Corneal transplant (keratoplasty) is an ophthalmic surgery that replaces a portion of or the entire patient’s cornea with donor corneal tissue. The first successful human, full-thickness corneal transplant was performed in 1905 by Eduard Zirm, decades before organ transplantation took off in the medical community. Corneal transplant procedures opened the door to a new and improved way to treat previously irreversible cases of corneal blindness.
Types of corneal transplants
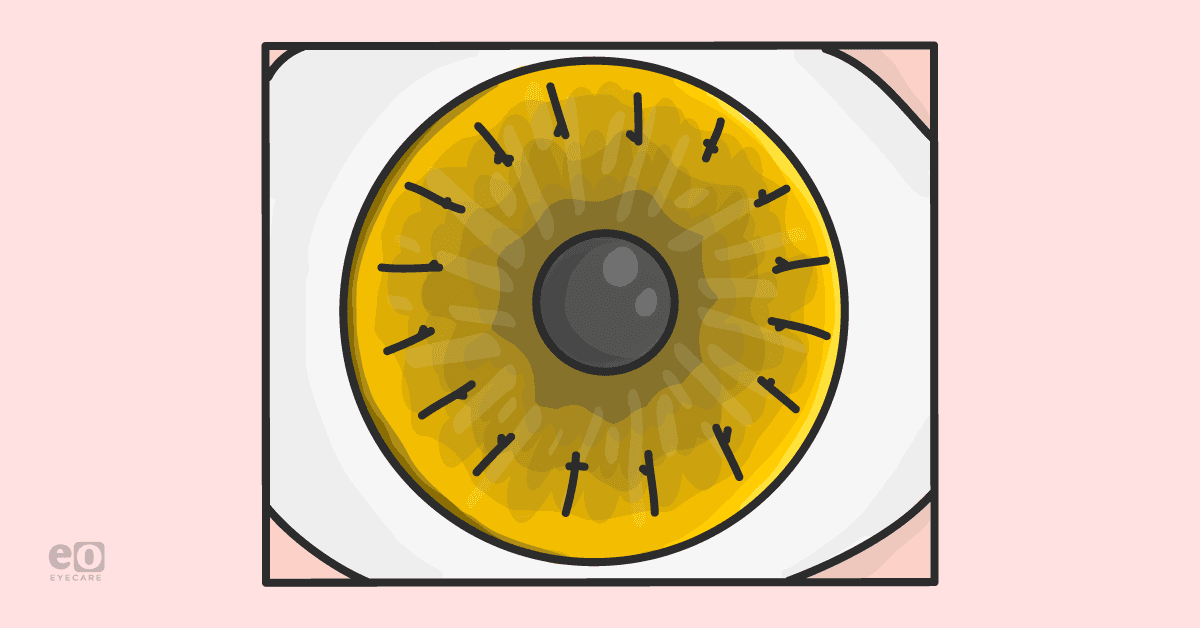
There are four main types of corneal transplants differentiated on what selective patient corneal tissue is being removed. The cornea is a transparent tissue covered by epithelium; beneath the epithelium is Bowman’s layer. The central corneal stroma is made of collagen and comprises 95% of the corneal thickness. The internal surface of the cornea consists of Descemet’s membrane (the strongest layer of the cornea), which supports the growth of a single cell layer of endothelium. Importantly, the corneal endothelium has no regenerative capacity, and damage leads to corneal edema and loss of vision.
The four types of corneal transplants discussed below include:
- Penetrating keratoplasty (PK)
- Endothelial keratoplasty, of which there are two subtypes:
- Descemet stripping automated endothelial keratoplasty (DSAEK)
- Descemet membrane endothelial keratoplasty (DMEK)
- Deep anterior lamellar keratoplasty (DALK)
- Artificial corneal transplant (keratoprosthesis)
PK is a full-thickness corneal transplant. The ophthalmologist will trephine the patient’s cornea, and the donor cornea will be dissected to fit and placed into the opening. The donor cornea is then sutured into place; these sutures may be removed at a later date. Also known as an “open-sky” technique, since the globe is “open” to the external environment during surgery, PK provides a surgical technique to replace all the layers of the cornea.
