and tracking their progress throughout their treatment. Since OptiLight addresses DED due to MGD through several mechanisms, there will likely be many potential candidates. With this said, proper patient selection is critical when measuring the success of the IPL treatment along with managing post-procedure expectations. Specifically, patients displaying MGD and comorbidities such as ocular rosacea, Demodex or bacterial blepharitis, or generalized ocular surface inflammation are prospective candidates. One or more of these elements is likely to occur in nearly every dry eye patient, so it is helpful to keep IPL in mind when determining the best course of treatment for your dry eye and ocular surface disease patients.
IPL treatments have been cited in the TFOS DEWS II recommended staged management plan for DED, where it is considered a second-stage management option after foundational treatments have been initiated.137 Due to its multiple mechanisms of action, it is a treatment of choice for patients requiring more advanced management. Therefore, to achieve optimal success with IPL, it is critical that patients are concurrently following a foundational dry eye treatment regimen as well.
While IPL is an incredibly powerful treatment option, patients will experience the greatest benefit if they are also using a dry eye treatment protocol that includes:
- Omega 3 fatty acid supplementation
- Recommend a high quality, re-esterified, triglyceride-based supplement with 3:1 EPA to DHA ratio and at least 2 grams of combined EPA and DHA
- Warm compresses
- May not be ideal for all patients, use with caution in patients with ocular rosacea
- Blink exercises
- Lid hygiene
- Hypochlorous acid
- Tea tree oil
- Artificial tears
- Primarily palliative
- Recommend preservative-free, lipid-based formulations or gels
- Immunomodulators (if necessary)
- Nocturnal Exposure
- Gels or Ointments
- Moisture goggles
- Other Treatments
- Tyrvaya
- Eysuvis
- iTear100
- NuLids
While these foundational treatments are helpful for many suffering from DED, many more still struggle with DED despite trying initial therapies. These patients are certainly candidates for IPL, as are many newly diagnosed DED patients who want to be proactive in their treatment. Additionally, longtime dry eye patients who are looking for a treatment option that does not require adding another daily therapy to their regimen are ideal candidates as well.
Another critical element to patient selection and safety is accurately determining a patient’s skin pigmentation level, which is typically done using the Fitzpatrick scale.17,138 Ultimately, the patient’s Fitzpatrick skin type is used to determine the IPL treatment settings including energy fluence. The Fitzpatrick scale ranges from I-VI and is based on a patient’s ability to tan versus burn with sun exposure.139-141The fairest and most easily sunburnt complexions are categorized as a I on the scale and the darkest skin tones that never experience sunburns as a VI.139-141 Accurately assessing where a patient falls on the Fitzpatrick scale is critical to determining if a patient is a candidate for IPL, as patients with darker skin tones are less likely to tolerate IPL and are more prone to side effects such as burns, blisters, and depigmentation as a result of a higher amount of energy absorption due to a greater presence of pigment in the form of melanin.17,138 Therefore, patients with a skin type of V or VI on the Fitzpatrick scale are not considered candidates for IPL, as OptiLight is indicated for the treatment of Fitzpatrick skin types I-IV.10,17,142 If a patient’s skin type is uncertain, it is recommended to apply a “test shot” prior to performing a full treatment to assess the patient’s reaction and tolerance, which will be discussed further later in the guide.
