Double vision, or diplopia, can be a daunting concept for many optometrists. This is completely understandable, as a complaint of diplopia can stem from something as mild as
convergence insufficiency to a life-threatening neurologic disease. But fear not, as this article will guide you with the appropriate questions to ask, and diagnostic tests to perform to isolate the affected ocular structure or muscle.
If your patient complains of double vision, the first question to always ask is: Does it go away with either eye closed?
Monocular Diplopia
The patient’s perception of diplopia may be misunderstood if they are actually experiencing image ghosting, glare, or
visual field defects. Confirm that the patient is seeing two physically separate images in one eye. Then begin to rule out causes of monocular diplopia moving through the ocular structures from ‘front to back’:
- Refractive error: High and/or irregular astigmatism
- Eyelids: Growths, chalazia, or tumors causing mechanical compression of the cornea
- Tear film: Dry eye disease
- Cornea: Opacities, scarring, dystrophies, pterygium, keratoconus, post-refractive surgery, ill-fitted contact lens
- Iris: Iridodialysis, polycoria, iridotomy, iridectomy
- Lens: Cataract, subluxation
- Vitreous: Opacities, foreign bodies
- Retina: Maculopathies including ERM, ARMD, macular holes or edema
Binocular Diplopia
Unfortunately, identifying the cause of binocular diplopia is not as systematic as monocular diplopia. That is why asking a thorough case history is crucial as it will often get you closer to the diagnosis before any testing.
Case History Questions
Are the two images separated horizontally, vertically, or diagonally?
- Horizontal: Suggests a medial or lateral rectus dysfunction
- Vertical: Suggests a CN 4 palsy or skew deviation
- Diagonal: Can result from various CN palsies or diffuse orbital disease
When was the initial onset?
- Longstanding (>3 months): Suggests either a decompensated phoria or a progressive disorder
- Acute (<3 months): Suggests a vascular event (hypertension, diabetes) or trauma
Is it worse at distance or near?
- Distance: Suggests a divergence issue
- Near: Suggests a convergence issue
Is it worse in a certain direction of gaze?
- Looking up: Suggests a CN 3 palsy or inferior oblique over-action
- Looking down: Suggests a CN 4 palsy
- Many or all directions: Suggests systemic disease (Grave’s, Myasthenia Gravis) or diffuse orbital inflammation
Is there a known history of childhood strabismus and/or particular head posture?
- Yes: Suggests longstanding deviation that is decompensated
Is there associated pain, headaches, or neurological symptoms?
- Yes: Suggests vascular event (hypertension, diabetes), optic neuritis, Giant Cell Arteritis, diffuse orbital disease (Grave’s, Myasthenia Gravis), or pituitary apoplexy
Was the onset after any recent ocular surgery, including refractive, cataract, glaucoma, strabismic, or retinal detachment surgeries?
- Yes: Suggests post-operative intractable diplopia
Diagnostic Tests To Consider
Now that you’ve assumed a few diagnoses as a differential, it’s time to open your clinical toolkit and identify which muscles are affected.
Cover Test and/or Maddox Rod Test
In addition to the unilateral and alternating cover test in primary gaze, use a Maddox rod lens to obtain subjective measurements. Either of these tests can confirm if the ocular deviation is comitant or non-comitant.
A comitant deviation means the ocular posture is longstanding. A non-comitant deviation suggests an acute event has taken place.
If your patient experiences binocular diplopia in primary gaze, a quick way to determine comitancy is to perform the Maddox rod test twice; once with the red lens over the right eye, and again over the left. This is performing primary versus secondary fixation. If the magnitudes of each result are greater than 10 prism diopters apart, this is a non-comitant deviation and likely an acute event.
If your patient experiences binocular diplopia in a particular gaze, it is wise to perform the cover test or Maddox test in that gaze and compare the magnitude of the deviation to what was measured in primary gaze. The same rules apply where the deviation is considered non-comitant if the magnitudes in each gaze are greater than 10 prism diopters apart.
NPC and Vergence Ranges
If your patient does not have a strabismus, perform NPC and vergence ranges to determine if they are experiencing an insufficiency or excess in divergence or convergence skills.
Performing vertical vergence ranges on a patient with a vertical posture will confirm a longstanding deviation if the break value is extended past 1-2 prism diopters.