DSAEK and DMEK are partial-thickness corneal surgical techniques and involve removing diseased tissue from the posterior lamellar layers of the cornea and replacing them with donor tissue. DSAEK involves the selective removal of the patient’s Descemet membrane and endothelium (approximately one-third of the cornea is removed), followed by transplantation of donor corneal endothelium and corneal stroma. Contrasting with DSAEK, DMEK partial-thickness transplantation is more selective and only adds a new Descemet’s membrane and endothelium without a donor layer of corneal stroma.
Similar to DSAEK and DMEK, SALK and DALK both entail removing the diseased tissue, except these two procedures involve tissue from the anterior corneal layers rather than the posterior. Which procedure you get is determined by the amount of damage there is to the cornea. SALK removes less than one-third of the anterior corneal stroma and is used when the damage is more superficial. DALK is used when the damage goes deeper into the anterior corneal stroma.
Artificial corneal transplant is usually only utilized when previous methods of corneal transplant have not worked. The most commonly used is the Boston Keratoprosthesis, which is a collar button designed keratoprosthesis. The donor corneal tissue is sandwiched between two plates that snap together and are then sutured into the eye.
With all these different options, one can’t help but ask: Which procedure is right for me? What are the success rates of each? For this information, we can turn to public graft registries such as the Australian Corneal Graft Registry (ACGR), the Swedish Corneal Transplant Register (SCTR), and the UK Transplant Registry (UKTR).
Penetrating keratoplasty success rates
For PK, success rates are heavily influenced by the extent of recipient cornea neovascularization as illustrated in ACGR. With no neovascularization, transplant survival rate is approximately 83%; success rate decreases significantly with extensive corneal neovascularization present. It is worth noting that, for common corneal endothelial diseases like Fuchs endothelial dystrophy or pseudophakic bullous keratopathy, a 2015 UKTR analysis did not find that neovascularization was a risk factor for rejection of transplant tissue.
Other host risk factors that adversely impact PK success rates include ocular inflammation and uveitis, concurrent corticosteroid use, and the presence of glaucoma. In eyes with ocular inflammation, the average survival rate of PK transplants at 4 years is 58%. Similarly, the average survival rate of PK transplants at 4 years is 55% when raised intraocular pressure or glaucoma are present. The USA Cornea Disease study reported a 10-year failure rate among 1090 PK procedures of 58%, if there was a history of glaucoma (versus 22% failure rate in the absence of glaucoma). Both of these risk factors are independent of corneal neovascularization for prediction of one-year graft failure.
Endothelial keratoplasty success rates
Recent studies provide evidence that DSAEK or DMEK may have lower rejection rates than PK. In a study that compared outcomes of 200 transplants treating Fuchs endothelial dystrophy, graft rejection was found to be 16% with PK and 5% with DSAEK at two years after transplantation. Moreover, in 168 corneal allografts for secondary bullous keratopathy, the four-year rejection rates for PK and DSAEK recipients were 15% and 4%, respectively.
It is important to note that, as of now, there have been no randomized controlled clinical trials to definitively compare short- or long-term outcomes of DSAEK/DMEK and PK for transplant rejection. Without this level 1 evidence, surgical technique must rely on individualized patient factors to achieve optimal success rates.
Anterior lamellar keratoplasty success rates
A meta-analysis of randomized controlled trials related to DALK for treatment of keratoconus, the merged 1-, 3-, and 5-year graft survival rates were found to be 100% (99.9–100%, P < .001), 92.9% (89.8–95.9%, P < .001), and 90.4% (86.0–0.948%, P < .001), respectively. This meta-analysis supports DALK as a viable option for keratoconus patients who require a corneal transplant. When comparing PK versus DALK, study results show that DALK has a higher overall failure rate than PK; however, postoperative vision rehabilitation is quicker in DALK patients.