Contraindications and additional findings of note when performing IPL
There are a several contraindications and relative contraindications to be aware of when considering IPL for a patient. As previously discussed, patients displaying higher Fitzpatrick skin types, especially V-VI, are at higher risk for adverse events, such as burns or blistering. Therefore, patients with higher Fitzpatrick skin types (i.e. Fitzpatrick V and VI) are contraindicated for treatment with OptLight.10,17,142 Additionally, any areas of tattooing, including tattooed eyeliner, should be avoided as treating over the tattoo pigment can result in significant skin irritation and depigmentation. Treatment in the presence of sunburns, healing wounds, or active herpetic infections in the treatment area should be avoided, as should treatment in cases of recent cosmetic procedures.143Additional contraindications for OptiLight include: ocular surgery or eyelid surgery within 6 months prior to the first IPL session, neuro-paralysis in the planned treatment area within 6 months prior to the first IPL session, uncontrolled eye disorders affecting the ocular surface (such as active allergies), pre-cancerous lesions, skin cancer or pigmented lesions in the planned treatment area, uncontrolled infections or uncontrolled immunosuppressive diseases, ocular infections within 6 months prior to the first IPL session, prior history of cold sores or rashes in the perioral area or in the planned treatment area (such as Herpes simplex 1 and 2, systemic Lupus erythematosus, and porphyria), use of photosensitive medication and/or herbs within 3 months prior to the first IPL session that may cause sensitivity to light exposure (such as isotretinoin, tetracycline, doxycycline, and St. John's Wort), radiation therapy to the head or neck within 12 months prior to the first IPL session or planned radiation therapy within 8 weeks after the last IPL session, treatment with a chemotherapeutic agent within 8 weeks prior to the first IPL session or planned chemotherapy within 8 weeks after the last IPL session, and a history of migraines, seizures, or epilepsy.143
Other considerations when performing IPL include melasma and scarring. These conditions are not contraindications, but it may be advisable to avoid direct treatment to areas of melasma or deep scarring during the course of the procedure. Melasma has been shown to display hyperpigmentation and darken after being treated with IPL.144 However, it is worth noting that IPL has also been used to treat melasma, therefore the use of IPL on this condition is somewhat controversial.144,145 The concern with treating areas of deep scarring is more related to comfort than any detrimental effects, as IPL has actually been shown to improve the appearance of scarring,106 but when IPL is applied directly to an area of scarring, the tissue may react adversely to treatment as the tissue is denser and may contain more pigment resulting in greater energy absorption that can cause blistering or irritation.
Another somewhat controversial area is the use of IPL in the context of systemic lupus erythematosus (SLE). SLE often presents with an erythematous, malar rash on the face which is generally considered a contraindication for the use of IPL, as light exposure can potentially exacerbate the condition.146,147 However, there has been a documented case of improvement in facial erythema in a patient with active SLE with IPL treatment, and it has been suggested that IPL may be a potential treatment for the cutaneous manifestation of the disease.146,147 So, the presence of SLE may also be a relative contraindication, however, any cases should be approached with caution and all risks, benefits, and alternatives discussed with the patient. Therefore, there is a degree of clinical judgment to be exercised when performing IPL treatment.
One commonly questioned potential contraindication to IPL treatment revolves around the concurrent use of oral doxycycline. Doxycycline is commonly used in the treatment of DED and MGD.30,148,149 However, one of the potential side effects of doxycycline use is increased photosensitivity which makes the patient more prone to skin irritation when exposed to sunlight. For this reason, a common question is if this means patients taking doxycycline are at increased risk of an adverse skin reaction from IPL treatment due to it being a light-based therapy. However, it has been shown that patients concurrently taking doxycycline and receiving IPL do not experience any adverse photosensitivity-related effects.150 The suggested reason for this is that the wavelengths responsible for inducing sunburns and the photosensitivity-related side effects of doxycycline are part of the ultraviolet spectrum, which are not among the wavelengths used in IPL therapy.150Additionally, the dosages of doxycycline typically used in treatment of DED and MGD are usually lower than the standard antibacterial level, as it retains anti-inflammatory properties even at lower dosages,30,148,149which also reduces the chances of side effects like photosensitivity.
Accurately determining a patient’s skin tone using the Fitzpatrick Scale is a crucial step to ensuring a well-tolerated OptiLight treatment. Skin tone sensors can be helpful adjunct instruments when the results of the Fitzpatrick questionnaire are not definitive. Photo courtesy of authors.
