Astronomer Horace Babcock first proposed the concept of adaptive optics (AO) in 1953 to help capture structures in space in sharper detail. The first steps towards applying this technology to the human eye started with Dreher et al., 1989 who used a deformable mirror (DM) to give static correction of
astigmatism in a scanning laser ophthalmoscope (SLO). A few years later, Liang et al., 1997 used the Hartmann-Shack wavefront sensor in conjunction with a deformable mirror to reduce optical aberrations and produce some of the first in-vivo images of the cone receptors.
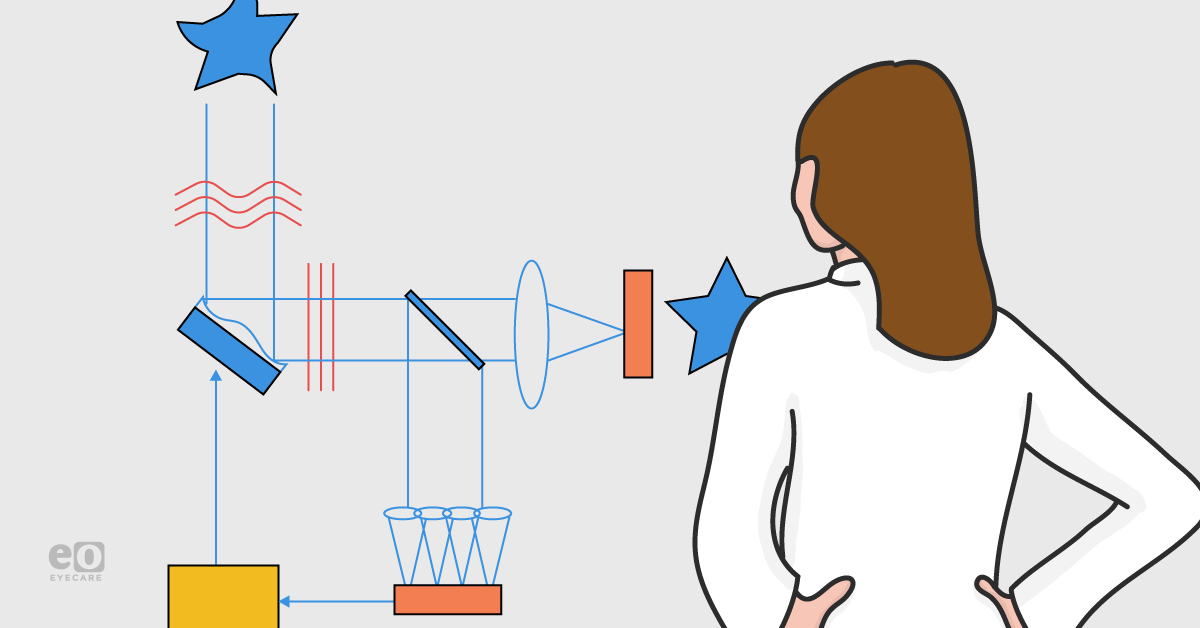
Adaptive optics is not an imaging modality by itself but rather a technology used in conjunction with other
imaging modalities to improve their performance. AO measures and corrects ocular aberrations in real-time using wavefront sensors and shaping modules (Figure 1). The resolution is unprecedented (approximately 2-3 microns) and can resolve individual cells (Figure 2).
Figure 1: Schematic representation of adaptive optics imaging with Hartmann-Shack wavefront sensor taken by Gill et al., 2019.
Figure 2: One of the first documented images of cones in the cross-section view of the foveal region without adaptative optics (a) and with adaptive optics (b) (Liang et al., 1997).
Adaptive optics instrumentation
Adaptive optics fundus imaging
The first AO used for eye imaging was coupled with a high magnification fundus camera with a wavefront sensor and deformable mirror (Figure 3). This instrumentation allowed for the first extensive analysis and imaging of photoreceptors and vasculature. An advantage of the AO-Fundus technology is that eye movement minimally affects the image because it has millisecond capture times. However, it is hard to filter scattered light and, therefore, the latter reduces image quality (this was later improved upon in the AOSLO discussed below).
Figure 3: Schematic drawing of adaptive optics fundus instrument (Parthasarathy et al., 2017).
Adaptive optics scanning laser ophthalmoscope (AOSLO)
AO was later combined with scanning laser ophthalmoscopy (SLO) which improved upon the optics of the AO-Fundus instrument to eliminate the scattered light by utilizing a confocal pinhole addition (Figure 4). This enabled the user to control the amount of light returning from the retina, emphasizing specific structures of the retina that they wanted to study more closely. A disadvantage of this design is that researchers are unable to capture a 3D image, only 2D. This was later solved in the AO-OCT model.
