It’s the end of the day and your office receives a call from a patient in a panic. They describe their symptoms as sudden onset floaters, decreased vision, and pain in their left eye. You agree to see them on an emergency basis. A list of differentials immediately starts piling up in your head.
Once in your chair, your patient tells you their systemic and ocular histories are unremarkable except for a previous doctor stating they have a “pigmented scar” in the back of their left eye. You are racking your brain for the possibilities.
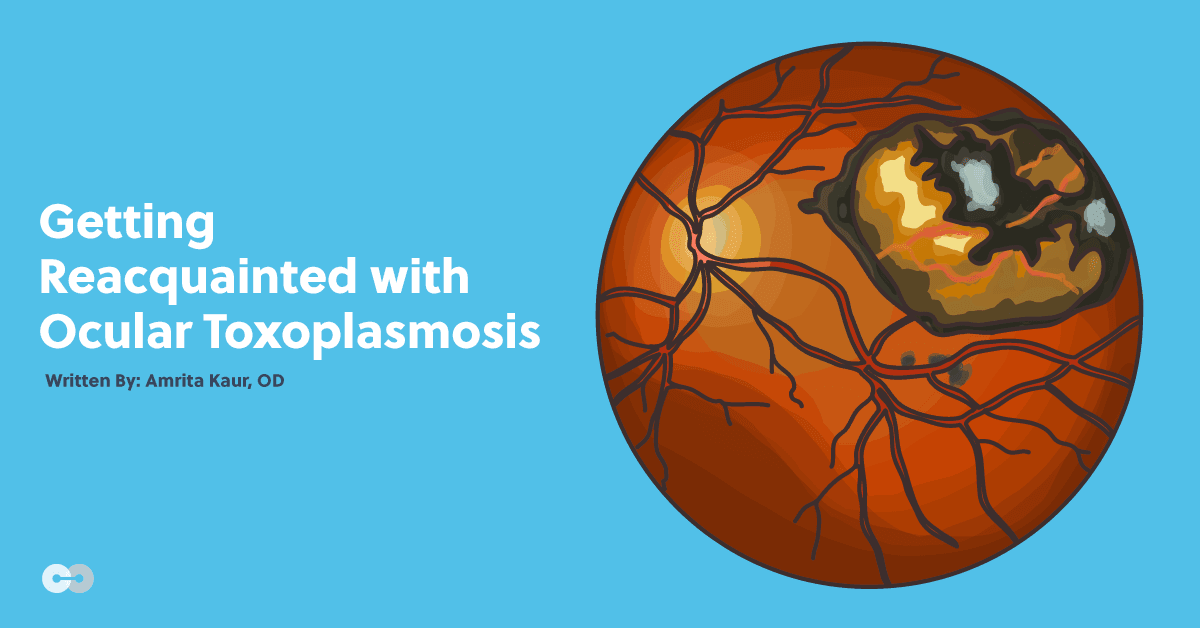
You pick up your BIO to take a look at their fundus. You first see heavy vitreous cells, and then a peculiar fluffy white retinal lesion adjacent to a chorioretinal scar, obscuring your view of the macula. What do they have?
They are presenting with ocular toxoplasmosis (which you knew because you read the title of this article).
It’s been a minute since I took boards. Can you brush me up on the details?
Systemic toxoplasmosis is an infection induced by the parasite Toxoplasma gondii. T. gondii can be acquired or congenital. Adults can be infected by ingesting contaminated foods, water, or undercooked meat. They can also acquire it from exposure to infected cat litter.1,2
So think twice before you order that rare steak! Toxoplasmosis can also be acquired congenitally through the placenta if a pregnant mother becomes infected during pregnancy.
It is estimated that about one billion people worldwide are infected with the parasite, although most of this population is asymptomatic.1
Ocular toxoplasmosis occurs in about 25% of the population infected with systemic toxoplasmosis.1 The ocular manifestation exists in both an active and inactive form.
While the mechanism by which systemic toxoplasmosis induces an ocular infection is not fully understood, it is believed the parasite reaches the eye via the bloodstream, and the host’s immune response converts the parasite to its cystic form.2
It may never cause any symptoms for the host, but the initial inflammation often creates a chorioretinal scar.2 This can create a fun little game of ‘Name that lesion!’ for the clinician. The cyst is believed to remain dormant in or adjacent to this chorioretinal scar and may reactivate at a later time to release the parasite (but we hope it stays inactive!).
The majority of immunocompetent patients who acquire ocular toxoplasmosis present with the inactive form and are asymptomatic. However, in those who are unlucky enough to have an active or recurrent infection, it is the leading cause of posterior uveitis worldwide.1,3 The active form is more likely to occur in immunocompromised individuals or those who acquired the disease congenitally.1,3
What do I need to look for as a clinician diagnosing ocular toxoplasmosis?
As mentioned earlier, the inactive form of ocular toxoplasmosis is benign and presents without symptoms. Those with past and inactive infection typically present with pigmented, inactive chorioretinal scars in the posterior pole. These self-limiting scars may vary in size, number, and location.