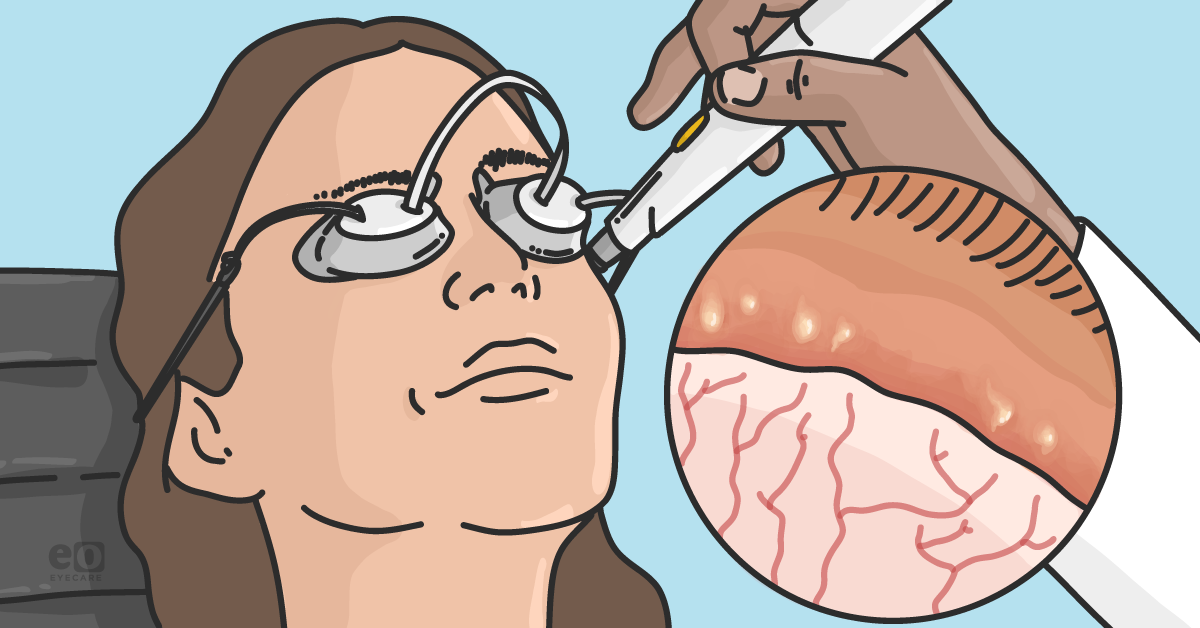
How is OptiLight performed?
OptiLight IPL treatment for DED and MGD is applied to the skin overlying the cheeks and nose in a tragus to tragus pattern with ultrasound gel covering the treatment area and protective adhesive eye patches in place with opaque goggles over top. This is primarily where telangiectatic blood vessels reside and feed the inflammation of the eyelids.10,17,30 Treatment spans four to five sessions that are usually scheduled 2-4 weeks apart (no sooner than 2 weeks and no longer than 4 weeks).10 Subsequent maintenance treatments typically consist of one treatment per year,26 however, some patients require more or less frequent treatment depending on the severity of their condition.
IPL uses a xenon flash lamp which emits wavelengths of light from 400-1200 nm.17,68 As previously mentioned, cutoff filters are then used to transmit the desired wavelengths depending on the goal of treatment. The OptiLight device uses a standard 590 nm filter for treatment of DED and MGD, which corresponds to the yellow, orange, and red portion of the visible light spectrum as well as near-infrared light.95,96 Additionally, settings for skin pigmentation based on the Fitzpatrick scale and energy level to be delivered in the form of fluence are determined for each specific patient. The standard lightguide is an actively cooled, rectangular (15 x 35 mm) sapphire crystal which will be the primary tip used for most treatments, whereas the OPT handpiece utilizes a smaller cylindrical (6.4 mm diameter) tip that is ideal for treating hard-to-reach places and when precise treatment is needed. When a shot is applied to the target tissue, the OptiLight device uses Optimal Pulse Technology (OPT) to employ a triple-pulse pattern in which the device emits three pulsed flashes of light of a duration of 4-20 ms per pulse with a 5-150 ms relaxation time between pulses (with standard settings of a 6 ms pulse duration and a 50 ms delay between pulses).
The IPL handpiece allows for treatment of large areas while the OPT handpiece is ideal for hard-to-reach areas or delicate regions.
