In recent years, we are hearing references to what are called the “Social Determinants of Health” (SDoH). This is a term that may apply to our patients and have an effect on the care we provide for them and the outcome of that care when treating various pathologies.
It is important that eyecare practitioners (ECPs) understand the SDoH concept and its effect on their practices.
What are social determinants of health?
The concept of SDoH first started in the early 1970s when McKeown coined the term “determinants of health.”1 Then, in 1999, Marmot and Wilkinson published “Social Determinants of Health” and discussed two critical concepts that helped to better define SDoH.
Those concepts were:2
- “Differences in health between population groups is due to the characteristics in society, not differences in healthcare.”
- “When people change social and cultural environments, their disease risks change."
The World Health Organization (WHO) developed a formal definition of SDoH in 2008, which has subsequently been embraced by the Centers for Disease Control and Prevention (CDC). That definition is: “Social determinants of health (SDoH) are the non-medical factors which influence health outcomes.
They are the conditions in which people are born, grow, work, live, and age, and the wider set of forces and systems shaping the conditions of daily life.”3 These factors can be things such as food supply, housing, transportation, income, and education.
Affordable Care Act
In 2010, the Affordable Care Act included SDoH as a factor to be considered for emerging healthcare policy.4 The COVID-19 pandemic magnified how lower-income patients may have been more likely to develop severe COVID-19 problems.
The American Academy of Emergency Medicine concluded that “low-income groups use fewer inpatient services, are prone to severe illness and death from COVID-19, and treatment in this group has a lower chance of success.”5
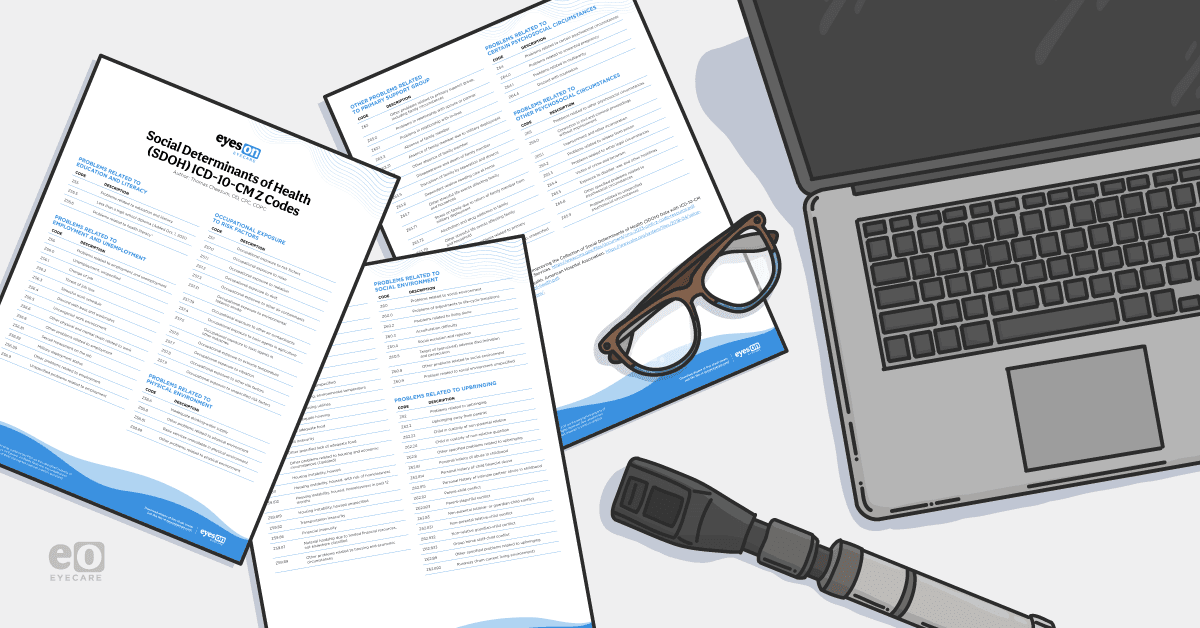
Over the past few years, dozens of International Classification of Diseases, Tenth Revision (ICD-10) diagnosis codes related to SDoH have been added in the Z55 to Z65 section of the ICD-10 code book.
These codes may be used for those applicable patients whose healthcare may be affected by things such as access to food supply, transportation, income, housing and others as the CDC has concluded that these factors “whose distribution across populations effectively determines length and quality of life.”6
Download the Social Determinants of Health ICD-10-CM Z Codes Cheat Sheet
The role of SDoH in eyecare
Eyecare providers may wonder how SDoH affect their practices, to contextualize their importance, think about these items:
- If a patient can not afford or have access to transportation, does that affect your ability to care for sight-threatening conditions, such as glaucoma? What if the patient can not come to appointments on a timely basis?
- If a low-income patient has to choose between paying for their medications, feeding their children, or paying their utility bills, are they at higher risk of complications from ocular disease?
- Is an ocular infection you are treating for a homeless person who has limited access to sanitary living conditions likely to respond to your care, assuming they can even afford their medication?
These are things any ECP needs to take into account, especially when they deal with patients who may fall into these at-risk populations for these non-medical factors.
Examples of SDOH codes
Since these factors may increase the complexity of the ocular disease problems you are treating for some of these patients and also increase the risk of ocular morbidity, it may result in the ability to bill using a higher level of Evaluation and Management (E/M) code.
For example, if a patient has glaucoma and can properly use their medications and comply with their exam schedule, if their glaucoma is stable and their intraocular pressure (IOP) is at target pressure, a progress check visit would most likely be coded as a 99213.
Conversely, a low-income patient who has difficulty getting transportation to attend their periodic visits and, instead of being able to come in every 4 months, is only able to come in every 7 to 8 months and may not be able to afford to use their medications as prescribed, has a higher risk of glaucoma progression since the treatment can not be monitored properly.
Therefore, the complexity and risk of dealing with their glaucoma rises to a higher level which would then qualify as a 99214 E/M code. In order to properly bill for these SDoH-related issues, the provider has to properly document the specific SDoH problems the patient may have that affect their care.
This could include poor access to reliable transportation (Z59.82) or homelessness (Z59.02) in the patient records. Then, when billing the exams for the patient, the coder should list the disease diagnosis code(s) first, followed by the applicable Z55 to Z65 code(s).
Final thoughts
In conclusion, it’s important that you and your staff listen to your patients when they are seen to ascertain if they are subject to any of these SDoH factors which may affect their ocular and general health and take those factors into consideration when you formulate your care plan for the patients.
Document those problems in the record and, if possible, perhaps refer them to various prescription drug assistance programs—either the federal government or state government or sponsored by pharmaceutical companies—which may allow low or no-cost access to needed medications and perhaps government and non-government resources to help with such things as housing and access to food.
As members of the healthcare community, we must learn to care for the patients as a whole and not just focus on ocular-specific problems only.