Though it makes up the majority of the volume of the globe, the vitreous body is often overlooked in our daily clinical lives. As the vitreous ages, the gel-like structure begins to liquify, while the vitreoretinal adhesion begins to weaken. This degenerative process eventually culminates in the extremely common posterior vitreous detachment, often accompanied by acute floaters and photopsias. In a subset of patients, an incomplete or anomalous posterior vitreous detachment will occur. This persistent vitreoretinal attachment can lead to vitreomacular traction which is characterized by foveal contour irregularity, pseudocyst formation, and/or foveal detachment. In mild cases, patients are often asymptomatic but more advanced cases can develop blurred vision, metamorphopsia, or central photopsias.
Welcome to Diagnostics & Imaging Monthly, a new column from Daniel Epshtein, OD, FAAO! This column will cover diagnostics and imaging of the anterior and posterior segment and will share both basic and advanced educational tips to help optometrists and ophthalmologists.
While you're waiting for the next column, check out these articles:
Cross-sectional epidemiological studies have estimated the prevalence of vitreomacular traction, as identified by OCT, to be 1.6%.
1 I specifically quote the prevalence as identified by OCT, because vitreomacular traction is often difficult to diagnose clinically. In fact, I frequently diagnose vitreomacular traction incidentally while managing other macular conditions such as
age-related macular degeneration or macular edema. Because vitreomacular traction is difficult to diagnose with funduscopy, it is important to remember that the prevalence of vitreomacular traction increases with age and in eyes that have undergone surgery, trauma, or significant myopic elongation. It is important to keep a high level of suspicion in these patients and acquire an OCT image to visualize the vitreomacular interface.
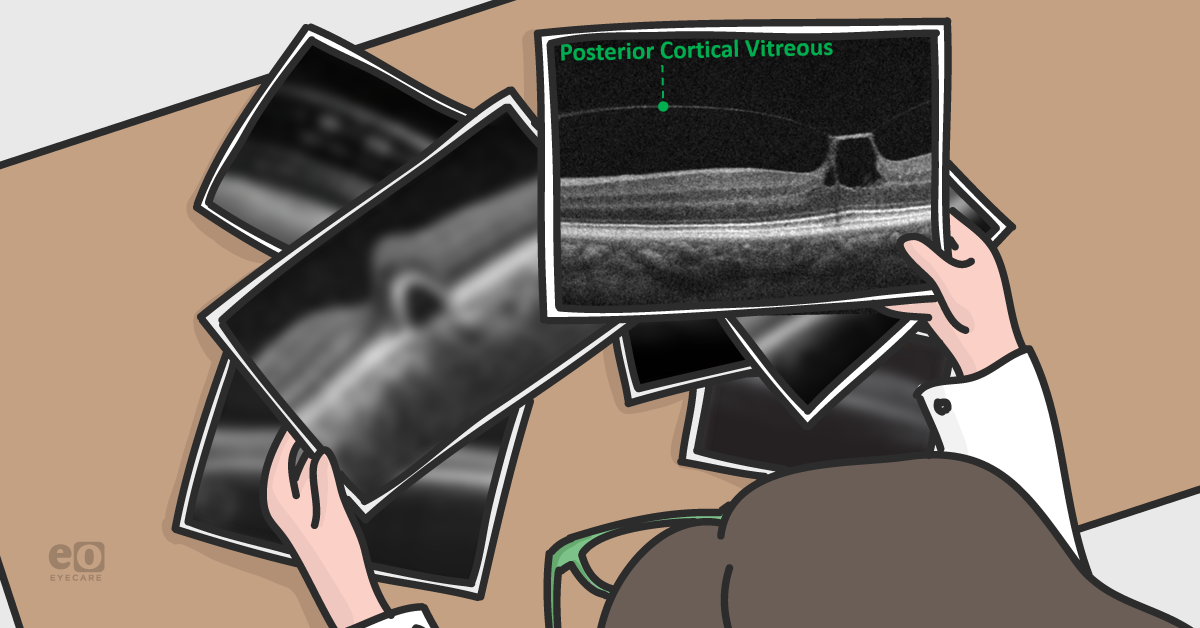
Figure 1: The posterior cortical vitreous has pulled away from the retina but is tightly bound at the fovea leading to vitreomacular traction.