Pre-procedure
After a patient has been determined to be an appropriate candidate for IPL treatment, their Fitzpatrick skin type, as discussed in the previous section, is determined using a questionnaire. Based on the patient’s responses they are assigned a Fitzpatrick number from I-VI, with Fitzpatrick skin types I-IV being indicated for treatment with OptiLight. This assigned skin type will determine the settings to be used for treatment. However, it is important to note that there is more to determining a patient’s Fitzpatrick skin type than just the questionnaire results, as the results may not accurately reflect the patient’s current skin tone. For example, a patient may state they burn easily, suggesting a lower Fitzpatrick skin type, such as I or II, but they live in a warm, sunny climate and have developed a significant tan, so now they have a “true” Fitzpatrick skin type that is closer to a III or IV. Additionally, even patients with very fair skin can have a higher-than-expected Fitzpatrick skin type if they have significant rosacea. The reason for this is that in cases of significant rosacea the development of telangiectatic vessels can result in a reddish complexion. As discussed, the basis for IPL is light energy absorption by pigment, and both these cases illustrate examples where pigmentation is greater than expected either due to an increase in melanin from tanning or the presence of vessels carrying hemoglobin-rich red blood cells. Therefore, it is advised to double check a patient’s Fitzpatrick skin type by either using a Fitzpatrick sensor device or visually comparing the patient’s skin tone to the expected Fitzpatrick number when there is uncertainty. In cases of discrepancy, it is recommended to err on the side of caution and select the higher of the two Fitzpatrick skin types, or to use the lower Fitzpatrick skin type but also use a lower energy fluence as most adverse effects are associated with using higher fluence levels.138
Determining the most accurate Fitzpatrick skin type and fluence level are critical steps, as the best indicators for potential adverse effects of IPL treatment are the patient’s level of skin pigmentation and the fluence used.138 It is crucial to remember that the patient’s Fitzpatrick skin type and the fluence used have an inverse relationship. If a patient has a lower Fitzpatrick skin type, such as a I or II, then a higher fluence can be used as they have less pigmentation and will therefore not absorb energy as easily, whereas those with higher Fitzpatrick skin types, like III and IV, will have more pigment, so a lower fluence can be used as energy can be absorbed more readily. After the initial treatment session, if the patient responds well with no complications, then the fluence settings can be adjusted. Similarly, if a patient falls on the higher end of the scale (i.e. between IV and V) and there is a question whether the patient is a good candidate in general, a “test shot” can be performed. This typically involves applying one shot or triple-pulse to either an inconspicuous location on the neck or arm. The patient’s response to the test shot can then be evaluated one week later. If no adverse reactions occurred, then an initial treatment can be performed, though it is still best to be somewhat cautious and use a lower fluence or a lower number of shots, and then recalibrate as necessary for future treatments depending on their tolerance to the full treatment. If the patient experiences an adverse reaction, such as blistering or pigmentation change after receiving their test shot, then the procedure is contraindicated. A test shot should only be performed if the patient is considered a borderline candidate. If a patient is a definitive V or VI, then in most cases the risk involved with even a test shot should be avoided which will likely facilitate counseling on alternative therapeutic options.
The patient’s Fitzpatrick skin type and the energy fluence to be used are entered via the settings screen prior to performing treatment with OptiLight.
After the patient’s Fitzpatrick skin type has been determined, this information is used to input their treatment settings from a preset selection of options built into the OptiLight menus. The user will select the patient’s Fitzpatrick skin type and can use either the preset energy fluence or adjust the fluence if necessary. The treatment parameters will then be set when it is time to begin the treatment. Next the patient’s eyes are covered with adhesive eye patches and opaque goggles placed over top the eye patches. It is important to make sure the patient is not wearing any makeup or applied any skin product prior to the procedure, as this can interfere with the treatment, especially if the products contain colored pigments. If the patient is wearing makeup or has used some other product, then it must be removed completely prior to applying the ultrasound gel. It is recommended that only clear, transparent and fragrance-free gels be used to avoid any interaction with the emitted light and to avoid any allergies, respectively.
The supplies required for performing an OptiLight treatment include adhesive eye patches, opaque goggles, transparent ultrasound gel, and photoprotective eyewear. When performing a treatment with OptiLight, double eye protection is utilized, with goggles placed over top the adhesive eye patches. Photo courtesy of authors.
After the gel has been applied to the treatment area and adhesive eye patches and opaque goggles are in place, the treatment is performed. The operator should wear photoprotective eyewear while performing the procedure. The typical treatment pattern involves two passes with shots applied from tragus to tragus going over the cheeks and nose and below the eyes with the lightguide oriented vertically (which can be switched to a horizontal orientation as you follow the natural contour of the patient’s face) and the lightguide resting lightly, but firmly, against the skin to ensure complete contact. A more detailed description of the treatment protocol is provided below.