Binocular Versions and Monocular Ductions
Versions are similar to EOMs but performed in all nine fields of gazes—making a ‘square’ pattern rather than an ‘H’. Have your patient fixate on a transilluminator binocularly and pay attention to the corneal reflexes. Move the transilluminator into all fields of gaze, watching for any misalignment of the corneal reflexes. This test will reveal any EOM under or over-action in the problematic gaze(s).
If you’ve identified a muscle restriction in a particular gaze, then it is time to perform the monocular ductions test. Have the patient fixate on the light again in the problematic gaze monocularly and compare the grading of the muscle restriction to the previous versions test.
On ductions testing, if the muscle position remains the same as versions, this suggests a mechanical muscle restriction (positive ductions test). If the muscle position improves to any extent and becomes better aligned with the transilluminator, this suggests a neurological muscle palsy (negative ductions test).
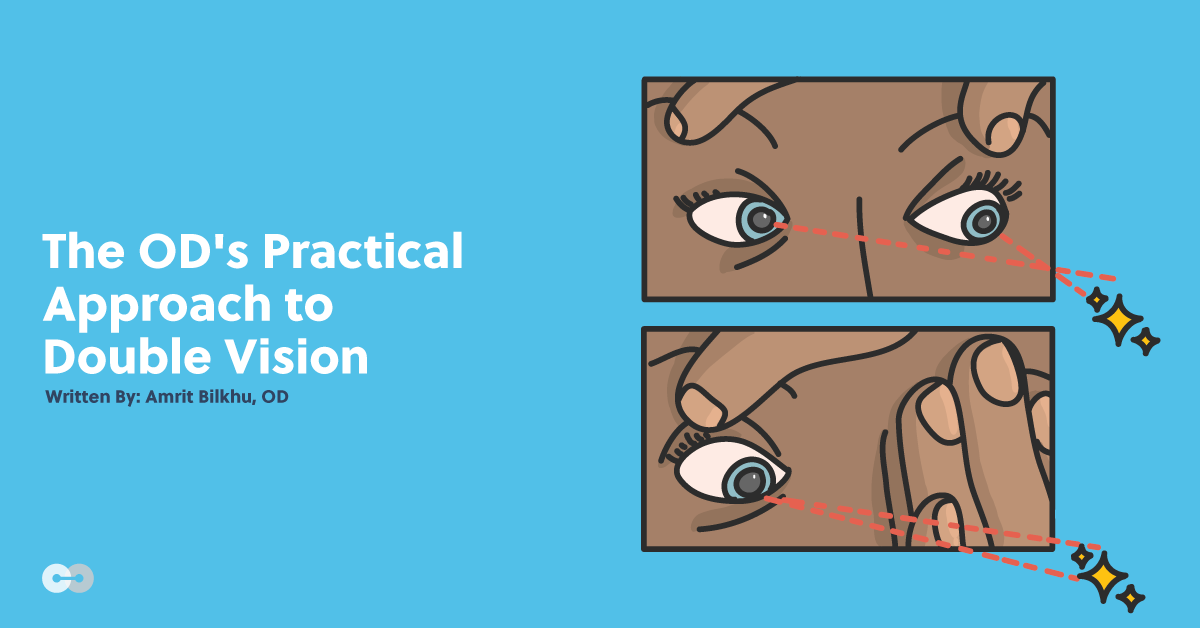
The top image shows binocular vision testing in left-down gaze where the patient has a right superior oblique muscle restriction. The visual axes are highlighted in red to demonstrate the misalignment of the right eye towards the light source. The bottom image shows monocular ductions testing. The thin red line indicates the previous visual axis when binocular. The thick red line indicates the movement of the visual axis further towards the light source when monocular, indicating a neurological restriction. This patient was diagnosed with a trochlear nerve palsy.
Slit Lamp Examination
Use the slit lamp to rule out signs of orbital diseases and space occupying lesions that cause diplopia. Check for proptosis, lid edema or retraction, signs of orbital inflammation (conjunctival injection, chemosis, erythema, uveitis), and signs of other systemic diseases including
Grave’s thyroid eye disease, Myasthenia Gravis, and Multiple Sclerosis.
Using the case history questions and examination tests discussed here will allow you to successfully identify the affected ocular structure(s) or muscle(s), narrowing down on your diagnosis in even the most challenging monocular or binocular diplopia cases.
Resources:
- Tan AK, Faridah HA. The two-minute approach to monocular diplopia. Malays Fam Physician. 2010;5(3):115-118.
- Dinkin M. Diagnostic approach to diplopia. Continuum Journal. 2014;20(4):942-965.