If multiple scars (satellite lesions) exist, it is likely that the initial scar became activated one or more times. These bouts of active chorioretinitis generally occur in the proximity of an existing scar and form new pigmented scars throughout the retina when said inflammation has resolved.3,4
Immunocompetent patients tend to have unilateral involvement. If the infection does reactivate, chorioretinitis is expected to be unilateral in 72-86% of active cases.2,5
Patients with active ocular toxoplasmosis present with a myriad of signs and symptoms. Presentations vary depending on location and severity of the inflammation, but the disease has a predilection for the posterior pole.2,3
The ocular symptoms in acute activation include new onset floaters, decreased vision, and pain. These symptoms are presumed to occur as a result of a ruptured cyst in a previously inactive scar, unless this is the initial infection.
The inflammatory response from the activated cyst creates a hallmark retinitis and overlying vitritis, inducing pain which corresponds to the severity of this inflammation. Severely decreased visual acuity may occur if the retinitis occurs within the macula.3-6
Upon dilated exam, you will often find a new fluffy-appearing lesion that is yellow-white in color, adjacent to an old chorioretinal scar when active ocular toxoplasmosis is present. Overlying the retinal inflammation, there is typically the classic presentation of “headlights in a fog” arising from dense cells in the vitreous.
Quite often, the posterior uveitis spreads to the anterior chamber, creating an anterior uveitis and possibly changes in intraocular pressure.3,5,6 Retinitis, vitritis, and anterior uveitis, oh my!
Be aware that toxoplasmosis can also present in the deep retinal layers, with the absence of uveitis, although this is atypical. In rare instances, more often with immunocompromised patients, you may also see optic disc edema, macular edema, or retinal vasculitis. If inflammation from the retinal necrosis or posterior uveitis is severe enough, serous or rhegmatogenous retinal detachment may occur from subretinal fluid or vitreoretinal traction.7-9
Those with congenital ocular toxoplasmosis tend to have the most severe complications and visual impairment. The majority of congenital cases present bilaterally and can be a significant cause of blindness.10,11
As with acquired ocular toxoplasmosis, chorioretinitis is the most common finding during active infection. These individuals may also present with strabismus, nystagmus, leukocoria, ptosis, or microphthalmus from the inability of the eyes and visual system to properly develop.11,12
Those with congenital disease or who are immunocompromised are far more likely to have macular involvement, larger areas of retinal necrosis, and to have acute reactivation of ocular toxoplasmosis throughout their lifetime.11-13
Confirming the diagnosis, treatment, and management
Clinical presentation is typically sufficient to diagnose ocular toxoplasmosis, but at times signs and symptoms can be misleading. In these cases, the diagnosis of toxoplasmosis infection is confirmed in the laboratory. Blood serum is analyzed via T. gondii Polymerase Chain Reaction (PCR) and antibody titers.3
You do not need to be bored with the details of how PCR works. It is only important to realize that PCR allows us to expose any presence of DNA from a foreign or infectious organism. Antibody testing allows us to determine if the individual has an active infection based on an active immune response.5 We can test antibody titers in the aqueous humor and the serum to determine if the patient specifically has an active ocular infection.3-5
It is also important to take a good history. The prevalence of T. gondii varies throughout the globe. In North America, Northern Europe, and Southeast Asia, the prevalence of the parasite is fairly low. South American and African countries carry a much higher prevalence. The parasite tends to thrive more in tropical countries or areas with warm climates. Ask your patients if they have recently done any traveling or have lived in these regions.13
Additionally, ask your patients if they possess any immunocompromising conditions. Discuss if they may have ingested undercooked meat, or plants from contaminated soil or water. Be wary of exposure to any animals, not just cats. A patient’s history and lifestyle may certainly help you confirm a diagnosis of ocular toxoplasmosis. Pay attention to the details.
Once we determine a patient has an active ocular toxoplasmosis infection, how do we treat them?
The first treatment goals are to reduce signs and alleviate symptoms of the active infection. We want to prevent or minimize any inflammatory process that may cause vision damage. Treatment is not typically required in inactive stages of the disease, except in rare cases when efforts are made to decrease the chances of active recurrence.
If symptoms are mild in a patient with a sound immune system, the inflammation may be self-limiting and resolve in four to eight weeks. More often than not, however, prompt treatment is indicated in active ocular toxoplasmosis. Anti-microbial therapy and steroids are commonly used.3-5
Often, acute toxoplasmic chorioretinitis requires combination therapy. Pyrimethamine and sulfonamides are the most commonly prescribed antimicrobials. Oral corticosteroids are typically used in conjunction with these. Dosage is dependent on patient size and severity of the infection, but usually starts aggressively with a quick taper.
If ocular signs and symptoms are severe, do not hesitate to also add a topical steroid—but be sure to monitor the intraocular pressure closely.5-7 Encourage your patients to drink lots of fluids, and consider a probiotic to alleviate GI symptoms.