The standard OptiLight treatment pattern consists of pulses applied from tragus to tragus including over the nose.16
Performing an OptiLight treatment*
Lumenis protocol
Lumenis’ FDA-approved protocol involves placing adhesive eye patches over both eyes with opaque goggles then placed over top the patches. Transparent ultrasound gel is applied from tragus to tragus, below the orbital rim, and over the nose which serves as the treatment area. This area is then treated with an overlap of no greater than 1 mm between applications. The first pass is applied with the lightguide positioned in a parallel orientation (relative to the nose) and the second pass is applied with the lightguide positioned perpendicularly. This technique applies to both the use of the large rectangular (15 x 35 mm) lightguide and the OPT handpiece, with the Opti-Tip disposable cover discarded after use if the OPT handpiece is implemented. The ultrasound gel is then removed, and manual gland expression may be performed. The patient is then given the appropriate after-care instructions.
An example of a patient with adhesive eye patches in place before goggles are placed over top with ultrasound gel applied to the treatment area. Photo courtesy of authors.
*IPL andOptiLight are intended to be used by licensed practitioners, according to local rules and regulations.
Four quick tips for performing OptiLight
Once you understand the protocol for performing the OptiLight procedure, treatment is relatively straightforward. However, there are some tips and tricks that can potentially improve the efficacy and comfort of the procedure.
- Patient Comfort Level: If at any time treatment starts to become uncomfortable for the patient, you can take a short break between shots, often only a few extra seconds are needed to improve comfort. If you are trying to decide between fluence levels, you can start the treatment at a lower fluence with the first pass and increase the energy if tolerable for the second pass. You can also decrease the fluence at any time if needed.
- Fitzpatrick Skin Type: If a patient is between Fitzpatrick skin types, it is best to go with the higher skin type and adjust the fluence accordingly.
- Applying Light Pressure: When performing the treatment, you want to apply light pressure to ensure contact with the skin, however you do not want to apply too much pressure, especially if you are treating over an area with substantial telangiectasia as too much pressure will cause blanching of these vessels, which will decrease blood flow, and, in turn, decrease the presence of the hemoglobin rich red blood cells that function as the treatment target and absorb the light produced by the IPL.
- Sun Protection: It is also critical to emphasize the importance of proper sun protection after treatment, so we recommend having sunscreen in-office that the patient applies immediately after the procedure to ensure they are protected when they leave as well as to underscore the importance of avoiding sun exposure during the treatment period.
Post-treatment gland expression
The performance of manual meibomian gland expression immediately following IPL treatment is somewhat controversial. The reason for this is the uncertainty surrounding the exact mechanism behind IPL’s effect on the meibum contained within the meibomian glands. As previously mentioned, it has been proposed that the heat generated by IPL melts any clogged oil present in the glands, however, it has been shown that the heat produced dissipates quickly and is likely insufficient to facilitate melting.16,102,103 Therefore, it is more likely that IPL alters the clogged oil photochemically by altering the bonds of the fatty acids present in the stagnant meibum, rather than through thermal melting, as the meibum undergoes a phase transition from a gel to a liquid crystalline structure rather than undergoing a state change from a solid to a liquid.142,15 If this is the case, manual expression following the procedure is unnecessary and closer to a “cold expression” which is both uncomfortable for the patient and relatively ineffective.14,65 Therefore, we have found that in cases where expression is still warranted after IPL, the best results are achieved when pairing IPL with a dedicated thermal pulsation treatment such as LipiFlow, iLux, or TearCare, as it has been shown that IPL and thermal pulsation appear to have a synergistic effect when used in tandem.152,153
After care
A major benefit of IPL treatment is very little after care is required. However, it is important to advise patients to avoid sun exposure (especially tanning which should be avoided entirely) and wear sunscreen (SPF 30 or higher) and/or a hat for the first 2 weeks following treatment, especially within the initial 48 hours, as the skin is more sensitive and UV light is damaging and can have a negative impact on the regenerative nature of the treatment.154-156 It is best to have the patient apply sunscreen before leaving the office after treatment has been performed. Additionally, they should avoid the use of any abrasive facial scrubs or retinol containing products, as retinoids can be damaging to the meibomian glands.10,157,158 Typically, the treatment is very well tolerated with the most common side effect being mild redness and irritation, similar to a mild sunburn, which is transient and dissipates quickly.17 However, if the patient finds the irritation to be bothersome, a gentle skin moisturizer is often adequate to provide comfort. It is also important to remind patients to continue using their other prescribed dry eye treatments as directed, as the IPL treatment will be most effective when used in tandem with their other therapies.