Figure 4: Schematic representation of the AOSLO instrumentation with the confocal pinhole adaptation (Roorda et al., 2010).
Adaptive optics optical coherence tomography (angiography) AO-OCT/ AO-OCTA
AO has recently been coupled with the
new technology of OCT and OCTA. The AO-OCT and AO-OCTA are the first combinations with adaptive optics to produce three-dimensional images by combining both lateral resolution from the AO and axial resolution from the OCT. The AO-OCT allows for high-resolution images of photoreceptors and cellular structures in the retina (Figure 5). The AO-OCTA can enable researchers to capture retina vasculature and even individual blood cell movement within vessels.
Figure 5: Schematic drawing of the adaptive optics and optical coherence tomography instrument (Miller et al., 2011).
Adaptive optics and eye imaging
Currently, the major adaptive optics instrumentation used is AOSLO, AO-OCT, and AO-OCTA. With these three types of imaging techniques, researchers can identify the structures of a healthy eye and study several clinical conditions, including age-related macular degeneration (AMD), hereditary retinal dystrophies, optic neuropathies, and diabetes.
Photoreceptors
AO-OCT is currently used to capture healthy cones for normative database use and disruption in cones from retinal diseases. For example, Chui et al., 2008b found that beyond two degrees of retina eccentricity, all quadrants of the retina (except between disc and fovea) increase cone spacing with increased eye length. This could be useful to detect and monitor eye growth in young patients in the future.
A study by Tumahai et al., 2008 measured cone density in various ages in healthy eyes and found that perifoveal cone density significantly decreases with age whereas cone spacing increases (FIGURE 6). This is essential information to create a normative database to compare with unhealthy eyes in clinical trials.
Figure 6: AO-OCT is able to measure perifoveal cone density in various ages. With increasing age, cone density decreases and cone spacing increases (Tumahai et al., 2008).
Retinal vasculature
Retinal blood vessels can potentially serve as biomarkers to identify and monitor systemic diseases like hypertension and diabetes. Researchers currently use AO-OCTA to monitor vessel caliber, vascular perfusion, blood velocity, and blood flow without invasive techniques such as intravenous
fluorescein angiography. The level of resolution of the foveal avascular zone (FAZ) is strikingly different with OCTA only versus AO-OCTA (Figure 7).
Figure 7: Adaptive optics allows for much higher resolution image acquisition of retinal vasculature. The red line demarcates OCTA imaging of FAZ without adaptive optics on the left side compared with adaptive optics on the right side (Burns et al., 2019).
Furthermore, AO-OCTA can study changes in perfusion in capillaries over time in patients with diabetes or hypertension (Figure 8). This imaging technology can allow practitioners to identify diabetic changes before they appear on fundus photography, allowing treatment to be implemented earlier.
Figure 8: Microscopic changes to retinal vasculature in a patient with diabetic retinopathy. The left image with the square shows the area of the fundus that was subsequently imaged with AO-OCTA. The AO-OCTA image shows black arrows which point to areas of abnormal vessel walls and white arrows which point to areas of nonperfused capillaries (Burns et al., 2019).
Retinal degeneration
Scanning laser ophthalmoscope near-infrared reflectance (SLO NIR) technology captures geographic atrophy using traditional fundus photography; contrastingly, AO with fundus photography demonstrates areas of hyporeflective clumps throughout the retina (Figure 9).
Figure 9: Far left image demonstrates area of geographic atrophy with regular scanning laser ophthalmoscope fundus photography. The middle image shows the same area of geographic atrophy captured with adaptive optics and fundus photography. The right image shows a magnified view of middle image (Gocho et al., 2013).
Researchers have also looked at drusen changes in AMD. A study by Johnson et al., 2003 found that photoreceptors overlying both soft and hard drusen exhibit structural and molecular abnormalities. This suggests that photoreceptor cell function is compromised secondary to drusen formation (Figure 10).
Figure 10: Adaptive optics imaging showing drusen (asterisk) pushing up on outer segments of cones above, resulting in cone disruption. Johnson et al., 2003.
It is unclear which tissue is affected first in
AMD. AO studies can potentially help identify the time and sequences in which tissues are affected. Furthermore, AO can be used to look at cone photoreceptor density in various
inherited retinal diseases, such as Stargardt’s and retinitis pigmentosa.
Retinal nerve fiber bundles
Early detection of axonal tissue loss is critical for managing diseases that destroy the retinal nerve fiber layers (RNFL), such as
glaucoma. AO-OCT allows us to identify RNFL bundles which demonstrates the spacing between bundles (Figures 11 and 12). AO can measure thickness and width variations of individual RNFL bundles between normal, aging, and diseased retinas.