Practical considerations
The type of cornea transplantation surgical technique a patient receives is usually decided by their corneal subspecialist ophthalmologist. Individualized patient care involves a multitude of positive and negative risk factors that need to be considered. Depending on the cause and type of disease process, some patients may not be suitable candidates for cornea transplantation, and other methods of treatment should be considered. As with any surgical procedure, corneal transplantation comes with risks. Specifically, corneal transplant immunological rejection, resulting in graft failure, is a lifelong risk with the highest prevalence. To minimize this risk, patients are generally prescribed topical immunosuppressive eye drops for at least a year following the surgery. Other common risks associated with corneal transplant procedures include glaucoma, endophthalmitis, wound leakage, and retinal detachment.
Future of corneal transplants
The main advancement in the field of corneal transplant in recent history has been the use of thinner lamellar slices of tissue for DSAEK and DMEK procedures. But for those patients who are unable to have surgery, an exciting new development - as of June 2020 - involves LiQD Cornea, which is an alternative to conventional corneal transplantation and sealants.
Before LiQD Cornea, corneal perforation was treated with cyanoacrylate glue, with possible cytotoxic effects requiring transplantation. LiQD Cornea is a self-assembling, fully defined, synthetic collagen analog that is less costly than human recombinant collagen and reduces the risk of immune reactions. It gelatinizes within five minutes of application, so the procedure can be performed in an outpatient clinic as opposed to an operating room. While these findings are indeed exciting and promising, comparative and long-term studies are needed for a valid comparison of LiQD Cornea to traditional corneal transplants techniques.
References
- Armitage, W John, et al. “High-Risk Corneal Transplantation: Recent Developments and Future Possibilities.” Transplantation, Lippincott Williams & Wilkins, Nov. 2019.
- Boyd, Kierstan. “Corneal Transplant Surgery Options.” American Academy of Ophthalmology, 17 Sept. 2020.
- Figueiredo, GS, et al. “Transplant Rejection Following Endothelial Keratoplasty and Penetrating Keratoplasty in the United Kingdom: Incidence and Survival.” American Journal of Ophthalmology, U.S. National Library of Medicine, June 2015.
- Guan, Meng, et al. “Graft Survival Rate of Deep Anterior Lamellar Keratoplasty for Keratoconus: A Meta-Analysis.” Medicine, Wolters Kluwer Health, July 2018.
- Hjortdal , J, et al. “Graft Rejection and Graft Failure after Penetrating Keratoplasty or Posterior Lamellar Keratoplasty for Fuchs Endothelial Dystrophy.” Cornea, U.S. National Library of Medicine, May 2013.
- Jones MNA, Armitage WJ, Ayliffe W, et al. Penetrating and Deep Anterior Lamellar Keratoplasty for Keratoconus: A Comparison of Graft Outcomes in the United Kingdom. Invest Ophthalmol Vis Sci, Dec. 2009
- McTiernan, Christopher D et al. “LiQD Cornea: Pro-regeneration Collagen Mimetics as Patches and Alternatives to Corneal Transplantation.” Science Advances, June 2020.
- Pedersen , IB, et al. “Graft Rejection and Failure Following Endothelial Keratoplasty (DSAEK) and Penetrating Keratoplasty for Secondary Endothelial Failure.” Acta Ophthalmologica, U.S. National Library of Medicine, Aug. 2012.
- Singh, R, et al. “Corneal Transplantation in the Modern Era.” The Indian Journal of Medical Research, U.S. National Library of Medicine, July 2019.
- Sugar A, Gal RL, et al. ; Writing Committee for the Cornea Donor Study Research Group “Factors Associated with Corneal Graft Survival in the Cornea Donor Study.” JAMA Ophthalmol., March 2015.
- Tourkmani AK, Sánchez-Huerta V, De Wit G, et al. “Weighing of Risk Factors for Penetrating Keratoplasty Graft Failure: Application of Risk Score System.” Int J Ophthalmol, March 2017.