Follow-up and frequency of future treatments
The same procedure will be repeated every 3-4 weeks for four total treatments. Timing treatments around patient schedules can sometimes be challenging, so treatments can be repeated in as short as 2 weeks or up to 5 weeks later; however, for best results it is recommended to stay within the 3-4 week range. At the fourth treatment, we explain the post-treatment follow-up schedule. We typically see patients back 4-6 weeks after their final treatment to evaluate their progress. This follow-up visit involves repeating all testing performed prior to treatment including meibography, tear meniscus height evaluation, lipid layer analysis, and tear breakup time, and we recommend discussing the impact IPL had on each test.
If not done previously, this is also a good time to discuss the need for repeat treatment in the future. If the patient is doing well at this visit and there are both subjective and objective improvements in signs and symptoms, then a repeat maintenance treatment will likely not be necessary for 6-12 months.142,159,160 If, however, the patient has not yet displayed the desired improvement, it is likely that a fifth or even sixth treatment will be necessary, which can more commonly occur in patients with severe DED and MGD, especially those with significant meibomian gland loss. In some cases, a patient will display improvements in their objective testing but not in their symptoms. In these cases, we reassure them that it is not uncommon for improvement in symptoms to lag behind improvement in their objective signs. We have found these patients to inherently be candidates for a fifth treatment or the addition of another outside therapy.
As discussed, after the initial series of four treatments, patients will often require maintenance treatments periodically as time passes. However, the frequency and number of treatments needed are often patient specific in our collective clinical experience. Typically, most patients will need a repeat treatment between 6-12 months after their initial series.142,159,160 Often this will only require one to two treatments rather than a full series of four, but, in general, the longer the time that elapses between the first series and the repeat treatment, the more likely the patient will require more than one session. It is best to explain that future maintenance treatments will likely be necessary when first discussing IPL as a treatment option. Having this discussion will both set expectations and make patients aware that the treatment can easily be performed again if they notice any regression in their symptoms with time.
It is also important to note that some patients will require, or desire, more frequent treatment than the standard four sessions followed by a maintenance treatment every 6-12 months. We have found that some patients with significant meibomian gland loss, such as the gland loss experienced after chemotherapy, respond incredibly well to routine monthly treatments when other therapies have failed to provide adequate relief. Others with less severe but still significant DED may need treatment every 3-4 months for sustained improvement.
Additionally, some patients find that they are able to discontinue other therapies when being routinely treated with IPL. In fact, they prefer to do regular IPL treatments as a way to reduce their reliance on therapies that require daily use. The key to determining treatment frequency is to listen closely to the patient and educate them on what to look for after treatment. For example, as part of patient education we explain that most patients will eventually need maintenance treatment which typically occurs between 6-12 months, however this can vary. Therefore, they should carefully monitor their symptoms. If they notice that they were initially doing well after IPL but start to notice their symptoms are returning even with continuity of prescription treatments, then that is a telltale sign it may be time for repeat maintenance treatment.
Discussing OptiLight with patients and patient education
Explaining IPL and how it helps treat dry eye
As is true with any procedure or treatment, patient education is the key component into successfully implementing OptiLight into a practice. This begins with an easily understandable explanation of how IPL works, why they as a patient are a good candidate, how IPL will help their condition, and what to expect from the procedure. We recommend going over a patient’s testing results directly with them during their exams. For instance, showing them a picture of their meibomian gland loss through meibography or slit lamp photos of telangiectatic blood vessels of their eyelids can go a long way in helping them understand their condition. By thoroughly explaining a patient’s condition and how IPL will help each element of their dry eye, patients will better grasp the benefits of the procedure and will more likely desire to pursue treatment. It is important to remember that dry eye patients are seeking relief from their symptoms, and many have tried numerous treatments without experiencing the improvement they were hoping for, so they are often eager to try something new. Therefore, if you can clearly explain how IPL will specifically help improve their condition, that is often all that is needed to move forward with treatment. In our practice, we have found the vast majority of patients to be receptive to treatment after describing the various ways IPL treats dry eye and how it will specifically help them.