As in figure 1, the posterior cortical vitreous will be mostly detached from the retinal surface but the persistent vitreoretinal attachment will cause disruptions in the retinal architecture. Vitreomacular traction is classified as either focal (≤1500 μm) or broad (≥1500 μm) and isolated or concurrent depending on the presence or lack thereof comorbid retinal disease.2 Progressive vitreal degeneration can lead to spontaneous resolution or development of a full thickness macular hole. Small scale OCT-based longitudinal studies have noted that 26%-43% of isolated vitreomacular traction cases will resolve spontaneously.3,4 For this reason, observation is often recommended in cases of isolated vitreomacular traction, especially in patients with mild subjective complaints. In persistent or complicated cases, pharmacological vitreolysis, pneumatic vitreolysis, or vitrectomy can be performed.
In mild cases like figure 1, where the outer retinal is intact, visual acuity will usually be in 20/25 range and these patients can be monitored in 1-2 months after initial diagnosis. The follow up interval can be gradually lengthened based on symptoms and risk factors. Cases that are monitored should have repeat
OCT imaging to evaluate the vitreoretinal changes, as visual acuity may be relatively stable even as this condition progresses to early hole formation. Special cases of vitreomacular traction, such as monocular patients or patients with a full thickness macular hole in the other eye should be monitored more often or referred to a retinal specialist to consider intervention. My threshold for referral to a retinal specialist is lower in these high-risk patients because full thickness macular hole is a devasting outcome that can occasionally be avoided with lower risk surgical interventions such as pharmacological or pneumatic vitreolysis.
Figure 2: OCT image of vitreomacular adhesion. Note the posterior cortical vitreous pulling away from the retina without altering the retinal architecture.
Theoretically, every eye that undergoes posterior vitreous detachment will go through a phase of vitreomacular adhesion. This is a state where the posterior cortical vitreous has separated from the retina but no alteration in the retinal structure is appreciated. Vitreomacular adhesion can be thought of as a normal phase of the vitreoretinal relationship and no intervention is thought to be necessary. As with vitreomacular traction, vitreomacular adhesion can be classified as either focal (≤1500 μm) or broad (≥1500 μm) and isolated or concurrent depending on the presence or lack thereof comorbid retinal disease.2
Vitreomacular traction and vitreomacular adhesion are two relatively common findings as visualized by OCT, with a combined prevalence of 40%.
5 Both are difficult to discern clinically, but readily identified with OCT. Observation is often initially favored, but management is dictated by visual acuity, symptoms, OCT findings, and risk of full thickness macular hole formation. In the next issue, we will delve into the world of
macular holes in all its forms; full thickness, lamellar and pseudo.
Resources
- Meuer, Stacy M., et al. "The epidemiology of vitreoretinal interface abnormalities as detected by spectral-domain optical coherence tomography: the beaver dam eye study." Ophthalmology 122.4 (2015): 787-795.
- Duker, Jay S., et al. "The International Vitreomacular Traction Study Group classification of vitreomacular adhesion, traction, and macular hole." Ophthalmology 120.12 (2013): 2611-2619.
- Dimopoulos, Spyridon, et al. "Rate and timing of spontaneous resolution in a vitreomacular traction group: Should the role of watchful waiting be re-evaluated as an alternative to Ocriplasmin therapy?." British Journal of Ophthalmology 99.3 (2015): 350-353.
- Theodossiadis, George P., et al. "Spontaneous resolution of vitreomacular traction demonstrated by spectral-domain optical coherence tomography." American journal of ophthalmology 157.4 (2014): 842-851.
- Rodman, Julie A., et al. "Prevalence of vitreomacular adhesion in patients without maculopathy older than 40 years." Retina 38.10 (2018): 2056-2063.
We have a direct partnership with ZEISS!