Prognosis is variable but significantly better when diagnosis and treatment are addressed promptly. If necessary, antimicrobial therapy is sometimes used as a preventative treatment for immunocompromised patients as well.4,6
Pregnant women who acquire toxoplasmosis may take spiramycin for treatment, but be sure to communicate with the patient’s OBGYN first. Infants with active congenital ocular toxoplasmosis may be treated with a low dose of pyrimethamine with a quick taper, but again, be sure to discuss with the child’s pediatrician before prescribing.10,11
Be mindful of the fact that those with active or recurrent ocular toxoplasmosis are affected emotionally as well as physically. Anxiety and depression are common in those patients who suffer from severe uveitis or vision loss.
The repercussions of ocular toxoplasmosis can lower one’s quality of daily life. These patients may live in fear of recurrence and have a decreased ability to work. Consider directing them to counseling resources as seen appropriate, and keep low-vision resources accessible.14
Ocular toxoplasmosis is a multifaceted disease with many presentations and complications that as optometrists we need to be aware of. Given that ocular toxoplasmosis is an extension of systemic toxoplasmosis, it needs to be treated with an interdisciplinary approach.
Treating this disease presents an opportunity to work as part of a medical team. Treat ocular findings as you feel comfortable, but do not hesitate to collaborate with an ophthalmologist at any point. Maintain open lines of communication with the patient’s primary care physician, an infectious disease specialist, OBGYN, gastroenterologist, and even therapist if necessary.
Can you give me the CliffsNotes version?
What do you need to know about ocular toxoplasmosis?
- Take a good history
- Ask about travel to other regions, exposure to animals, lifestyle, and any previous immunocompromising conditions
- Do a thorough exam
- Pay attention to what aspects of the eye are affected and the severity of the conditions
- Dilate!
- Anticipate future complications and take measures to prevent them if possible
- Keep these patients on your radar and schedule follow-ups with them even if they are not symptomatic. It is often easier to prevent complications than to treat them!
- Keep lines of communication open with other health care specialists and treat or refer promptly
- Educate and reassure your patient
- Acknowledge your patient’s physical and emotional needs. Reassure them and make them aware of their resources
Now that you are reacquainted with ocular toxoplasmosis, be sure to keep it on your list of differentials when you have a patient with new onset floaters, ocular pain, or decreased vision. As optometrists, we have the power and responsibility to help optimize not only our patients’ visual outcomes, but also their overall wellbeing.
References
- Vallochi AL, Nakamura MV, Schlesinger D, et al. “Ocular toxoplasmosis: More Than Just What Meets the Eye.” Scand J Immunol. 2002 Apr;55(4):324-8.
- 2. Wu L, Roy H, et al. “Ophthalmologic Manifestations of Toxoplasmosis.” Medscape. September 29, 2015;http://emedicine.medscape.com/article/1204441-overview#showall.
- Butler, NJ, et al. “Ocular toxoplasmosis II: clinical features, pathology and management.” Clin Experiment Ophthalmol. 2013 Jan-Feb; 41(1): 95–108.
- Xiaoli, LV, et al. “Early diagnosis and successful treatment of acquired toxoplasmosis infectious retinochoroiditis.” Medicine (Baltimore), 2018 Jun; 97 (26).
- Park, YH, et al. “Clinical Features and Treatment of Ocular Toxoplasmosis. Korean J Parasitol, 2013 Aug; 51(4): 393–399.
- Holland, GN. “Ocular toxoplasmosis: a global reassessment. Part II: disease manifestations and management.” Am J Ophthalmol, 2004;137(1):1-17.
- Bonfioli AA, Orefice F. “Toxoplasmosis.” Semin Ophthalmol. 2005;20(3):129-141.
- Celebi AR, et al. “Retinal tear: an unusual complication of ocular toxoplasmosis.” Open Med (Wars), 2015 Dec 21;10(1):555-559.
- Bosch-Driessen LH, et al. “Retinal Detachment in ocular toxoplasmosis.” Ophthalmology. 2000 Jan;107(1):36-40.
- Kump LI, et al. “Ocular toxoplasmosis in pregnancy.” Clin Experiment Ophthalmol. 2005;33(5):455-460.
- Perry, DD, et al. “Congenital Ocular Toxoplasmosis.” J Natl Med Assoc, 1983 Feb; 75(2): 169-174.
- Melamed, J., Eckert, G., Spadoni, V. et al. “Ocular manifestations of congenital toxoplasmosis..” Eye 24, 528–534 (2010) doi:10.1038/eye.2009.140.
- Florence, RG, et al. “Epidemiology of and Diagnostic Strategies for Toxoplasmosis.” Clin Microbial rev. 2012 Apr; 25(2): 264-296.
- Canamary, AM Jr, et al. “Quality-of-Life and Psychosocial Aspects in Patients with Ocular Toxoplasmosis: A Clinical Study in a Tertiary Care Hospital in Brazil.” Ocul Immunol Inflamm, 2019 Oct 7: 1-9. doi: 10.1080/09273948.2019.1612453.