Below is a sample patient education script that we would use with a typical dry eye patient in our clinic*:
“IPL has been used for years in dermatology to treat many different skin conditions including age spots and wrinkles. The main mechanism of the treatment is energy delivery. The bright flash you will see during treatment is just energy in the form of light. When we do the OptiLight procedure, the light energy travels to the meibomian glands, which is thought to stimulate them, which improves their structure and function. This stimulation helps the glands make new, better-quality oil, and the energy delivered helps break apart any clogged oil that is blocking the glands. Additionally, the energy can also help close off the spidery blood vessels around the eyes and lids, especially in ocular rosacea, that cause inflammation, so this decreases the number of inflammatory factors that reach the eyes. The treatment also potentially decreases the number of mites and bacteria present on the lids and lashes as well. Also, the energy delivered stimulates skin cells to produce more collagen which can tighten skin and improve lid position which potentially improves blinking mechanics. This improved lid position and blinking behavior can increase oil secretion from the meibomian glands and improve spreading of that oil over the eye’s surface which helps stabilize the tear film that covers and protects the surface of the eyes.”
*IPL andOptiLight are intended to be used by licensed practitioners, according to local rules and regulations.
Patient education is a key component of successful implementation of OptiLight. Patients often ask how treating the area around the eyes helps their dry eye. A helpful demonstration involves using a transilluminator pressed against your thumb to illustrate how a single point source of light can illuminate and reach a much larger area beyond simply the head of the transilluminator. Photo courtesy of authors.
Another critical component of successful use of IPL is setting expectations. In our experience, it typically takes most patients 3-4 treatments before they can notice a difference in their signs and symptoms. So, it is best to always ask the patient before each treatment how they are doing. If they are seeing improvement after the first or second treatment, we let them know that they are ahead of schedule and it is an encouraging sign. If they have not noticed any major differences after the first few treatments, we reassure them that is completely normal and remind them that some patients do not experience improvement until after the third, fourth, or in some cases, even the fifth treatment. This is the reason we also tell patients on the day of the first treatment that they likely will not be able to tell a difference after the first two sessions, but not to be discouraged because this is completely normal. This helps set expectations, assuage any concerns, and improves the patient’s confidence in the treatment.
Before the first treatment, we usually describe what to expect in the following manner:
“I see today is your first treatment, so I want to go over what to expect. After this first treatment, most patients do not feel much of a difference in how their eyes feel, and that is completely normal. The reason for this is that the treatment is based around energy delivery and after this first treatment there is not usually enough energy delivered to make a noticeable difference, but it sets the foundation for your next three treatments. After the second treatment a small number of patients may start to notice an improvement in their symptoms, but it is not usually until their third or fourth treatment that this difference is noticeable. So, there is no need to worry if you do not notice a difference right away, you are still right on track. From a comfort standpoint during the treatment, you will likely see a bright flash of light even though your eyes are covered, and you may feel some heat or a snapping sensation like a rubber band, but this is normal and should pass quickly. Afterwards your skin may be a little red and tight, like a mild sunburn, but this is normal too. If you find that it is bothersome, we recommend a gentle moisturizer to help with comfort.”
Additionally, you should be prepared to answer any questions the patient may have. Some of the most common questions include how many treatments are needed, will the other treatments they are using still be necessary, and is this guaranteed to work?
While we have already discussed the standard base number of treatments and the likely need for future maintenance treatments, the other two questions are also crucial to setting proper expectations.
“Based on the data and studies available, most patients need four treatments to successfully treat dry eye. This is the reason we recommend a series of four treatments as this is the number of treatments needed to deliver the amount of energy necessary to improve your dry eye. It is also likely you will need repeat treatment in the future to maintain improvement, but this usually will not be needed for 6-12 months. IPL works best when used alongside your other dry eye therapies. So, while IPL may not replace your other treatments, you may not need to use some of them, like artificial tears, as frequently after treatment. With IPL, like all medical treatments and procedures, nothing is guaranteed. However, we have found great success with the treatment and the majority of patients experience an improvement in their symptoms and objective testing. In some cases, they experience an improvement in their testing before their symptoms, but it is extremely rare that a patient does not experience some benefit from treatment. Regardless, we will do everything in our power to ensure the best outcomes possible.”
And while IPL is often considered a “second line” treatment, it is best to avoid assuming patients with even mild dry eye are not interested in the procedure. Many patients want to be as proactive as possible, so we recommend at least discussing it with all your dry eye patients to bring awareness to the option. In our experience, after explaining how IPL works, we have found a significant number of patients voice a desire to undergo the treatment, even if it is their initial exam and they are just beginning foundational dry eye therapy, and in many cases, they wish to have the procedure performed that same day if possible. So, again, it is best to empower the patient to make the decision by providing all the necessary information to make an informed choice about their treatment.