Figure 11 shows cross-section of various layers in retina using AO-OCT. (Miller et al., 2011).
Figure 12 shows the spacing between RNFL clearly defined with AO-OCT (Miller et al., 2011).
One study by Zwillinger et al., 2016 assessed the morphology of the human lamina cribrosa pores in healthy and primary open-angle glaucoma eyes. They concluded that, on average, the lamina cribrosa pores are more elongated and fused in POAG eyes compared to healthy eyes (Figure 13).
Figure 13 shows pores of lamina cribosa in healthy patients versus bottom image revealing enlarged and fused pores in patients with open angle glaucoma (Zwillinger et al., 2016).
Limitations of adaptive optics
Adaptive optics is a novel technology that allows us to image structures at a microscopic level. However, there are some limitations to this imaging technique. For example, optical medical densities/abnormalities such as dry eye, cataracts, vitreous debris, and corneal scarring can impact the quality of the image. Furthermore, sizeable uncontrolled eye movements can disrupt the image. When capturing images with AO, the field of view is very narrow, which makes this process time-consuming. Lastly, before we understand retinal disease and its effect on cellular structures, normative databases need to be established and clinicians trained in interpreting these images.
Future of adaptative optics
Researchers are continuing to improve upon the resolution and speed of image capture. Miller et al., 2011 was able to acquire the first four-dimensional images of cones using an ultra-high resolution (UHR)-AO-OCT and CMOS (complementary metal-oxide semiconductor) device (FIGURE 13). This technique has improved resolution to a fraction of a cone width, and images are acquired six to eight times faster than a commercial OCT. In the future, adaptive optics could prove helpful in clinical trials of stem cell and gene therapies and demonstrate capability in monitoring the progression of various ocular diseases at a cellular level.
FIGURE 14: Imaging of cone receptors using UHR-AO-OCT at 0.5, 1.5, 3, and 6 degrees temporal to the fovea of a healthy subject (Miller et al., 2019).
References
- Burns SA, Elsner AE, Sapoznik KA. Adaptive optics imaging of the human retina. Prog Retin Eye Res. 2019 Jan;68:1–30
- Chui, T.Y.P., Zhong, Z.Y., Burns, S.A., 2011. The relationship between peripapillary crescent and axial length: implications for differential eye growth. Vis. Res. 51, 2132–2138
- Dreher AW, Bille JF, Weinreb RN. Active optical depth resolution improvement of the laser tomographic scanner. Appl Opt 1989; 24: 804–808.
- Gill, J.S., Moosajee, M. & Dubis, A.M. Cellular imaging of inherited retinal diseases using adaptive optics. Eye 33, (2019) 1683–1698.
- Gocho K, Sarda V, Falah S, Sahel J-A, Sennlaub F, Benchaboune M, et al. Adaptive optics imaging of geographic atrophy. Investigative Ophthalmol Vis Sci. 2013;54:3673–80
- Johnson PT, Lewis GP, Talaga KC, Brown MN, Kappel PJ, Fisher SK, et al. Drusen-associated degeneration in the retina. Invest Ophthalmol Vis Sci. 2003;44:4481
- Liang J, Williams DR, Miller DT. Supernormal vision and high-resolution retinal imaging through adaptive optics. J Opt Soc Am A Opt Image Sci Vis. 1997 Nov;14(11):2884-92.
- Makiyama Y, Ooto S, Hangai M, Takayama K, Uji A, Oishi A, Ogino K, Nakagawa S, Yoshimura N. Macular cone abnormalities in retinitis pigmentosa with preserved central vision using adaptive optics scanning laser ophthalmoscopy. PLoS One. 2013 Nov 19;8(11):e79447
- Miller, D., Kocaoglu, O., Wang, Q. et al. Adaptive optics and the eye (super resolution OCT). Eye 25, 321–330, 2011
- Roorda A. Applications of adaptive optics scanning laser ophthalmoscopy. Optometry and Vision Science : Official Publication of the American Academy of Optometry. 2010 Apr;87(4):260-268.
- Parthasarathy, Mohana & Lakshminarayanan, Vasudevan. A Brief History of Aberrometry Applications in Ophthalmology and Vision Science. (2017) 10.1007/978-981-10-3908-9_4.
- Tumahai P, Moureaux C, Meillat M, Debellemaniere G, Flores M, Delbosc B, et al. High-resolution imaging of photoreceptors in healthy human eyes using an adaptive optics retinal camera. Eye (Lond). 2018;32:1723–30
- Zwillinger S, Paques M, Safran B, Baudouin C. In vivo characterization of lamina cribrosa pore morphology in primary open-angle glaucoma. J Fr Ophtalmol. 2016;39:265–71