After the patient has a firm understanding of how IPL works, it is easier to have an informed discussion around cost-benefit analysis. IPL is not covered by insurance, and although this is typical for most dry eye-related treatments, it is often the most common barrier to treatment for patients and area of discomfort for their doctors to discuss. We have found the keys to this discussion are being upfront and honest, keeping the focus on the patient’s condition, and empowering the patient to take ownership of the decision. As a doctor, it should never be our job to “sell” our patients on something or to pressure them into the decision, in fact, we routinely tell patients we do not want them to do the procedure if they are not 100% comfortable with the decision. It is simply our job to educate them on their condition and the benefits of the procedure and answer any questions they may have to help them make the decision that is right for them. By using this straightforward approach, we have found great patient acceptance.
Additionally, it is a good idea to educate all staff members on the basics of IPL treatment. Not only does this allow them to answer any questions that may arise from patients, but also creates a consistent message that will build the patient’s confidence in both the procedure and your practice.
It is best to empower the patient to make the decision by providing all the necessary information to make an informed choice about their treatment.
How to introduce OptiLight into your practice
Incorporating OptiLight
When deciding to implement a new in-office treatment, the logistics surrounding it are often just as important as the procedure itself. A benefit to IPL is its relatively short treatment time. The whole process from start to finish, depending on the treatment protocol utilized, typically takes around 15 minutes, often with 5-10 minutes of that being hands-on time for the doctor. So, in our practice we schedule each IPL session as a 15-minute appointment slot. We have also found that creating a “procedure day” works best for our office flow by scheduling all IPLs on the same day, back-to-back. This allows for a consistent flow and maximizes the number of IPLs that can be performed without disrupting a routine exam schedule. Additionally, it is key to have a thorough discussion and answer as many questions as possible before the day of treatment, as the most common source of disruption to the flow of a procedure day is extensive patient questions or concerns that would have been better addressed beforehand.
From a packaging and bundling standpoint, there are many potential options for IPL, from choosing a number of individual IPL sessions to combining IPL with other procedures such as thermal pulsation. We have found that bundling all four treatments together makes the most sense as this is considered standard practice, so offering individual treatments is less ideal clinically, at least for the initial treatment series. Additionally, as most patients do not experience significant improvement until the third or fourth treatment – if a patient only purchases one or two treatments and experiences no improvement, they may lose confidence and choose not to receive the full course of treatment, which is a disservice to both the patient and the doctor as the patient does not receive the standard of care and feels dissatisfied with their experience, and the doctor is not able to provide the care they desire. In regard to maintenance treatments after the initial series, there is more flexibility. We offer both individual treatments as well as another full package of four treatments at a discount. The way we have this setup is that if a patient chooses to purchase a package of four treatments but only needs one, then we note in their record that they have three future treatments available to use whenever they see fit. We also offer bundles including both IPL and thermal pulsation procedures for patients who are interested in both treatments.
OptiLight is a powerful treatment tool that can transform both the way you manage dry eye and your practice in general.
Summary
Dry eye is a multifactorial disease with several potential causes and contributing factors. The multifaceted nature of the condition means many separate treatments are required to address the different elements of the disorder. This same challenge makes OptiLight a unique and powerful treatment option as it addresses several elements of the disease in a single modality. Lumenis light treatment is the first and only IPL device approved for the management of dry eye and its most common cause, MGD. Through the delivery of light energy, OptiLight can manage dry eye by improving meibomian gland structure, function, and meibum quality, as well as decreasing the number of inflammatory factors present in the tear film and on the ocular surface. Invariably, IPL treatment might also eliminate or reduce the proinflammatory telangiectatic blood vessels associated with ocular rosacea and while eradicating Demodex mites and decrease the bacterial burden on the lids and lashes along with improving skin quality which may improve blinking mechanics.
All of these potential benefits make OptiLight an optimal treatment choice for long-term dry eye patients and newly diagnosed patients alike. Performing the treatment is well-tolerated and quick, making integration into even the busiest practices easy and straightforward. Adding OptiLight benefits both patients and practices, which ultimately allows dry eye practitioners to provide the best care possible for even the most challenging dry eye patients.